Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Jlalia Z*1 and Ben Salem O2
Received: February 11, 2018; Published: February 23, 2018
*Corresponding author: Zied Jlalia, Pediatric orthopedic department, Kassabinstitute for orthopedicsurgery, Ksarsaid 2010 Tunis, Tunisia
DOI: 10.26717/BJSTR.2018.02.000794
Abbreviations: INSAT: Institute Of Applied Science And Technology; BROS: Browser-Based Reconfigurable Orthopedic Surgery ; BW: Brower ; UC: Control Unit; MW: Middle Ware
Generally robots are used in different industries for many different applications. The medicalindustry, is one of those industries, which uses robots in different applications especially in the assistance of the surgeon duringhissurgery. These robots have advantages over humans (stability, precision and computer control). In orthopedicsurgery, these robots prevent the surgeon from being exposed to the ionizing radiation needed to perform several surgical techniques, including percutanées insertion of supracondylarelbow fractures in children. This fracture isacommonlesion in pediatrictraumatology [1]. The realization of thisrackingrequires the use of a brightness amplifier (generator of ionizing rays) necessary for the control of both the reduction of the fracture and its stabilization by pins [2]. But this control canonlybemonoplane in a moment T, thus increasing the risk of the reduction and trajectory defects of the pins which are successively controlled in the two planes of face and profile. In addition, the incorrect positioning of the pins can cause iatrogeniclesions of vessels and / or nerves passing in the region of the elbow [3].
In addition, a poor reduction of the fracture and / or a bad racking result in vicious consolidations and deformations of the elbow [4]. Another disadvantage of current treatmentis the recurrent exposure of medical and paramedical personnel to radiation whenusing the fluoroscopic arm [5]. These X-ray radiations are dangerous, and X-ray examinations usually involve radiation doses higherthan those generated by a simple X-ray [6,7]. Given these constraints and problems, a new national project called BROS (Browser-based Reconfigurable Orthopedic Surgery) was launched to address these issues. BROS is a new reconfigurable robotic platform dedicated to the treatment of supracondylarelbow fractures in children. It is able to work in several modes to meet the requirements of the surgeon and well-defined constraints. Thus BROS can perform the entire surgical procedure or bequeath certain tasks to the surgeon. The BROS architecture consists of a control unit, a navigation system combined with a middleware to perform image processing, two robotic arms to reduce the fracture and another to insert the pins at the level of the humer alpallet. This project has been launched to address the two most important problems facing medical and paramedical personnel, namely blind pinning and recurrent exposure to ionizing radiation.
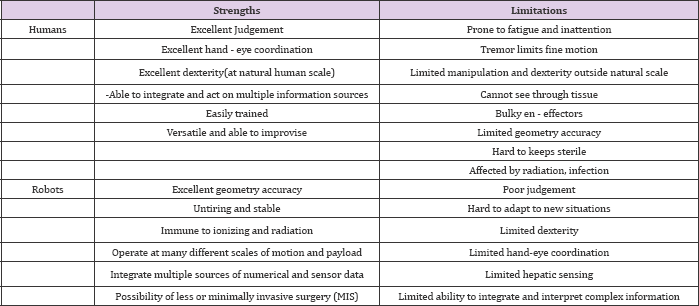
It is able to reduce fractures, block the arm and fix the fragments of the bones of the elbow by racking. It also offers a navigation function to track the progress of the pins in the fractured elbow. The field of computer-assisted surgery is relatively new. The first clinical application of a robot performed neurosurgeryin 1985 [8]. Since then, many research centers around the world have developed a multitude of robotic and computer-assisted surgical products, tackling new areas such as orthopedics [9] radiology [10], urology [11] cardiothoracic [12] and ophthalmology [1314]. At the beginning, the products consisted mainly of modifying industrial robots for a given procedure, but the safety of such mechanisms. Was called into question [15,16]. The current trend in surgical robotics is that systems will no longer be adaptations of industrial robots, but increasingly systems will be dedicated to a single task, with some autonomous capabilities and an extreme level of safety [17]. Medical robots are more and more accepted thanks to their ability to significantly improve surgeon's technical capability [18,19] They also take advantage of the complementary strengths between humans and robotic devices as described in [20,21] (Table 1).
Table 1: Complimentary strengths of robots and humans.
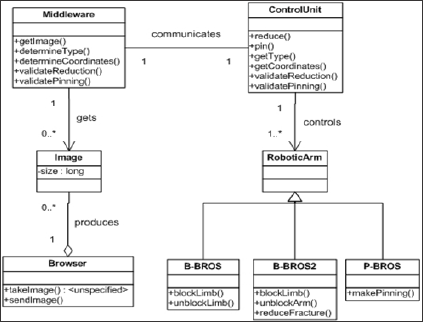
Their functionis far from replacing the surgeon, but supporting him with ameliorated dexterity, visual feedback, and information integration [22,23]. However, the systems still lack flexibility concerning their capacity to be autonomous and reconfigurable [24]. BROS is, as shown in the class diagram below (Figure 1), composed of a browser (BW), a control unit (UC), a middleware (MW), a robotic arm for racking-in (P-BROS) and 2 robotic arms for fracture reduction and arm locking (B-BROS1 and B-BROS2). Reconfiguration is an important feature of BROS. The latter is designed to be able to work in different modes. Le chirurgien peut en effet décider de réaliser manuellement une tâche si BROS ne parvient pas à l'exécuter automatiquement, que ce soit la réduction de la facture, le blocage du bras ou l'embrochage.
Figure 1: Diagramme De Classes De Bros.
Thus, five different modes of operation are designed. BROS offers a navigation function using the middleware which checks in real time the smooth running of the operation. This project embodies our desire in medicine and engineering to move forward in the field of knowledge. Adopted as a national project by the Ministry of Higher Education Tunisian this project was the subject of a doctorate of state in robotics, prepared at the National Institute of Applied Science and Technology (INSAT) and supported in Germany by the University of Saarland. This work involved the creation of a database of information on approximately 7,000 elbows of healthy and fractured children and the documentation of nearly 150 supracondylarelbow fractures in children collected at the Kassab Institute of Orthopedics and children hospital of Tunis between 2013 and 2016. The opening up of medicine in other areas is now a necessity, through the realization of this project we acquired a knowledge and a maturity to meet other challenges and join those who preceded us. The current state of our medicine must not prevent us from dreaming and hoping for the best, and I am certain that the future will be better. Thank you to all who helped us, they were a source of motivation and courage to lead this project to good port.


