Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Holst T1, MakariousLaham M1, Heckmann J2, Roosta-Azad M1, Bigdeli H1, Zandi A1 , Koch A2 and Kamler M*1,2
Received: January 09, 2018; Published: January 18, 2018
*Corresponding author: Kamler M, Heart Center Essen Huttrop, University Hospital Essen, Germany; Department of Thoracic and Cardiovascular Surgery, West-German Heart and Vascular Center Essen, University Hospital Essen, Germany
DOI: 10.26717/BJSTR.2018.02.000669
Extracorporeal life support (ECLS) is a powerful tool for cardio respiratory support in cardiogenic shock. A 24 year old female patient was admitted with acute heart failure due to amphetamine use and emotional stress leading to cardiac arrest. After successful treatment with ECLS the patient was discharged from hospital at day 14.
Abbreviations: ECLS: Extracorporeal Life Support
Acute heart failure is associated with significant morbidity and mortality. Medical therapy appears to be inadequate in severe decompensation. Extracorporeal life support (ECLS) is a promising tool for these patients [1-3], allowing immediate restoration of circulation and further therapeutic measures.
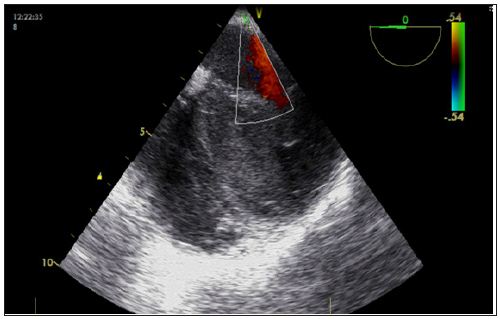
We present a case of a 24 years old female patient with acute asthma leading to cardiac arrest out of hospital due to extensive amphetamine use combined with a violent conflict in her family. After intubation by an emergency physician she was admitted to an external hospital ICU under ongoing conventional cardiopulmonary resuscitation. Since subsequent advanced cardiac life support could not achieve a return of spontaneous circulation ECLS was established as a bridge to therapy or recovery on site by our institutional “ECMO team”. ECLS was implanted left femoral and an additional cannula for left leg perfusion was installed. Further on the patient was transferred to our specialized ICU. TEE showed a ballooning resembling heart with octopus trap configuration and stunning left ventricular wall motion (Figure 1).
Figure 1: TEE at arrival. A ballooning resembling heart with octopus trap configuration and stunning left ventricular wall motion treated with ECLS. Nearby septum flow is low showing blood stasis.
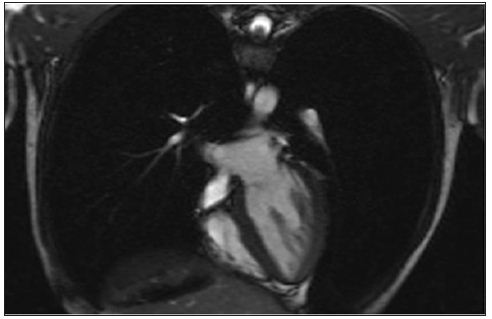
ECG findings were T-wave inversion with QT-interval prolongation. Laboratory investigation showed mild TnT elevations 0.229 ng/ml and high liver parameters (1097 U/l GOT/ASAT) and a neuron- specific enolase value of 39.33 ng/ml. ECLS flow was 3,8 l/m (Patient 160 cm / 50 kg). Patient was stabilized with moderate catecholamine doses. Cranial computer tomography showed a moderate brain edema (Figure 1). Repeat TEE on day 3 of ECLS showed normal left ventricular dimensions with moderate left ventricular wall motion dysfunction (40 % ejection fraction) under low catecholamine use and ECLS. ECLS was weaned and removed at day 6. Post ECLS recovery was unremarkable. The patient was transferred to a cardiologic department were further investigations were performed with no pathological findings. Cardiac magnetic resonance imaging on day 12 after ECLS implantation showed a clinical completely recovered heart with no wall dysfunctions. The patient was discharged home after a total of 14 days (Figure 2).
Figure 2: MRI 12 days after ECLS implantation presenting a completely recovered heart.
Takotsubo cardiomyopathy is a type of non-ischemic cardiomyopathy. Because this weakening can be triggered by emotional stress, a break-up, or constant anxiety, it is also known as broken- heart syndrome and is characterized by left mid ventricular and often apical dysfunction and ballooning with sparing of basal segments in the absence of acute coronary artery obstruction [4,5]. This was fulminant in our case and was successfully treated with ECLS. Despite this new concepts and strategies of advanced life support, the outcome of patients with out of hospital cardiac arrest remains poor. The main reason accounting for these poor results is a low flow phase during conventional cardiopulmonary resuscitation with insufficient end organ perfusion. As shown in this case, early use of systems as ECLS during conventional cardiopulmonary resuscitation might improve survival as well as the neurological outcome in resuscitated patients. ECLS has been proved to increase survival in acute or chronic heart failure [1].
That’s why some cardiothoracic surgery departments have launched ”ECMO teams” to ensure area-wide patient centered care with such systems to escalate advanced life support in fulminant cases. In our case we could achieve complete recovery without any neurological deficits. Early use of systems as ECLS might improve the outcome in patients with prolonged cardiac arrest. Use of these systems should be based on the individual decision of an experienced “ECMO team” considering defined inclusion and exclusion criteria and considering the risk of complications such as bleeding, clotting, infection, limb ischemia and organ failure. As outcome mainly depends on the duration and the quality of conventional cardiopulmonary resuscitation, an “ECMO team” support should be requested within minutes after establishing advanced life support.


