Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Laila A AlBishi*
Received: March 01, 2018; Published: March 20, 2018
*Corresponding author: Laila A AlBishi, Department of Pediatric, Assistant Professor Pediatric Endocrinologist, Pediatric department, Faculty of Medicine, University of Tabuk, Saudi Arabia
DOI: 10.26717/BJSTR.2018.03.000873
Abbreviations: VT: Visceral Fat; VAT: Visceral Adipose Tissue; IR: Insulin Resistance; MetS: Metabolic Syndrome; T2DM: Type 2 Diabetes Mellitus; BMI: Body Mass Index; LDL: Low Density Lipoprotein; SCFA: Short Chain Fatty Acids; ITF: Inulin-Type Fructan; FOS: Fructo Oligopolysacchrides; PYY: Peptide YY; RCT: Randomized Clinical Trials; GLP-1: Glucagon like Peptide-1; HDL: High Density Lipoprotein; BW: Body Weight
Undoubtedly, obesity has become a global public health problem particularly when looking at the obesity-related diseases. Over the past 20 years, studies explored greatly the role of fat tissue in obesity pathogenesis suggesting that the functional differences between visceral fat adiposity (VFA) and subcutaneous fat adiposity (SFA) impacted the appearance of many obesity-related diseases. Therefore, increased knowledge about VFA and SFA could promote the development of more effective therapies against several obesity- related problems. The role of modulating gut microbiota with fiber- diet (prebiotics) in attempt to reduce VFA is nowadays an era of interest to treat obesity. Prebiotics constitute a selective stimulation of growth/activity of certain microbial species in the gut microbiota that offer health benefits to the host [1]. Consequently, its use as a dietary intervention provides a novel therapeutics in obesity and cardio-metabolic disease risk [2]. These mini-review summaries the current evidence linking a specific dietary-fiber called inulin to the reduction of VFA.
Figure 1: Mechanisms of insulin-type fructans in decreasing lipid profile.
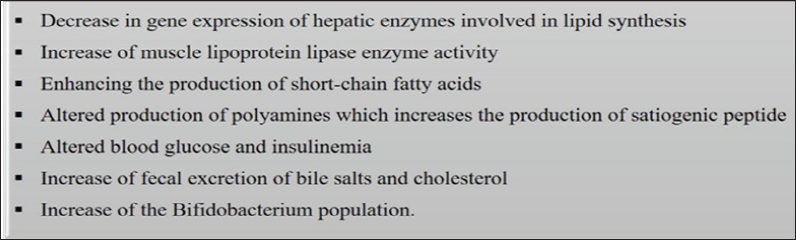
Inulin is a chicory root fiber that also found in onions, garlic, wheat, artichokes and bananas. It is a polymer of fructose monomers that is indigestible but soluble fiber. The estimated daily consumption ranges between 3-11 grams in Europe and 1-4 grams in the United States [3]. Studies demonstrated several physiological functions of inulin such as modulation of lipid metabolism in the liver and muscle. Reis et al. explained the main mechanisms of inulin-type fructans in the improvement of lipid profile, thus reducing the cardiovascular risk [4] (Figure 1). As the diet considered a strong contributor to the structural microbial changes [5], a prebiotics such as oligofructose (a subgroup of inulin) may affect the structural composition of the intestinal microbiota following high-fat diet feeding, thus improving the parameters of metabolic inflammation [6].
Interestingly, Cani [6,7] demonstrated that oligofructose consumption resulted in increased satiety and accompanied by a decrease in total energy intake in adults. This is explained by the presence of short chain fatty acids (SCFA) and their ability to increase appetite suppressing hormones such as glucagon-like peptide 1 (GLP-1) [7]. A large intestinal microflora fermentation facilitated a reduction in serum cholesterol and low density lipoprotein (LDL) levels 'important risk for coronary heart disease', [8] consequently, inulin found to exist a role in the stimulation of bifid bacteria growth "probiotics" [9].
VF is a type of adipose tissue which has an important implication for metabolic health [10]. Interestingly, VF is highly heritable and showed significant associations with the fecal microbiota. According to Beaumont et al, studies linked increased abdominal adiposities using body fat distribution measures such as waist/ hip ratio, to fecal microbiome profiles in which specific probiotic consumption reported to lower VF. The authors suggested that VF mass plays a major role in the components of central adiposity or 'cardio-metabolic disease risk' [11]. More importantly, the presence or absence of a microbial flora regulates insulin sensitivity and cholesterol metabolism [12]. According to Tilg and Kaser, evidence indicated that type 2 diabetes mellitus (T2DM) negatively affect the structural composition of the microbiota (Bacteroidetes) which if decreased, the metabolic endotoxemia and systemic inflammatory markers might improve in diabetic mice [13]. Furthermore, microbiota produces enzymes that degrade ingested polysaccharides, therefore promoting the absorption of nutrients particularly carbohydrates, leading to increased liver lipogenesis, hepatic IR, and hyperinsulinemia.
Authors added that various dietary components such as wheat fiber, inulin, or starch with high amylase content improve glucose absorption, decrease insulin secretion, increase the incretin GLP-1 level, and increase SCFA production and absorption. In hepatic steatosis 'a health-related risk of obesity and T2DM', a proton magnetic resonance spectroscopy used to measure intrahepatocellular lipids and intramyocellular lipids showed a close correlation between body adiposity and hepatic steatosis [14]. Importantly, by giving Agave inulin (inulin type with different chemical structure and botanical origin) to healthy adults in a randomized dose of 0, 5.0, or 7.5 g/day, there was a positive correlation between agave inulin intake and Bifid bacterium which is a promising shift of the gastrointestinal microbiota composition and activity in healthy adults [15].
In terms of body weight (BW) and fat mass reduction Abrams et al. observed a significant BMI reduction and less increase in fat mass for adolescents who received 8 grams oligofructose-enriched inulin daily for one year and this effect maintained in the following year [16]. A study by Dewulf et al. evaluated the contribution of the gut microbiota to the modulated host metabolism by dietary inulin- type fructans (ITF) prebiotics in obese women and found that ITF decreased the fat mass, serum lipopolysaccharides, and plasma lactate and phospha tidylcholine levels [17]. A recent comparison between the effects of fructooligosaccharides (FOS) and high- fat "western" diet with or without 2.5% FOS supplementation ad libitum on the development of obesity in rats showed that BW and percent body fat were lower FOS group while the weight of the visceral adipose tissue, and the weight and triglyceride content of the liver were significantly lower in the high-fat + FOS group.
Moreover, fecal excretion of lipids markedly potentiated by FOS consumption thus indicated the suppression effect of dietary FOS to the high-fat diet-induced body fat accumulation, and intestinal absorption of dietary fat [18]. Another comparison between non- fermentable (10% cellulose) and fermentable inulin, the results showed that the short-term inulin feeding in mice positively impacted the lipid metabolism [19]. On clinical grounds, inulin demonstrated a significant role in health-protective effects and disease-reversal benefits particularly with high level of intake. Data showed a positive impact on cardiovascular health disease, hypertension, diabetes, obesity, and certain gastrointestinal diseases. Additionally, high fiber intake improves serum lipoprotein values, lowers hypertension, improves blood glucose control for diabetic patients, and leads to weight loss [20].
Rebello et al. [21] examined the effects of a gastrointestinal microbiome modulator containing inulin on metabolic parameters, fecal markers of gut microbiota, and satiety where the results confirmed an improvement in glucose tolerance and satiety. Johnston et al. [22] demonstrated better insulin sensitivity with chronic consumption of resistant starch in individuals with MetS though a non-significant effect observed on BW, fat storage in muscle, liver or visceral depots. Additionally, there was no change on vascular function or markers of inflammation Fernandes, Vogt & Wolever compared markers of colonic fermentation after acute inulin ingestion in individuals with normal (<40pmol/l) and high (≥40 pmol/l) plasma insulin. The result supported that inulin increases short-term markers for colonic fermentation, thus produced SCFAs, acetate, propionate and butyrate, which might protect from T2DM by reducing serum free-fatty acids [23]. There is evidence that inulin-type fructans increases the GLP-1 level in the proximal colon that has a role in improving glucose tolerance, glucose-stimulated insulin secretion, insulin-sensitive hepatic glucose production, and thus reducing weight gain.
Furthermore, OFS could modulate gastrointestinal peptides such as peptide YY (PYY) and ghrelin that involved in the control of food intake. Data in humans reported the control of satiety facilitated by FOS as well as triglyceridemia, and steatohepatitis [24]. In male lean and obese rats, Parnell & Reimer evaluated the dose-dependent effects of inulin and oligofructose on gut satiety hormones, energy expenditure, gastric emptying and gut microbiota by giving randomized fiber intake of 0 to 20%. The authors concluded that bacteroides and total bacteria correlated positively with ghrelin and negatively with insulin demonstrating that prebiotics action of food intake, satiety hormones and alterations in gut microbiota are regulated in a dose-dependent manner which could have therapeutic potential for obesity [25]. In a similar context but plateau result, a dose of daily 10 grams inulin for 12 weeks duration showed no significant effect on serum glucose and lipid levels in T2DM patients which raised important questions regarding the optimal dose of inulin as dose-response and also the optimal dosage that is not studied in humans [26].
Kim et al conducted a small randomized clinical trials (RCT) in medical students' evaluating the effects of fructooligosaccharides (FOS) supplements on BW and body composition, blood lipid profiles, and Ca status. The results demonstrated a significant decrease in BMI, body fat mass, percent body fat and VF while skeletal muscle mass increased. Also there was a decrease in serum total cholesterol, LDL-cholesterol and triglycerides level while HDL-cholesterol calcium related biomarkers increased. Authors suggested that habitual FOS consumption considered as effective for weight reduction, improving lipid profiles, and calcium status [27]. Guess et al. [28] concluded that inulin may reduce the risk of diabetes by promoting weight loss and decreasing intrahepatocellular and intramyocellular lipid in subjects with prediabetes independent of weight loss [28]. A recent systematic review by Liu et al. [29] assessed the effects of ITF on human lipid profiles and glucose homeostasis complicated by dyslipidemia, overweight or obesity, and T2DM.
The authors found that the ITF consumption associated LDL reduction across all study populations, however, improvements of HDL and glucose control demonstrated only in the T2DM subgroup. Thus, additional, well-powered, long-term, RCTs are required for a definitive conclusion. Overall, ITF supplementation may provide a novel direction for improving the lipid profile and glucose metabolism [29]. A further recent animal study demonstrated that the additive effect of enriched-diet containing both lactalbumin and inulin decreased energy intake, supra-additively decreased BW, fat, and lean mass, in addition to decreased respiratory quotient and plasma leptin concentrations [30].
The review supported short-term significant beneficial effects of inulin on body weight with particular attention to the VF accumulation and its consequences though most data demonstrated obvious positive effects on lipid profile. Some studies focused on a high dose to yield an optimal dose-response effect. On the other hand the lack of standard safety guidelines on oral administration of inulin as prebiotics agents in human necessitates a careful consumption. Additionally, further long-term studies are essential to increase the understanding of the complex efficacy between ingested inulin and cardio-metabolic risks


