Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Sergio Carmona*1, Gabriela Grinstein2, Romina Weinschelbaum3 and Guillermo Zalazar4
Received: January 20, 2018; Published: January 31, 2018
Corresponding author: Sergio Carmona, Department of Neuro-Otology, Fundación San Lucas para la Neurociencia, Rosario, Santa Fe, Argentina
DOI: 10.26717/BJSTR.2018.02.000711
We present the case of a 14-year-old girl, who presented with a positional vertigo of second duration, compatible with BPPV, but whose final diagnosis was a cavernoma in the cerebellum. We emphasize the importance of keeping in mind the different etiologies of vestibular syndrome in children.
Keywords: BPPV; Cavernoma; Episodic vestibular syndrome; Atypical BPPV
Abbreviations: BPPV: Benign Paroxysmal Positional Vertigo; Y.O: Year Old; NSAIDs: Nonsteroidal Anti-Inflammatory Drugs; HIT: Head Impulse Test; MRI: Magnetic Resonance Imaging
BPPV is the most frequent cause of recurrent vertigo [1]. and its incidence increases with age [2]. As it is not a frequent event in children, a research on prevalence at a pediatric age found BPPV to be a cause of vertigo in a 3.88%, and 3.4% [3]. For the age group of the patient here discussed. When we have to study a clinical picture with characteristics similar those to BPPV but a history, symptoms or clinical findings that are not the typical ones of a vertigo caused by a detachment of the otoliths, other canalithiasis or cupolithiasis non-related causes must be considered.
Female patient, 14 y.o., with no relevant clinical history, who consults due to frontal headache, which partially improves with NSAIDs, positional vertigo that lasts seconds, permanent dizziness and neurovegetative symptoms: nausea and vomiting over the last week. Patient denies motion sickness; father refers having suffered from migraine in his adolescence, with no symptoms as an adult. No maternal history of migraine.
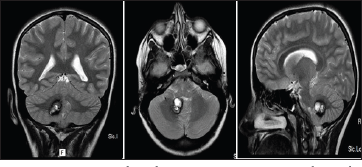
Bilateral negative bedside HIT. Negative head shaking. Patient presents geotropic nystagmus with both head rotations and greater nystagmus intensity with left turn (Figure 1). She presents neurovegetative symptoms during examination. It is interpreted as left horizontal canalithiasis. Lempert maneuver is performed. Evolution: symptoms improve 3 days later. Mild nystagmus persists with left head turn. Lempert maneuver is performed again. 4 days later patient is controlled: she refers having experienced a clinical improvement in the previous days. Today patient refers suffering from headache and dizziness when changing positions. She does not show positional nor did gaze evoke nystagmus. She presents horizontal nystagmus with right head turn, downbeat nystagmus with left head turn. A brain MRI is requested. MRI shows a heterogeneous lesion in right cerebellar hemisphere with signs of subacute bleeding compatible with right cavernoma (Figure 2).
The patient was clinically presented as a geotropic lateral canal BPPV, yet, several atypical characteristics must be considered: the first one is age [2,3]. When there is no history of trauma. The patient s answer to the maneuvers applied was inconsistent and during the evolution she presented a vertical downbeat nistagmus which cannot be explained as due to changes related to severity. Carmona et al. recently presented a 4 [4], Where they found a prolonged geotropic horizontal nystagmus accentuated to the side in which the patient had an acoustic neuroma and the authors speculate that, given the size of the tumor, there may be a dynamic compression of the vestibular nuclei which may generate variable information on the velocity storage mechanism or perhaps a true BPPV with an impaired velocity storage mechanism [5]. The presence of atypical BPPV must be studied with imaging studies, in this case of acoustic neuroma, hearing was symmetric and the only key were the atypical signs of the BPPV as explained. In this case, the acute onset of symptoms and the evidence of intracavernous bleeding may have an effect on the nodulus that regulates the nystagmic answer, which would also explain the change of direction in the nystagmus [6].
Figure 1: Videonistagmografía-Pruebas posicionales
Figure 2: IRM ponderada en T2, cortes coronal axial y sagital
BPPV is uncommon at a pediatric age, mainly in the absence of a history of trauma, and this, together with the evolution led in our case to an etiologic diagnosis of central pathology


