Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Dario Di Nardo*1, Gianluca Gambarini1, Riccardo Costantini1, Luca Testarelli1, Lucila Piasecki2 and Dina Al-Sudani3
Received: January 04, 2018; Published: January 10, 2018
Corresponding author: Dott Dario Di Nardo, Department of Oral and Maxillo Facial Sciences, Sapienza University of Rome, Italy
DOI: 10.26717/BJSTR.2018.02.000648
Aim To present the combined use of CBCT images and new endodontic software to identify and then facilitate the location and treatment of a canal in an unusually placed second mesio-buccal root of a maxillary left second molar. Summary A 45-year-old female was referred for root canal treatment on her maxillary left second molar tooth (tooth 27). Due to superimposition of the third molar and the position of the tooth that made conventional radiographs unhelpful, a pre-operative limited FOV, Low-Dose Technology™ CBCT image was taken with an OP-300 Maxio™ device (Instrumentarium, Helsinki, Finland). The CBCT images were then imported and analyzed using 3D Endo™ Software (Dentsply Sirona, Wels bei Salzburg, Austria). Within the software, the canal orifices and foramina were located and identified on the display, which allowed the software to automatically reveal and measure the pathway of each canal, which was traced and viewed in both frontal and mesial perspectives. The images revealed the presence of a separate second mesiobuccal root that contained one canal. Root canal treatment was then performed using the information derived from the software. The orifice of the canal in the second MB root was located in an unusual position: 5.99 mm palatally to the main MB canal and 7.57 mm medially from the palatal canal. An immediate post-operative limited FOV, low-dose CBCT was taken to assess the quality of the root filling. After one year the tooth was asymptomatic and radiographic examination revealed no sign of periapical pathosis.
Keywords: Anatomy, Maxillary Molar, Mesio-Buccal Canal, CBCT
Key Learning Points:
a) The variable anatomy of maxillary second molar teeth
b) The unusual (palatal) location of the second mesio-buccal root and canal in this case
c) The combined use of CBCT and 3D endodontic software for pre-operative assessment of complex cases in order to identify and manage risk.
The variability and complexity of root canal morphology in multi-rooted teeth is a challenge for the practitioner [1]. Knowledge of the most common anatomic characteristics and their possible variations is fundamental, because a missed canal is a leading cause of treatment failure [2,3]. The anatomy of maxillary second molars is similar to that of maxillary first molars; however, their main distinctive morphological feature is that the usual three roots align more closely and are occasionally fused [4]. Although four canals are found less often in the second molar than in the first molar [5]. Its canal configuration is more variable [6]. Indeed, many studies have described morphologic variations in maxillary molars, with multiple canals in each root, especially bi- or tri-furcated palatal canals [7-11]. Unusual anatomy in maxillary second molars is often difficult to diagnose because of its posterior location [12]. The superimposition of anatomical structures on conventional radiographs of this tooth may fail to reveal a bifurcated palatal root canal or other anatomical variations, such as single or double roots and fused roots [13,14]. Cone-beam computed tomographic (CBCT) images are useful in providing accurate anatomic details in three dimensions for diagnosis and treatment planning before root canal treatment [15,16]. More recently, a software package has been developed for analyzing endodontic parameters on CBCT images, 3D Endo™ (Dentsply Sirona, Wels bei Salzburg, Austria), which provides a user-friendly interface for the identification, visualization and measurement of root canals using a colour coded system for enhanced visualization of the trajectory of each canal.
A 45-year-old female was referred for root canal treatment on her maxillary left second molar (tooth 27). The referring dentists had previously taken an intraoral digital radiograph (Figure 1a) but due to the superimposition of the third molar and position of the tooth a pre-operative limited FOV, Low-Dose Technology™ CBCT image was acquired using an OP-300 Maxio™ device (Instrumentarium, Helsinki, Finland) adopting the following parameters: field of view (FOV): 50x50 mm, spatial resolution: 0.28 mm voxels, 90 kVp and 3.2 mA. A cold pulp sensibility test initiated a response from the patient. No swelling, mobility or tenderness to percussion was recorded. The CBCT images revealed a very unusual anatomy with a second mesial root located palatally. This root was adjacent to the main mesial root in the coronal region, and then diverged palatally; it had its own canal with an independent foramen (Figure 2a) similar to the MB2 canal that would be present in a single mesio-buccal root. To visualize better this unusual configuration and to determine the optimum access cavity design so as to locate all canal orifices, CBCT images were then analyzed using the 3D Endo™ Software. The software was used to crop the area corresponding to the tooth in the axial and para-sagittal planes. Once the tooth was selected, the canal orifices and foramina were located and identified in the next screen. This allowed the software to automatically reveal the pathways of the four canals, which were traced in different colours and viewed in frontal and mesial views (Figure 2b). The software also allowed a virtual access cavity design to be visualised along with the path of insertion of endodontic instruments within the canals (Figures 3a-3b); the number of roots and canals, their lengths and trajectories, and the position of orifices were identified easily. 3D volumetric rendering of the tooth was then performed using the OP-300 Maxio™ imaging software, to compare 3D pre- and post-operative images (Figures 4a-4b).
Figure 1a: Pre operative traditional radiograph taken by referring dentist with superimposition of the third molar.
Figure 1b: Control after one year: traditional radiograph taken by referring dentist.

Figure 2a: Axial CBCT image showing distance between second MB canal and MB (5,99 mm) and between second MB canal and palatal canal (7,57 mm).
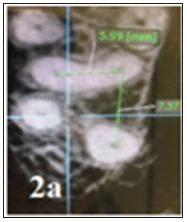
Figure 2b: 3D Endo™ Software image showing virtual access cavity and insertion of endodontic instruments in the four canals.

Figure 3a: Images from 3D Endo™ Software showing the different canal trajectories with different colours.

Figure 3b: Virtually inserted endodontic instruments inside the four different canals and following their trajectories.

Figure 4a: Preoperative 3D reconstruction (rendering) of initial anatomy (4a) showing the unusual root anatomy.
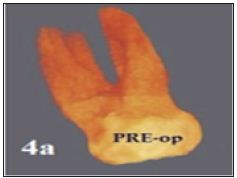
Figure 4b: Postoperative 3D rendering after canal obturation showing the four canals properly treated.
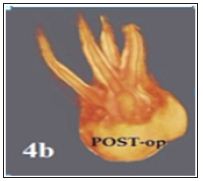
Root canal treatment was performed, using NiTi rotary instruments and a warm gutta-percha filling technique. The canal in the unusual second mesial root was located, negotiated and treated. The canal lengths estimated by the software were confirmed using an apex locator (Apex ID, Kerr Endodontics, Orange, Ca, USA). No intra-operative radiograph was taken. A CBCT post-operative limited-FOV low-dose image, using the same parameters, was taken to assess the quality of the root filling and to ensure the entire canal system was treated (Figure 4b). The access cavity was restored using a flowable, high viscosity, bulk composite (SonicFill, Kerr, Bioggio, Switzerland). After one year the patient remained asymptomatic. A digital radiograph (Gendex GXPS-500, Kavo, Biberach, Germany) taken by the referring dentist did not reveal any signs of periapical pathosis (Figure 1b).
A high proportion of treatment failures in maxillary molars occurs due to the impossibility of locating, instrumenting and filling the second MB canal [17,18]. With the result that many studies have evaluated the presence and location of this canal [2,19-21]. Interestingly, no reports on the actual treatment of a second MB root have been published. In the present case, a second mesial root with its own canal was detected in an unusual palatal position (Figure 2a); such a palatal orifice could have been missed without the use of 3D imaging. The CBCT images and 3D Endo™ Software facilitated the rapid detection of this key morphological feature and allowed the ideal access cavity design for locating and treating all four canals to be visualised pre-operatively. Each CBCT image was equivalent to half the radiation dose compared to an intraoral nondigital radiograph [22]. The 3D rendered images clearly revealed that this root was fused to the main MB root in the coronal region and that the canals in each root had an independent foramen (Figure. 3-4). Post-operative 3D rendered images confirmed the four canals had been shaped and filled, in a more detailed and clear way than traditional radiographs (Figure 1b) For maxillary molars, the usual way of assessing tooth anatomy in case reports has been via periapical radiographs, whereas the more popular method in morphological studies has been CBCT [4]. In a CBCT study [24]. The second MB canal was identified in 48% of the cases, and it was located 2.2 ± 0.54 mm palatally and 0.98 ± 0.35 mesially to the first MB canal. In another study, it was located 2 mm palatally and 1 mm mesially to the first MB canal [5]. In the present case, the orifice of the canal in the second mesial root was located in a very unusual position: 5.99 mm palatally (0.3 mm mesially) to the main MB canal orifice and 7.57 mm mesially from the palatal canal (Figure 2a). On the contrary, the MB, DB and palatal canal orifices were located in the usual position for maxillary molars. Second MB canals can often be managed successfully with the aid of a dental operating microscope [25]. However, the search for its orifice is usually limited to a few millimetres palatally and mesially from the main MB canal: the rationale being to avoid unnecessary weakening of the mesial marginal ridge and palatal cusp. In the present case, an intraoral radiograph did not provide sufficient information for the identification and location of the second mesial root and canal, due to the superimposition of anatomical structures and the impacted third molar.
The use of low-dose CBCT images and new 3D Endo™ Software, allowed rapid, simple and precise preoperative assessment of the second mesial root and canal, thus increasing the quality and outcome of the treatment by avoiding further complications related to a missed root and canal.


