Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Mohit Jai*, Kinjal Mavani
Received: November 29, 2017; Published: December 12, 2017
Corresponding author: Dr Mohit J Jain, Department and hospital of author: Department and hospital of author: Assistant Professor, Department of Orthopaedic, Pravara Institute of Medical Sciences and Rural Medical College, Loni, India; Affiliated Institution: Sanjeevani Multispeciality Hospital, Jetpur, India
DOI: 10.26717/BJSTR.2017.01.000584
Introduction: Operative fixation of distal radius fractures is one of the most commonly performed orthopedic procedures. Though external fixator is a well-established method of treatment for unstable and comminuted fractures, orthopedic surgeons from rural areas of developing countries are still found to be hesitant to use it for various reasons. Aim of our study is to provide an alternate technique for currently used external fixator or distracter modules in limited resources and not to substitute them.
Methods: A total of 32 elder patients with distal radius fractures from a rural hospital were treated with a Non-Spanning Syringe Fixator at a rural hospital which incorporates percutaneous K-wires used to fix distal radius fractures after anatomical reduction. These patients were evaluated for clinical and radiographic outcomes for 1 year and compared with a historical control group of 30 patients with Hoffman II external fixator construct by the same author but at the tertiary center.VAS and DASH scores comparison was also done. Our study results have also been compared with various other known case series for treatment of fracture distal radius by Gartland and Werley score.
Results: Mean radial tilt, 4 degrees; ulnar variance 0 mm and radial inclination angle was 23 degrees at 1 year final follow up. Mean loss of wrist range of motion as compared to normal side was as follows: flexion, 8 degrees, extension, 9 degrees; radial deviation, -1 degrees; ulnar deviation, 2 degrees ; pronation, -1 degrees ; and supination, 8 degrees. Average final DASH score was 9 ranging from 3-14.No statistically significant difference found in radiological and clinical variables or DASH scores between control Hoffman II fixator group and study group of Non Spanning Syringe Distractor. Using the Gartland and Werley score, there were 24 (80%) excellent to good and 6 (20%) fair to poor results which are quite comparable to other landmark studies.
Conclusion: External fixation has advantages over conventional Plaster of Paris cast and pinning in the treatment of unstable extraarticular or simple intra-articular fractures of distal radius. Non Spanning Syringe Distractor provides excellent to good results in majority of our cases. It provides advantages of pinning and fixator both by preventing wrist and hand stiffness and fracture collapse as well. The Simplicity of technique, less operative time, possible in minimal regional anesthesia and cost effectiveness all together makes it very useful for limited resources scenario.
Keywords: Distal Radius Fractures; Hoffman II External Fixator; Non-Spanning Syringe Distractor
Since their description by Abraham Colles, Prof of anatomy and surgery of Trinity college of Dublin in 1814, distal radial fractures remain a therapeutic enigma [1]. In describing patient outcomes of traditional non operative treatment, Colles stated “one consolation only remains, that the limb will at some remote period again enjoy perfect freedom in all its motions and be completely exempt from pain [2].” However, as recent studies emphasize outcomes using patient functional outcome measures, it has been shown that not all patients with distal radius fractures that have been treated non-operatively have had the excellent outcomes as first described by Colles. Unstable distal radius fractures are those which are mechanically prone to re-displacement after closed manipulation resulting in collapse and articular incongruity. Several factors have been associated with the instability [3].
a. The initial displacement of the fracture especially radial shortening.
b. The age of the patient due to osteoporosis.
c. The extent of metaphyseal comminution.
d. The amount of intra-articular comminution and steps.
So if treated with K-wires incorporating cast only, often results in permanent deformity, pain and loss of function [4]. There are various external fixation devices described for this. Often orthopedic surgeons from rural areas of developing countries are found hesitant to use it for the various reasons described below.
Cost factor
a. More operative time.
b. Limited anesthetic facilities.
c. Elder age with comorbid conditions.
d. Low socio economic class with low functional requirements.
e. Iatrogenic complication like infection and stiffness.
f. Associated other injury or fracture requiring priority treatment.
However, Non-Spanning Syringe Distractor provides an alternative option with comparable functional outcome.
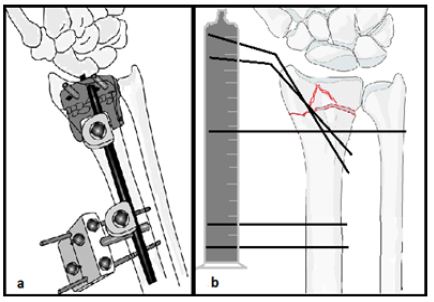
A total number of 32 cases of distal radius fracture treated by Non-Spanning Syringe Distractor from 2015 to 2016 admitted in Primary Level Hospital, India. Ethical committee approval was obtained prior to initiation of the study. All fractures were classified as per the AO classification [5]. Presence of distal ulnar fracture was recorded separately. Our study group was compared with a historical control group of 30 (mean age 61) patients who were operated for Hoffman II type of non-bridging external fixator (Figure 1) between 2015 to 2016 in India and followed up for 1 year by the same author but at the Tertiary Level center.
a. Displaced unstable comminuted fracture of the distal radius, which was defined as any distal radial fracture with more than 20° of dorsal angulation, metaphyseal comminution with or without intra-articular extension, and more than 10 mm loss of radial height
b. Fresh fracture (reported within 7 days of injury)
c. Age >50 years (elder population)
d. Informed consent for operative care.
a. Open fracture
b. Pathological fracture
c. Fractures where adequate reduction was not achieved on operative table
d. Injury severity score (ISS) of >17
e. Ipsilateral upper limb pathology which would affect the functional outcome e.g. arthritis, scaphoid fracture.
All surgeries were performed under regional anesthesia. Once reduction was achieved by ligament taxis, usually 2-3 K-wires (size 2 or 2.5 mm) were used for fixation. Then maintaining the stability at fracture, K-wires were bended carefully by wire bender up to an angle perpendicular to radial shaft. Proximally 1 or 2 threaded K-wires (size 3mm) inserted in distal radial shaft in dorso-lateral plane 4-5 cm proximal to fracture level depending upon fracture pattern and quality of bone. Distal ulno radial trans-fixation k wire if used for distal radio ulnar joint instability can also be used for distraction purpose if provides enough length. Length of K-wires were cut approximately 4-5 cm away from the skin making them blunt for fixation inside syringe. Under the image intensifier, the required distraction was applied across the wires, and approximate length judged by scale for hole making in syringe. A 5 or 10 cc plastic syringe used as distracter after drilling holes in one plane by similar sized K-wire over T handle. This makes opposite surface of holes as shield covering blunt cut ends of K wires. All the patients were given below elbow plaster (slab) applied meticulously by cotton bandage and soft paddings (Figure 1).
Figure 1: Technical diagram of (a) Hoffman II construct (B) Non Spanning Syringe Distractor.
An active range of motion at hand, elbow and shoulder was encouraged. Most of the patients could hold a cup of tea within next day of surgery and felt comfortable with the fixator. Oral antibiotics were given for 5 days. Slab was substituted by crape support at 4 weeks in all the patients to enhance early active wrist mobilization. Syringe distracter was removed at 6th to 7th week of surgery depending on the clinical and radiological signs of the union. Check X-rays were taken on 2nd week of the fixation, at the time of removal of the fixator and on subsequent follow-ups at 3 and 6 months and 1 year. Radiological and clinical outcomes were compared with control group of Hoffman II fixator. The total upper extremity function was assessed by self-evaluation, using an American translation of the original German DASH ranging from 0 (no disability) to 100 points (full disability).We recorded the degree of pain using VAS (Visual Analogue Score). Our study group outcome were accessed by Gartland and Werley score and compared with various standard case series of different modality for similar fracture [6] (Figures 2 & 3).
Figure 2: Case 1 of Non Spanning Syringe Distractor.
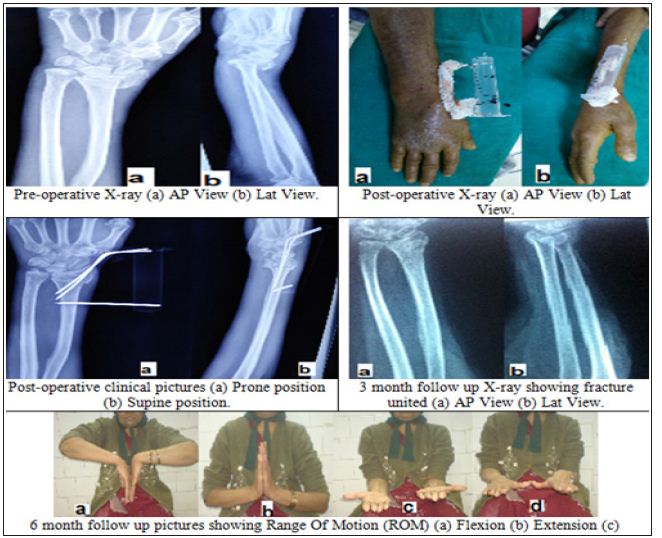
Figure 3: Case 2 of Non Spanning Syringe Distractor.

A sample size calculation showed that in order to show a difference with a 5% significance level and 80% power, 30 individuals in each group would be needed for radial tilt as outcome, while more than 8,000 individuals would be needed with inclination as the outcome. The mean differences, 95% confidence intervals and p-values for comparisons of the mean values at pre and postoperatively, at time of removal at 6 week and at 1 year follow-up when evaluating anatomical measures and at 6 week, 3 month, 6 month and 1 year follow-ups when evaluating functional measures. We considered p-values less than 0.05 to be statistically significant.
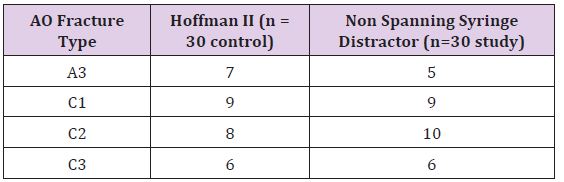
Out of 32 one patient died and one lost follow up reducing sample size to 30 same as comparison group. The mean age of patients treated was 62 years as compared to 61 years of control group. The patients were predominantly males (60%) in both groups. The dominant hand was injured in 21 (70%). Domestic falls followed by road traffic accidents were the predominant (>80%) modes of injury. Fractures belong to A3 or C1-3 class according to AO classification (Table 1).All the fractures were united within 3 months. 4 patients had pain mainly due to prominent ulnar styloid secondary to malunion or DRUJ instability. Wrist and finger pain and stiffness significantly improved after physiotherapy except in one due to Reflex Sympathetic Neuropathy (RSN). One out of two diabetic patients had developed pin track infection, which was healed subsequently. No one developed radial neuritis.
In the dental restorations, specific resin systems are applied to the damaged tooth area to form a cast restoration that is then heat-treated using special ovens under controlled laboratory conditions. The ideal temperature for heat treatment application depends on the thermal behavior of each composite, such as glass transition temperature (Tg) analysis and initial degradation temperature [7]. The Tg can successfully be used as a reference to sign the ideal heat treatment for photo-irradiated resin composites. Above Tg, the secondary molecular interactions are weakened and, as a consequence, material properties are optimized once trapped radicals are given the opportunity to react [8-9]. In addition, the maximum temperature for heating without damaging, i.e., initial degradation temperature, needs to be determined to avoid weight loss [10]. In the present investigation, Conventional TG-DTA is a powerful and convenient thermal analysis technique which allows various important physical and chemical transformations such as glass transition and degradations are examined (Figures 1-4). Glass transition temperature (Tg) and number of phase transitions are evaluated for different dental materials are shown in Table 1.
Table 1: AO classification of fractures.
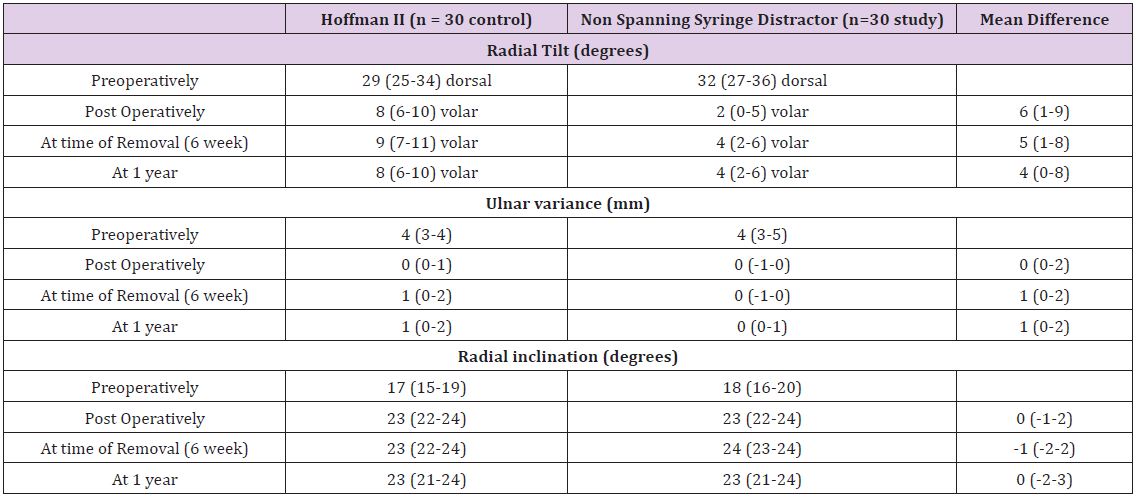
Anatomical assessment: Preoperatively, the median radial tilt was 29 degrees of dorsal angulation in the group and 32 in the Non Spanning Syringe Distractor group. Postoperatively, the median tilt was 8 degrees of volar angulation in the Hoffman II group and 2 degrees volar in the Non Spanning Syringe Distractor group (p = 0.002). At the time of removal of the fixators, there was still a statistically significant difference in radial tilt: 9 degrees of volar angulation in the Hoffman II group and 4 degrees in the. Non Spanning Syringe Distractor group (p= 0.04). At 1 year, the difference was no longer statistically significant. For the other anatomical variables, no statistically significant differences were found (Table 2).
Table 2: Comparison of radiological assessments, mean (95% CI).
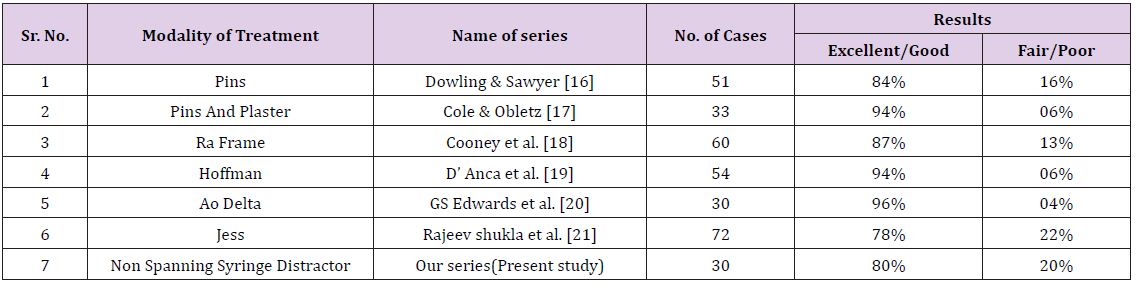
Functional assessment: At 6 weeks, the mean loss of flexion was 24 degrees in the Hoffman II group and 34 degrees in the Non Spanning Syringe Distractor group (p = 0.001). At the other times, the differences between the groups were not statistically significant. There were no statistically significant differences between the groups concerning loss of extension, radial and ulnar deviation, supination, or pronation at the different times (Table 3). There were no statistically significant differences in mean values of the VAS score between the groups at any time (data not shown). At 1 year, the mean (CI 95%) DASH score was 9 (3–14) in the Hoffman II group and 13 (8–20) in the Non Spanning Syringe Distractor group. According to Gartland and Werley score, 24(80%) excellent to good and 6 (20%) fair to poor results were achieved by Non Spanning Syringe Distractor. These results are also compared with different other landmark studies (Table 4).
Table 3: Comparison of functional assessments by mean (95% CI) loss of movement (in degrees) in the injured wrist compared to the uninjured wrist.
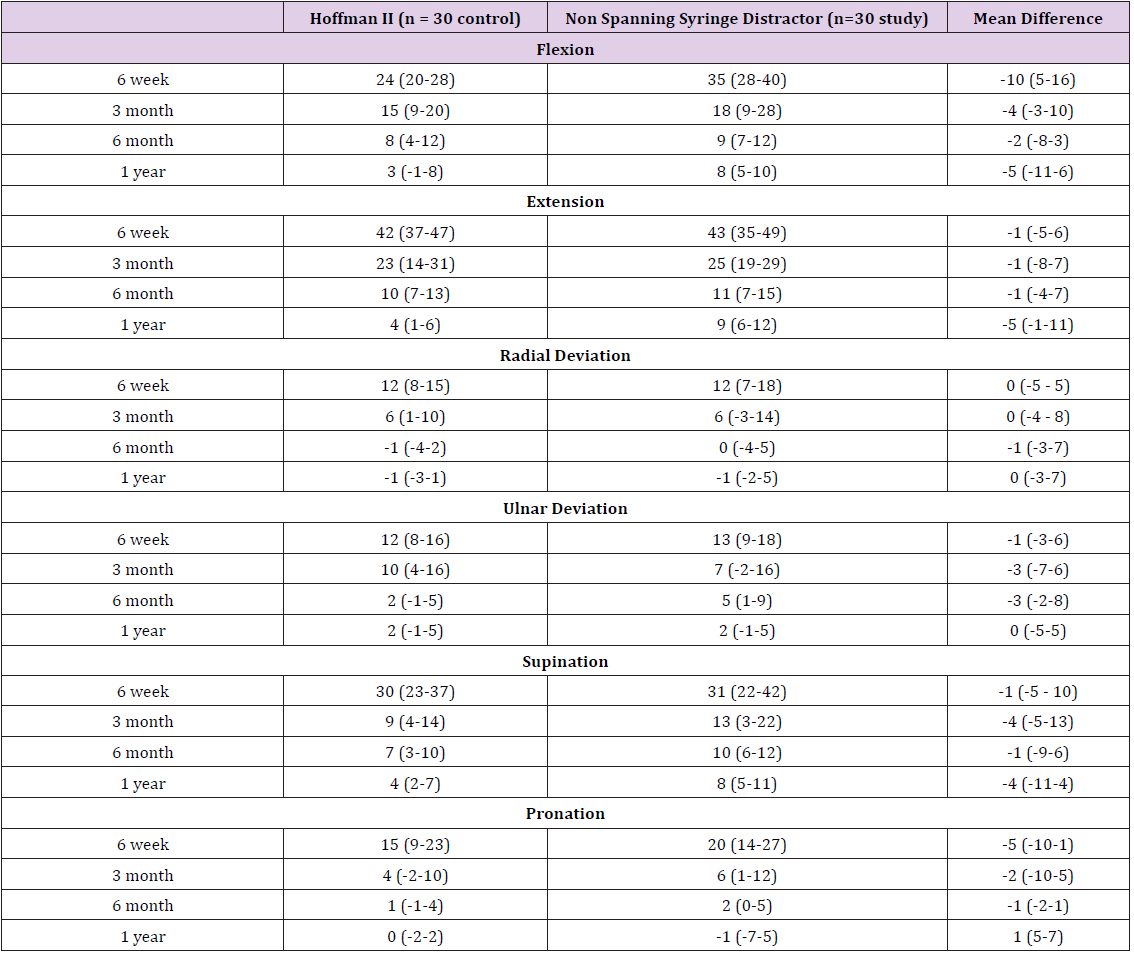
Table 4: Comparison of various study results (functional).
The fracture of distal end radius is the most common fracture we treat. Management of fracture distal end of radius is still a challenge for orthopedic surgeon and pose therapeutic problem in term of reduction of fracture, maintenance of reduction till the fracture unites mobility of the joint after fracture union. Moreover outcome of these fractures is not uniformly good regardless of treatment instituted. We agree with D.L. Fernandez et al that a good functional result usually accompanies a good anatomical reduction [7]. Collapse, loss of palmar tilt, radial shortening, and articular incongruity is frequent after closed treatment of unstable and comminuted intra-articular fractures of the distal radius and these often results in permanent deformity, pain, and loss of function [8]. Hence, skeletal fixation to maintain the reduction has been recommended [9]. The incorporation of transfixing Kirschner wires (K-wires) within the plaster or use of external fixation is being used for comminuted fractures. Many external fixation devices are described to achieve reduction and fixation of the fragments without loss of position and acceptable functional results [10]. Although the first description of an external fixator in the treatment of forearm fractures by Ombrédannein 1929 was of a non-bridging device, standard technique involves and current texts describe bridging constructs that cross and necessarily immobilize the wrist during the bony healing process [11]. The ligamentotaxis is the basic principle used by external fixation [12]. Prolonged rigid immobilization of the wrist in spanning external fixator leads to decreased blood supply to bone and soft tissues and causes periarticular fibrosis. This leads to osteoporosis, poor motion, and compromised functional outcome.
The early mobilization of the wrist leads to normalization of blood supply, hastened functional recovery, earlier resolution of wrist swelling, and decreased joint stiffness [2,4,8]. The dynamic external fixators have also been developed to provide mobilization of the wrist while reduction and fixation are maintained [13]. One such fixator was first designed by Penning (1990) [14]. The device allows wrist flexion by a hinge joint, with the center of motion being at the capito-lunate joint. This is based on several anatomic and biomechanical studies by Short WH et al. [15]. Our case series attributes to 24(80%) excellent to good and 6(20%) fair to poor results, which are quite comparable with all other landmark studies. No statistically significant difference found in radiological and clinical variables or DASH scores between control Hoffman II fixator group and study group of Non Spanning Syringe Distractor. Thus we believe that Non-Spanning Syringe Distractor is an alternative mechanical device especially for those who are prompted to not to use external fixator because abovementioned reasons. It combines the advantages of pins only and wrist spanning external fixator preventing their disadvantages at the same time.
Finally we would like to conclude that Non-Spanning Syringe Distractor is an easy, cost effective and reliable treatment in treating intra articular and unstable extra articular distal end radial fractures where limited resources in rural part of developing country prompt the orthopedic surgeons to opt for more conservative modality of plaster +/-pins and more frequently complicated by collapse and mal-union. We recommend this device as an alternative method to the currently used modalities and not as a superior substitute .We cannot pretend to present well-objectified functional result unless controlled multicenter trial in larger patient group, but can confirm the feasibility of the Non Spanning Syringe Distractor technique.


