Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Nam QD Vo*1 and Toan N Nguyen2
Received: February 13, 2017; Published: February 21, 2018
*Corresponding author: Nam QD Vo, Hospital for Traumatology and Orthopaedics, HCM City, Vietnam
DOI: 10.26717/BJSTR.2018.02.000784
Abbreviations: M: Mature; I: Immature; IF: Isolated Femoral Attachment; IP: Isolated Patellar Insertion; MID: Isolated Mid-Substance; COM: Combined MPFL Injuries; C: Complete Tear; P: Partial Tear
Patello femoral instability (PFI) is a debilitating injury for the patient and a challenging problem for the surgeon. The incidence of PFI ranges from 5.8 to 77.8 per 100,000 and recurrence rates of nonoperatively treated dislocations range from 15% to 50% [1]. In children and adolescents, the recent studies showed the incident of PFI of 43 per 100,000 [2] and the recurrent rates between 30% and 38% [2,3]. The medial patella femoral ligament (MPFL) is the primary soft-tissue restraint to lateral patellar translation [4]. The MPFL has a "sail-like" appearance with two functional portions: inferior straight bundle and superior oblique bundle. The MPFL originates from the medial femoral condoyle just proximal to the femoral attachment of the medial collateral ligament and distal to the adductor tubercle. It inserts on the super medial border of the patella. In children and adolescents with open phases, the femoral insertion is located slightly distal (4 to 5mm) to the medial femoral physics [5]. During 0 to 30 degrees of knee flexion, the MPFL contributes more than 60% of the medial stability of the patella and isolated insufficiency leads to increased lateralization or dislocation [6].
In cases of first-time acute lateral patellar dislocation, injury to the MPFL is described as the essential lesion, occurring in almost 100% of cases [7]. Repair, reefing, and advancement of the MPFL and medial retinacular structures can be performed as an isolated procedure or in conjunction with distal realignment procedures for patients with patellar instability. Understanding and appreciating MPFL injury patterns ultimately determines the success or failure of these procedures. Unfortunately, the location and pattern of MPFL injury cannot be consistently predicted [2]. Although early surgical dissections described femoral-sided injuries as the most common injury site, the recent studies using magnetic resonance imaging (MRI) have described a more even distribution of MPFL injury patterns, which include isolated patellar insertion ruptures, isolated femoral attachment ruptures, isolated mid-substance ruptures, and combined MPFL injuries [8].
This review focuses on the MRI-based studies of MPFL injury patterns, and related factors as age, injury severity and acute or recurrent PFI. These studies are shown in the (Table 1). Although most of these 9 studies (7 studies) are of primary PFI, prevalence of MRI-defined MPFL injuries ranges from 44.4% to 100%; and injury prediction in immature patient is much lower than in mature patient [3,9] and Wilson [9] stated that MPFL did not always tear in immature PFI. Some authors recommended some solutions that complement to investigate MPFL injuries as arthroscopic surgery [6], HR-MRI with microscopy coin [10]. In acute MPFL injuries, the complete tear is a bit more popular than the partial tear [11,12].
Table 1: MRI-based studies of MPFL injury patterns.
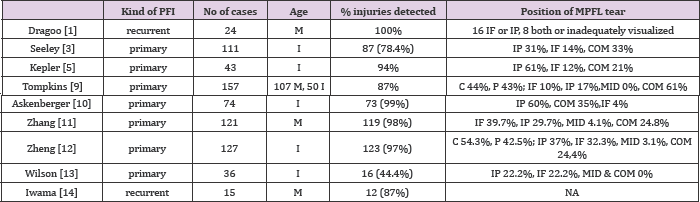
For detecting the location of MPFL injury, these studies in mature patients did not show what is the most among isolated patellar insertion ruptures, isolated femoral attachment ruptures, isolated mid-substance ruptures, and combined injuries; except the isolated mid-substance rupture was very rare 0-4% [1,11,13]. However, many studies proved the dominance of isolated patellar insertion ruptures in immature patients, and the combined MPFL injuries were more popular than the isolated femoral attachment ruptures, and the isolated mid-substance rupture was also very rare in immature patients 0-3% [3,5,9,11,12,14]. On the other hand, the complete MPFL tear was more often concomitant with osteochondral lesions of the lateral femoral condyle than the partial MPFL tear; the isolated patellar insertion ruptures and the combined MPFL injuries were more easily concomitant with osteochondral lesions of the lateral femoral condyle than the isolated femoral attachment ruptures. These results were from a study in adults [13] and a study in children and adolescents [12].
In conclusion, the location and pattern of MPFL injury were not consistently predicted on MRI and many studies proved the dominance of isolated patellar insertion ruptures in immature patients. Moreover, there is still the lack of MRI-based studies of MPFL injury for recurrent PFI.


