Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Cynara Ferreira Bernardes1, Manoel Barros Bertolo1, Michael Davitt2, Cecilia Morais Barbosa1, Juliana Zonzini Gaino1, Eduardo de Paiva Magalhaes2
Received: January 27, 2018; Published: February 07, 2018
Corresponding author: Eduardo de Paiva Magalhaes, Department of Internal Medicine, Rheumatology, Faculty of Medical Sciences, State University of Campinas/Unicamp, FCM/UNICAMP, Campinas/SP, Caixa Postal:6111, CEP:13083-970, Brazil
DOI: 10.26717/BJSTR.2018.02.000740
Objective: To evaluate the efficacy of insoles in rheumatoid foot reducing pain, improving function and mean peak pressure.
Methods: This was an observational study. 27 patients with foot pain, referred to Orthoses and Prostheses Unit of Unicamp were assessed regarding foot pain, foot deformity, disability (Health Assessment Questionnaire – HAQ-DI) and disease activity (Clinical Disease Activity Index – CDAI). Foot orthoses were prescribed according to each patient’s needs aiming to reduce pain, improve function and reduce the mean peak plantar pressures. The Foot Function Index (FFI) and the pedobarography (FSCAN system) were assessed at base line and after two weeks of intervention.
Results: FFI values decreased in all subscales (pain, disability and activity limitation) with orthoses. No significant difference was noted in the plantar pressure. CDAI and HAQ-DI were associated with FFI but not with plantar pressure. Orthoses were worn on average for was 7.08 hours-day. Minor adverse effects were noted in 7 patients, none of them resulting in treatment interruption.
Conclusion: Insoles may reduce foot pain and disability with no significant improvement in plantar pressure distribution in rheumatoid patients with established disease.
Keywords: Foot Orthoses; Rheumatoid Arthritis; Pedobarography; Insoles; Rheumatoid Foot
Rheumatoid arthritis (RA) is a chronic autoimmune disease where feet are involved in up to 90% of patients [1]. Rheumatoid foot results from chronic inflammation followed by structural and biomechanical changes. It may differ much from one patient to other and even from one foot to the contralateral [2]. The most common manifestations are metatarsophalangeal joints subluxations, widening of the forefoot, hallux valgus, claw toe deformities, subtalar and talonavicular synovitis, ankle valgus deformity, flat foot and posterior tibial tendon rupture [1,2]. This condition results in in pain, alterations in the loading pattern of the foot during weight bearing, limitations in daily activities and a reduction in quality of life [3]. Foot orthoses, especially insoles, are commonly used as an adjuvant therapy for the rheumatoid foot aiming to correct or improve plantar load and stabilize foot and ankle [3,4]. Many modifications can be applied to the insole such as medial contoured arch support, metatarsal and heel pads, soft cushioning in overweight areas [5]. Systematic review of the effect of foot orthoses in RA observed significant evidence of foot pain reduction but it is still uncertain if it could result in function improvement, foot deformity prevention or plantar pressure reduction [6]. The aim of this study was to evaluate the effect of insoles in RA patients regarding foot pain, function and plantar pressure distribution.
This was an open observational study conducted in Orthoses and Prostheses Unit of the Clinical Hospital of the State University of Campinas (UOP-Unicamp). The study has been approved by the Ethics Committee of the Faculty of Medical Sciences, State University of Campinas-Unicamp, in accordance with the Declaration of Helsinki.
Subject's Consecutive patients who were referred to podiatric treatment in UOP-Unicamp were approached to participate in the present study. The inclusion criteria were a definitive diagnosis of RA according to the The American College of Rheumatology criteria [7], the presence of feet pain, age > 20 years old, and stable drug treatment in the past 4 months. They were excluded if wearing any foot orthosis during the past month, in the presence of foot skin lesions, concomitant neurological or muscle disease, previous foot surgery, if they were unable to follow the instructions of the protocol and attend to revaluation. All subjects have read and signed an informed consent before study inclusion.
At the first visit subjects had their sociodemographic (age, race, marital status, education, income) and anthropometric (Body mass index-BMI) data collected and physical assessment performed. Patient medical history was assessed and physical examination was performed. Foot deformities, pain and callosities were noted and patients were asked to identify the main pain site in the forefoot (toes, MTF joints) or in the hindfoot (midfoot, calcaneus and ankles). All patients had the Clinical Disease Activity Score (CDAI) assessed by a rheumatologist [8]. Foot orthoses were prescribed in accordance to each patient's needs. Pedobarography was performed at initial visit (without orthoses) and after two weeks (with orthoses). Subjects were also asked to answer FFI and HAQ at the beginning and at the end of protocol. Satisfaction with the intervention was assessed asking the following question: "How did you feel after using the insoles?" (much worse, worse, same, better and much better).
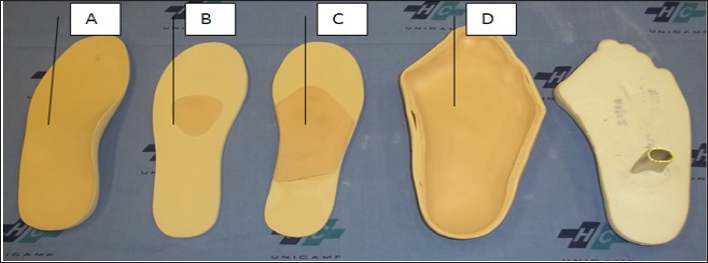
All subjects received custom foot orthoses made of ethylene- vinyl acetate (EVA) manufactured in UOP-Unicamp under the supervision of an experienced podiatrist. The objective of the insoles was supportive, not corrective. For patients with flat foot, a 12mm-thick medial arch support was prescribed; for those with metatarsalgia or callosities under the metatarsal heads, a 6mm-thick pad supporting the diaphysis from the second to fourth metatarsal bones or a 6mm-thick dome supporting the diaphysis from the first to fifth metatarsal bones was indicated. For very deformed feet, made-to-measure insoles were preferred, manufactured from a plaster cast mold (Figure 1). Insoles were adapted to patient's own footwear. The subjects were instructed to use the insoles during brief periods of the day at the beginning of the study; when they felt more comfortable, with pain relief, they could use them for most of the day.
Figure 1: Insoles with medial arch support (A), metatarsal pad (B), metatarsal dome (C) and made-to-measure insole with plaster cast mold (D).
Foot pain, function, disability and plantar pressure were assessed at baseline and after two weeks. The instruments used for data collecton included the Foot Function Index (FFI), The Health Assessment Questionnaire (HAQ-DI) and the pedobarography. The FFI consists of 23 items about the impact of foot impairments in three subscales: foot pain (FFI pain) (nine items), foot disability (nine items) and activity limitation (five items) [9]. In the Brazilian version of FFI, the original 100 mm visual analogue scale was changed to an analogue scale (0-10) to make it more comprehensive to the local population [10]. Each patient was asked to mark the number which best reflected his or her condition on each situation. To obtain a subscale score, the values of each item were totalled and divided by the number of items considered applicable by the patient. Calculating the average of the three subscale scores produced a total FFI score (FFI total). The HAQ-DI consists of 20 questions in eight categories which represent the activities of daily living, and for each category, there are two to four questions [11,12]. The responses are scored on a four-point scale: 0 without difficulty; 1 with some difficulty; 2 with difficulty; 3 impossible. The highest score for each of the eight categories is taken as the score for that category. The final score of the questionnaire is the averaged score of all the categories and ranges between 0 and 3.
For the pedobarography the F-scan in-shoe sytem was used (Version 4.11, Tekscan, Boston/MA - USA). The system uses thin pressure sensors trimmed to the foot size of individual shoe with up to 960 sensor cells; sensors are linked to a computer via cables for data acquisition. Calibration of the system was done with the patients supporting themselves on each foot alternately. For data acquision each patient followed the pre-established trajectory walking forward at a comfortable speed, for 3 minutes, until a comfortable and stable cadence was achieved. Gait parameters were then recorded for 8 seconds. Patients could not see or receive any sort of sensorial feedback that might interfere with their pace during recording. The mean peak plantar pressure was assessed in seven predetermined plantar subregions regions: five regions of the forefoot (Region 1: hallux, Region 2: 2+ to 5th toes, Region 3: 1st MTF joint, Region 4: 2nd to 4th MTF joints; Region 5: 5th MTF joint) and two regions of the hindfoot (Region 6: midfoot and Region 7: calcaneus).
The mean, standard deviation (SD), median and maximum (max) and minimum (min) values of each variable were calculated for sample profile analysis. To compare the peak pressure averaging values between times the Wilcoxon test for related samples was used, due to lack of normal distribution of the variables. To analyze the relationship between numerical variables (age, BMI, disease duration, CDAI, HAQ, FFI) and peak pressure averaging, the Spearman's correlation coefficient was used. For statical analysis, we used the SAS System for Windows (Statistical Analysis System), version 9.1.3, SAS Institute, Cary, NC, USA). A significance level of p< 0.05 was was considere to indicate significance.
Figure 2: Study flow diagram.
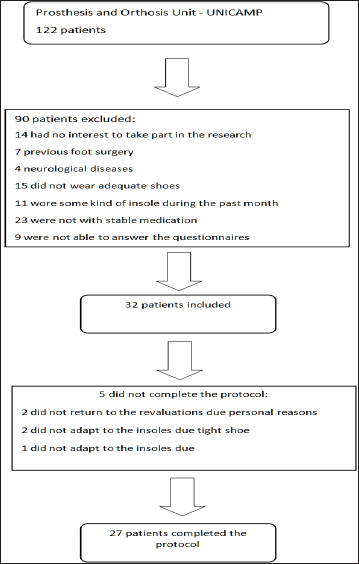
122 patients were assessed during the study. 14 had no interest to take part in the research, 7 were excluded due previous foot surgery, 4 due neurological diseases, 15 did not wear adequated shoes, 11 wore insoles during the past month, 23 were not with stable medication, 9 were not able to answer the proposed questionnaires and 7 related difficulty to attend to revaluation in adequate time. 32 subjects were included in the study. From these 5 did not complete the protocol (2 did not return to the revaluations due personal reasons not related to the orthosis, 2 did not adaptated to the insoles due tight shoe and 1 due feeling hot in the feet) (Figure 2). 27 subjects (23 women and 4 men), aged 48.62 year-old (23-68, ±11.79) completed the study. Most of them were white (66.66%), married (59.25%), with less than eight years of education (55.55%) and 70.37% with income < R$1500.00 per month (~US$500.00). The mean BMI was 25.34 (±4.18, 17.3034.88). The disease mean time was 11.52 yrs (± 8.13, 2-32) and the mean CDAI was 23.19 (±13.62, 1-61). The most common foot deformity was claw toes, present in 34 feet (62.96%), followed by flat feet in 21 feet (38.88%), halux valgus in 16 feet (29.63%), 6 ankle valgus (11.11%), 2 halux varus (3.7%) and 2 ankle varus (3.7%). Calosities in the forefoot were noted in 19 feet (35.18%) and in the mid- and the hindfoot in 4 (7.4%) feet. 18 patients referred pain predominance on the forefoot (66.66%) and 9 on the hindfoot (33.34%).
Concerning insoles modifications, the metatarsal dome was prescribed for 26 feet, the metarsal pad for 6 feet and the medial arch support for 20 feet. For 3 patients with very deformed feet, made-to-measure insoles, manufactured from a plaster cast mold, were preferred.
Table 1 shows the values of FFI.... (subscales pain, disability and activity limitation and total scores) and HAQ-DI in the initial evaluation without insole and after two weeks wearing foot orthoses. Significant differences were noted for the FFI in all subscales, but not for the HAQ-DI. Higher initial disability and activity limitation FFI subscales and FFI total scores were significantly related to higher CDAI and HAQ-DI scores (p < 0.05). FFI improvement was independent of age, disease duration, CDAI and HAQ-DI.
Table 2 shows the mean peak... plantar pressure considering the 7 determined plantar subregions. After intervention, no significant plantar pressure reduction was noted. On the contrary, a significant elevation of plantar pressure was observed in subregions 4 (2nd to 4th MTF), 5 (5th MTF) and 6 (Midfoot). Even when evaluating separately the patients with pain on the forefoot and on the hindfoot no significant reduction could be noted in plantar pressure distribution (data not shown). There was no significant relation between the mean peak of pressure values and the variables disease duration, FFI, HAQ-DI and CDAI. Orthoses were worn on average for was 7.08 hours-day. Adverse effects were observed in 7 patients as it follows: 4 with difficulty to adapt to the shoes; 2 with pain at the first few days of intervention; and one felt hot feet. None of them resulted in treatment interruption. When argued about the satisfaction with the treatment, 8 patients considered they were much better and 19 considered they were better after the intervention.
Table 1: Foot Function Index - FFI (subscales Pain, Difficulty, Disability and Total scores) and HAQ-DI values - mean (± standard deviation, minimum value - maximum value, median) - between baseline and after two weeks of wearing foot orthoses (T2).

Note: *p-value for the Wilcoxon test.
Table 2: The mean peak plantar pressure (kPa) - mean (± standard deviation, minimum value-maximum value, median) - at baseline without insoles and after two weeks wearing insoles considering the following subregions: Region 1 - hallux, Region 2 - 2nd to 5th toes, Region 3 - 1st MTF joint, Region 4 - 2nd to 4th MTF joints; Region 5- 5th MTF joint, Region 6: midfoot and Region 7: calcaneus.
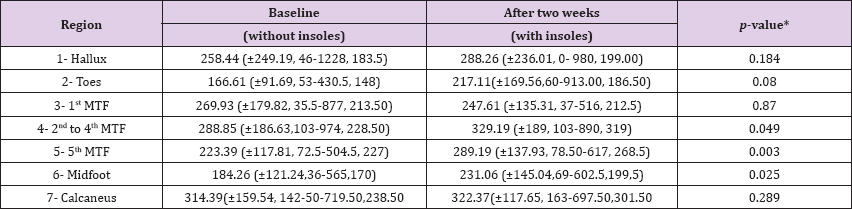
Note: *p-value for the Wilcoxon test for comparison of variables between baseline and after two weeks.
Foot orthoses are commonly indicated for patients with rheumatoid foot to reduce pain. They are also supposed to improve foot function and lead to a better plantar pressure distribution but these effects are not well established [6]. In this sample, the use of insoles was related to FFI improvement in all subscales (pain, difficulty and disability). FFI improvement with foot orthoses has been already reported. In a randomized trial Woodburn et al.[13] observed FFI reduction during 30 months of follow-up and in two additional studies, one observational with 36 subjects [5] and other randomized controlled trial with 45 subjects, the use of insoles resulted in FFI improvement after six months of follow-up[14] . On the contrary, Conrad et al. [15] in a study comparing foot orthoses vs placebo, found no clinical significant difference in FFI between groups. However, their subjects were atypical older male rheumatoid patients and the placebo orthoses used could have also interfered in the final results.
Despite FFI improvement there was no significant reduction in plantar pressure with insoles. On the contrary, it increased in the forefoot and in the mid foot.
There are few studies evaluating plantar pressure in RA and although the use of pedobarography has increased in clinical practice, its usefulness and relevance has not been proved [16]. In one study Li et al. [17] observed plantar pressure reduction in twelve rheumatoid subjects using a standard insole with metatarsal pad and medial arch support. Similarly, Jackson et al. [18] described plantar pressure reduction in eleven patient with forefoot pain wearing metatarsal pads. Also Hodge et al. [19] observed reduction of pressure beneath the first and the second metatarsal heads in twelve subjects using four kinds of insoles. All of these studies included a small number of subjects with no severe foot deformity. Plantar pressure reduction was also reported in subjects with early RA as reported by Santos and Cameron-Fiddes [20] evaluating 35 subjects wearing off-the-shelf foot orthoses and by Tenten- Diepnmaat et al. [21] studying 45 subjects using custom made foot orthoses. In subjects with advanced foot disease, plantar pressure and clinical diagnosis do not always correlate [16]. Schmiegel et al. [22] evaluated the foot pressure of 112 subjects with RA and observed that pedobarography did not score the highest-pressure values in the areas of severe pain suggesting that it could be unable to detect patient's habit of avoiding pressure in the area of pain (antalgic gait). Telfer et al. [23] did not observe significant changes in plantar pressure caused by orthotic interventions in a group of 15 patients with long time RA. The fact that our sample consisted most of patients with long time disease, with well-established and diverse deformities probably have influenced the results tours a non significant effect in plantar pressure reduction.
FFI-rather than plantar pressure, better reflected subjects' improvement. HAQ-DI and CDAI were also related to FFI, but not to plantar pressure. Plantar pressure analysis in subjects using foot orthoses may be confounding when evaluating subjects with advanced and heterogeneous disease being more useful when assessing subjects with early disease, with few deformities or with specific findings such as subjects only with metatarsalgia or with hallux valgus. This study has many limitations. As described before, subjects studied presented long time and active disease with advanced installed deformities. The group of subjects studied were also heterogeneous both with forefoot and hindfoot problems. It was not possible to use standard foot orthoses and insoles were custom molded according to patient's needs. Shoes were not controlled and may have influenced the results. It is difficult to use control foot wear since it is known that patients with RA show difficulties in wearing orthopedics shoes preferring sport shoes or adapted shoes with a better design [4]. There was not a control group, so we cannot rule out a placebo effect in relation to FFI improvement.
The use of insoles in rheumatoid patients reduced foot pain and disability with no significant effect in plantar pressure reduction. This intervention was well-accepted by the patients, used during long periods of the day, without significant adverse effects.
We would like to thank Mr. Helymar da Costa Machado and Ms Cleide Aparecida Moreira da Silva for the statistical analysis and the staff of UOP-Unicamp.


