Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Yasir Mohib1*, Pervaiz Hashmi2, Muhammad Atif3, Haroon Ur Rashid2 and Waseem Ahmed1
Received: November 15, 2017; Published: December 01, 2017
Corresponding author: Yasir Mohib, Instructor orthopedics AKUH, Karachi, Pakistan
DOI: 10.26717/BJSTR.2017.01.000560
Introduction: Kienbock’s disease is a form of osteonecrosis of lunate, first described in 1910 by Robert Kienbock. It occurs most commonly in men aged 20 to 40 years of age. Its exact etiology is still under study but most hand surgeons believe to be a multi-factorial origin and some time establishing the diagnosis is a challenge especially in unaccustomed hands. Management of Kienbock’s disease is focused on alleviating pain and halts the worsening disease process [1]. Our study aims to determine the functional and radiological outcome after surgery for Kienbock’s disease.
Objective: To determine the functional and radiological outcome after surgery for Kienbock’s disease.
Methods: The retrospective review of patients managed operatively for Kienbocks disease at Aga Khan University Hospital Karachi. Kienbock disease was classified according to Lichtman and Ross Classification. Patients underwent various procedures including surgical decompression and vascular bone grafting, etc. Radiological variables and outcomes were assessed.
Results: Of the 7 patients, 3 (42.9%) were men and 4 (57.1%) women. The right side was involved in 5(71.4%) patients, and 2(28.6%) had a left sided Kienbock disease. Duration of symptoms ranges from 8 months to 84 months with mean 31.12 +/- 26.63. Post operative x-rays 6 months follow up which showed Ståhl index minimum 0.29 to maximum 0.45 with mean 0.36 (sd .055), Nattrass index ranges from 0.76 to 1.74 with mean 1.4 (sd 0.31) and Radioscaphoid angle varies from 46.3 to 60.6 with mean 51.7 (sd 5.4).
Conclusion: We concluded that revascularization procedures are effective treatment in stage II and IIIa. Limitation was limited number of patients which encourage multi-centre trial to prove the efficacy of treatment.
Kienbock’s disease is a form of osteonecrosis characteristically affecting the lunate, first described in 1910 by Robert Kienbock who identified the changes in the proximal portion of the lunate and affecting the radiolunate articulation [2]. It is characterized by lunate sclerosis, cystic changes, fragmentation and articular surface collapse on plain radiograph [3,4]. It occurs most commonly in men aged 20 to 40 years of age. Its exact etiology is still under study but most hand surgeons believe to be a multi-factorial origin and some time establishing the diagnosis is a challenge especially in less experienced hands [5]. Litchman et al. [6] provided four progressive radiological stages of the disease which can be used access the progression of disease. Management of Kienbock’s disease is focused on alleviating pain and halt the worsening disease process [7]. Various standard modalities are used to treat this disease, including nonsurgical management, vascularised bone graft (VBG), joint levelling procedures, intercarpal arthrodesis, proximal row carpectomy and total wrist arthrodesis [8,9]. Gupta et al in 2014 presented their experience in 12 patients and found improvement in the functional outcome after treatment [3]. Our study aims to determine the functional and radiological outcome after surgery for Kienbock’s disease.
The retrospective review of patients managed operatively for Kienbocks disease from January 2005 to December 2015 at Aga Khan University Hospital Karachi. All adult patients with radiological evidence of Kienbocks disease were included. Kienbock disease was classified according to Lichtman and Ross Classification of Lunate osteonecrosis. Patients underwent various procedures including surgical decompression and vascular bone grafting, carpel fusion and iliac bone grafting, radial shortening, and external fixator. Radiological variables and outcomes were assessed by viewing appropriate pre-operative, post-operative and 6 month follow-up radiographs. Stahl index, Nattrass index and Radioscaphoid angle were calculated. Data was analyzed using SPSS 20.
Of the 7 patients, 3 (42.9%) were men and 4 (57.1%) women. The right side was involved in 5 (71.4%) patients, and 2 (28.6%) had a left sided Kienbock disease. Duration of symptoms ranges from 8 months to 84 months with mean 31.12±26.63. According to Lichtman and Ross Classification of Lunate osteonecrosis, stage II had 3, stage IIIA had 1, stage IIIB had 2 and stage IV had 1 patient. Three patients with stage II were underwent decompression of lunate bone and vascular bone grafting, in stage IIIB one patient had radial shortening and vascular bone grafting and 2nd patient underwent lunate decompression and bone grafting with unilateral external fixator application, stage IV patient had wrist reconstruction with carpel fusion with iliac bone grafting. Postoperatively patients were immobilized with splint for 6 weeks with exception of patient with external fixator (Tables 1 & 2).
Table 1: Characteristics of patients in the present study (n = 7).
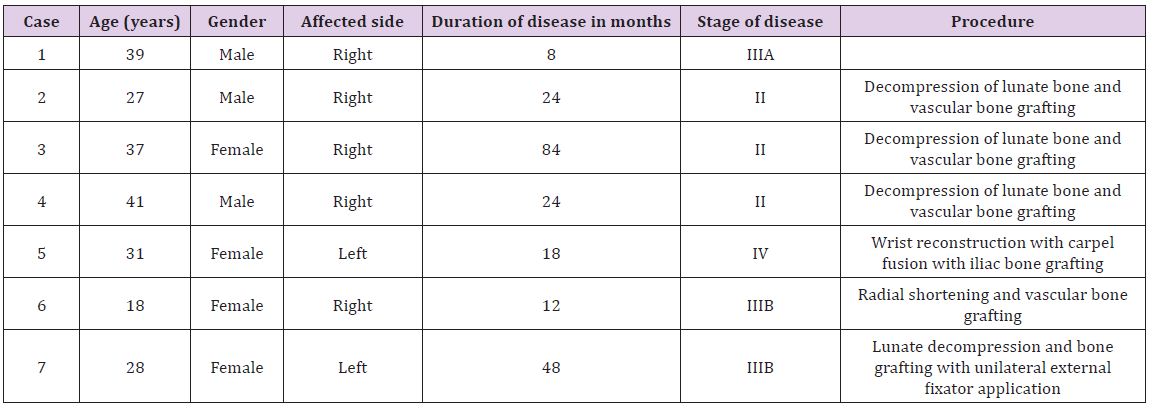
Table 2: Radiological outcomes of patients in the present study (n = 7).
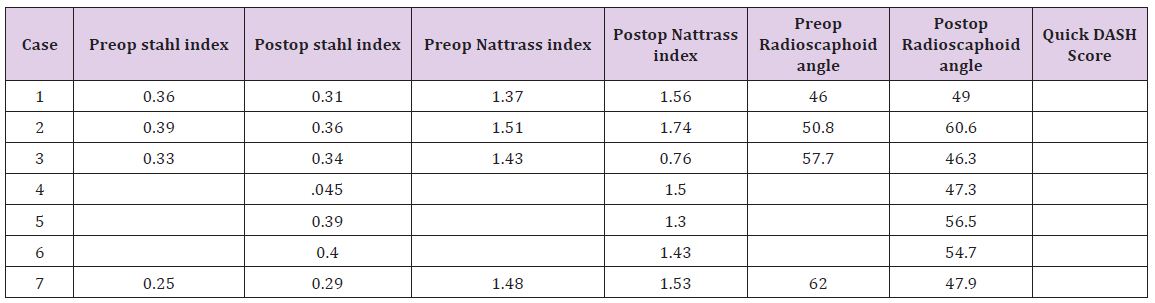
Post operative 6 months follow up x-rays which showed Ståhl index minimum 0.29 to maximum 0.45 with mean 0.36 (sd .055), Nattrass index ranges from 0.76 to 1.74 with mean 1.4 (sd 0.31) and Radioscaphoid angle varies from 46.3 to 60.6 with mean 51.7 (sd 5.4). One of our patient developed persistent wrist pain and later on diagnosed as Osteoid osteoma. Two and half years later we did curettage with bone grafting. Patient treated with no recurrence.
Kienbock disease though very rare but presents with agonizing wrist pain affecting the life of working individual. Situation would be more worrisome if they end up in primary care physicians. The radiographic findings don not correlate to the severity of symptoms [1]. A recent meta analysis showed subjective pain relief in all patients whereas object improvement in grip strength and range of movement in all patients treated surgically either joint levelling surgeries or VBG [1]. Our study also showed improvement with joint levelling procedures for negative ulnar varience. Impairment of vascularity is also thought be part of disease process and vascularised bone grafting, which could be expected to restore the biological environment. In our study 5 patients who received vascularised bone grafting showed improvement [10]. One of our patient developed persistent wrist pains one year post operatively and later on diagnosed to be Osteoid osteoma. He was managed by curettage with bone grafting. Due to very limited disease volume evaluation of multicentre data may help enhance better understanding of the disease. Though the present study is small case series we found decompression and vascularised bone grafting has provided promising results.
We concluded that revascularization procedures are effective treatment in stage II and IIIa. Limitation was limited number of patients which encourage multi-centre trial to prove the efficacy of treatment.


