Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Mert Saynak*1, Dilek Nurlu1, Funda Cukurcayir2, Gorkem Turkkan3 and Sernaz Uzunoglu4
Received: March 26, 2018; Published: April 12, 2018
*Corresponding author: Mert Saynak, Department of Radiation Oncology, Trakya University Hospital, 22030, Edirne, Turkey
DOI: 10.26717/BJSTR.2018.03.000955
Abbreviations: ChT : Chemotherapy; RT: Radiotherapy; pCR: Complete Response; MRI: Magnetic Resonance Images; PET: Positron Emission Tomography; CT: Computed Tomography
Most people with locally advanced rectal cancer are treated with chemotherapy (ChT), radiotherapy (RT), and surgery. With improved surgical techniques and the addition of neoadjuvant RT+ ChT, 5-year local recurrence rates have decreased from >25% to <10% [1,2]. Regarding to local/regional disease site, quality of life is a new and increasingly important goal for rectal cancer treatment. However, these advances have not appreciably decreased the risk of distant metastatic recurrence (approximately 30%), which remains the leading cause of rectal cancer-related death. That's why, systemic treatment to control distant microscopic disease especially has become increasingly importance in recent years.
Preoperative radiotherapy has an accepted role in reducing the risk of local recurrence in locally advanced rectal cancer, particularly when the circumferential resection margin is breached or threatened. There are several reports about patients who have neoadjuvant ChRT and surgery is not tolerating well the adjuvant chemotherapy. Whereas, the consolidation chemotherapy strategy has the potential to increase local disease control and distant control with relatively good treatment compliance. We would like to glance at pros and cons about total neoadjuvant treatment and nonsurgical treatment in this paper.
Neoadjuvant chemo radiotherapy (ChRT) has the potential benefit to improve of local disease control. Besides it may provide significant tumor downsizing and down staging and results in pathological complete response (pCR) in —15-30% of the cases [3]. The data that have been accumulated so far show that, patients who achieved pCR after CRT have better long-term outcomes, less propensity to develop local and distal recurrence, and improved survival [1]. One assumption proposed to explain this issue suggests those cases with pCR have relatively early stage and small disease initially. Another explanation is that obtaining a complete response in the local disease with CRT may indicate that the tumor is sensitive to ChT, indicating that it may be a controlled systemic disease. Total neoadjuvant therapy can be designed as chemotherapy followed by RT (+ ChT) in order to prolong the waiting period until surgery. Thus, by this treatment method, response probability can be increased for a couple of reason:
a. Longer waiting period and
b. Additional chemotherapy courses through this waiting period.
According to the data obtained from several prospective, singlearm studies that had >90% consolidation ChT completion rates [4,5]. Several ways have been tried to increase the likelihood of providing tumor response. One approach is to lengthen the interval between ChRT and surgery, because it has been proven that pCR is time-dependent. French study (Lyon R90-01) demonstrated that >6 weeks after RT has better response outcomes [5,6]. Actually, optimal time to surgery is still debated. A couple of randomized studies were carried out to compare 6 vs 12 weeks and 7 vs 11 weeks after ChRT. As a result, 12 weeks waiting period looked better than 6 weeks for pCR, but 7 and 11 weeks had similar pCR rates with higher surgical morbidity [7]. As the time to surgery increases, the concern that RT will cause an increase in late effects, which will increase the morbidity of the surgical procedure, has not been confirmed in other studies conducted in this area [8]. The second is the integration of different systemic treatment schemes into preoperative radiotherapy. Disappointingly, the addition of oxaliplatin to standard concurrent ChRT protocol was shown to increase toxicity risk without improving tumor response in most of the phase III randomized studies [9-11].
Only the German study showed an improvement in pCR in an unplanned exploratory analysis [12]. Duke University reported encouraged results with four cycles of bevacizumab infusion concurrently with 50.4 Gy RT and two cycles of 24-hour continuously infused 5-fluorouracil. In their phase I/II clinical study of 32 patients, they showed that 100% local control with this treatment schema [13]. Retrospective studies imply brachytherapy boost may improve the response possibility [14,15]. Besides the Lyon R96.02 Randomized Study demonstrated if contact 50 kilovolt X-ray treatment was administered in addition to external RT, the probability of pathologic complete response and in 10 years' follow-up, colostomy-free survival was increased [16]. If brachytherapy is administered alone without external radiotherapy, it is disadvantageous that the mesorectal lymph nodes receive an insufficient dose, and even that the lateral lymph nodes receive almost no dose. As systemic treatment options progress, brachytherapy may play a more central role in the treatment of rectal cancer.
Another strategy for obtaining tumor response is to administer additional ChT during the waiting period between ChRT and surgery One study demonstrated that 3 additional cycles FOLFOX after standard ChRT with fluoroprimidin-based ChT improved tumor response. In this prospective study, 34 patients with rectal cancer underwent 5-fluorouracil-based chemotherapy every 21 days in totally six cycles. The authors concluded, although in a preliminary basis, that the addition of chemotherapy after ChRT during the resting period (also known as "consolidation" chemotherapy) resulted in considerably high rates of complete response [17]. Recently, a study reported from United States, in which the primary study endpoint was the pCR rate. Remarkably, pCR rates increased significantly with additional cycles of FOLFOX between ChRT and surgery, with 38% of patients achieving pCR when 6 cycles of ChT were given after CRT (compared with an 18% pCR rate for patients who did not receive ChT between CRT and surgery) [18].
The Polish Colorectal Study Group conducted a phase III randomized study including 515 patients with unrespectable locally advanced rectal cancer (stage cT3 or cT4) to compare the results of short and long course RT schemas. In the control arm, patients received radiotherapy at 50.4 Gy given concurrently over approximately 5 weeks with bolus fluorouracil (5-FU) and leucovorin during the first and fifth weeks, plus oxaliplatin at 50 mg/m2 once weekly. The patients in experimental arm received 5 x 5 Gy RT followed by three cycles of FOLFOX4 (5-FU, leucovorin, oxaliplatin) every 2 weeks. R0 resection, the primary endpoint, was achieved in 77% of the experimental arm and 71% of the control arm (p= 0.07), indicating a trend in favor of the short-course approach. Pathologic complete responses were achieved by 16% and 12%, respectively (p = 0.17) [19]. The results of a phase II randomized trial, in which the efficacy of ChT with bevacizumab in the waiting period after ChRT is tested, are expected to understand the rationale for the non-surgical treatment approach be released soon [20].
The Korean Society of Coloproctology (KONCLUDE Study) has started a prospective randomized study to evaluate additional 3 cycles of chemotherapy consisted with FOLFOX regimen between neoadjuvant ChRT and surgery. Their expectance that this treatment approach could increase the proportion of pathologic complete response (pCR), subsequently could show better oncologic outcomes [21]. Similarly, impressive treatment compliance rates have been observed in studies using the second total neoadjuvant treatment paradigm-induction ChT followed by ChRT and then surgery. However, there is not so much high level evidence about superiority of this approach [22-25]. On the other hand, some patients initially have obstruction and hemorrhagic findings due to big tumors. That's why, starting with RT instead of systemic therapy alone, may provide a kind of early palliation theoretically and performing chemotherapy before the surgery instead of postoperative period improves patient compliance to systemic therapy, and increased tumor response probability. The recommended treatment strategy is shown diagrammatically in (Figure 1).
Figure 1: The recommended treatment treatment strategy is shown diagrammatically.
Note: RT: Radiotherapy, Cht: Chemotherapy, Brachy: Brachytherapy
It's clear that patients treated using non-surgical approach because of achieved complete tumor response is avoided from the risk of surgical mortality and morbidity on urinary, fecal and sexual functions. The studies have been published so far showed that, the oncologic outcome after non-surgical approach was comparable with that of patients with a pCR after surgery, but functional outcome was significantly better [26,27]. Long term results of non-surgical approach have been firstly reported by Brazilian investigators. A total of 99 patients had a sustained cCR for > 1 year and managed non-surgically. They reported 13 recurrences (13%) and 5 isolated recurrences were effectively salvaged at a mean 60 months' follow-up. They reported that 5 isolated endorectal recurrences were effectively salvaged. In the end, 5-year overall survival and disease-free survival rates were 93% and 85%, respectively [26]. Researchers in Holland initiated a prospective study. Twenty-one patients with cCR were managed non-surgically. As a result, only one patient developed end luminal recurrence and underwent surgical salvage [27]. Recently, a propensity matched cohort study(the OnCoRe (Outcomes after Clinical Complete Response in Patients with Rectal Cancer)) study evaluating non- surgical treatment have been published from United Kingdom. 259 patients were included of which 228 underwent surgery. Although this sounds like a potentially attractive option, only 12% (31 of 259) of the patients in this study experienced a complete response. As a result, there was no difference between the matched paired groups [28].
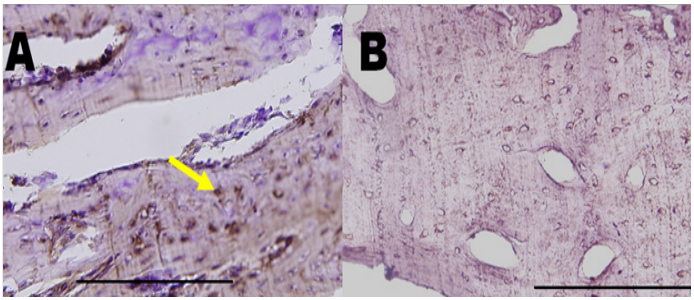
Unfortunately, major clinical response is not easy to define and not truly reliable in predicting pathological complete response (pCR). There is a difficulty to distinguish between tumor and fibrosis on magnetic resonance images (MRI) taken for restaging. Positron emission tomography (PET) is advantageous over computed tomography (CT) and MRI in that the latter two imaging modalities are often limited in differentiating post-treatment fibrosis from residual or recurrent tumor. Detection of residual tumor cell clusters using non-surgical methods is still not entirely possible. In the group of patients who underwent surgery after ChRT, 25-77% of patients with clinical complete response (cCR) had pCR [29-31]. At the current time, using the latest available imaging diagnostic techniques, we still have always a risk of misdiagnosing about 1520% with the most optimistic estimation in identifying pCR.
Question about the way in which patients who has achieved a true pCR to identify with precision is still being evaluated. Some clinicians suggest full thickness local excision for this patient group with cCR. The arguments of this approach are, it can be a treatment of residual disease at a certain level and can be helped to define pathological response as good as 99% for T stage. However, complete response of the primary tumor cannot predict response in regional lymph nodes, which are involved in 7 to 17% of patients who have cCR of the primary tumor [32]. Theoretically, anastomosis problems may constitute a potential disadvantage of this approach compared to non-surgical treatment. The 45-54 Gy dose is lower than the curative dose used by radiation oncologists in other diseases like head and neck cancers, lung cancers, endometrial and cervical cancers. There are some question marks about the progression-free time that the dose in question can provide. In the studies evaluated non-surgical approach has been used long- course radiotherapy.
Both the Dutch and Swedish rectal cancer studies used neoadjuvant short-course radiotherapy in 5 x 5 Gy and patients typically underwent surgical resection within 1 week ofradiotherapy completion. This approach looks effective to reduce local recurrence risk but in the past tumor regression was not primary aim of short course radiotherapy. However, the Poland Group conducted a prospective randomized study and demonstrated that 5 x 5 Gy followed by 3 cycles of FOLFOX and relatively long time waiting to surgery provides similar response with long course ChRT [19]. In rectal cancer population there is a kind of nasty local recurrence shape which may be involved to sacral nerves and attached to sacral bone. Even when the mesorectal is removed by performing total mesorectal excision, presacral region is the most important local recurrence site. Since the tumor cells can easily progress through sacral nerves into the sacral bone. This is a kind of nightmare for the clinicians.
Because it's a very painful clinical manifestation for the patient and surgical salvage is highly difficult in many such cases. Even though impressive initial study results with non-surgical approach reported by Brazil and Holland, local recurrence rate may be reach about 25%. However, local recurrences can be salvaged successfully if the close follow-up strategies are applied [33]. In relatively early stages, small tumors like small T3 a,b N0 disease, complete response may more possible than relatively more advanced stages like T4 and lymph node(s) clinically positive disease. However, for the T3a,b disease the recent wisdom for the management of rectal cancer treatment if TME is achievable, recommends surgery initially. Because postoperative ChRT could be selectively used in such patients [34] Therefore, the patient group that is more likely to achieve complete response with neoadjuvant therapy will not have received ChRT for this purpose.
In today’s modern era, it is clear that the common standards for large heterogeneous patient groups need to be replaced by more individualized therapies. Non-surgical treatment for complete responders after ChRT for rectal cancer should be based on strict selection and follow-up with endoscopy and up-to-date imaging may be practicable. Even so, the decision to undergo to surgery is up to patients' willingness. Patients should be informed that non-surgical approach remains unproven yet31. If a patient who had clinical CR volunteers to accept some risk to postpone rectal surgery in hope of avoiding major surgery and preserving rectal function can be taken a close follow-up protocol. The effective and safe implementation of this approach requires a multidisciplinary approach and very close cooperation between these different disciplines.
For many years the primary focus of rectal cancer treatment has been local/regional pelvic disease control. With current surgical methods and modern advanced techniques, the risk of local recurrence has been reduced to less than 10%.Thus reducing the risk of developing distant metastases and increasing the quality of life of surviving patients should be new aims of treatment. Theoretically, the patients who have the increased cCR provided by "prolonged waiting time and extra chemotherapy courses" will have the option of follow-up without surgery. This approach may allow for non-surgical treatment and so may save the patients from the comorbidities associated with surgical intervention. Besides, even if resection is to be done, completion of ChTprior to surgery can also ensure that patients complete the ChT regimen. Of course; these theoretical assumptions should be supported by phase III randomized study results.


