Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Miguel Prestes Nácul*, Marcelo Velloso Fabris and Ricardo Gonçalves Da Costa
Received: October 10, 2017; Published: November 06, 2017
Corresponding author: Miguel Prestes Nácul, Minimally Invasive Surgery Institute of Education and Research Moinhos de Vento Hospital - Porto Alegre, Rua dos Andradas, 1781/404, Bairro Centro CEP 91410-001 - Porto Alegre, RS, Brazil
DOI: 10.26717/BJSTR.2017.01.000497
Introduction: Intestinal obstruction by a gallstone (biliary jejunum) is an uncommon and potentially serious omplication of chronin cholecystitis. Ileum gallstone represents 25% of non-strangulation obstructions in the small bowel causing 1% to 3% of all obstruction surgeries. Biliary ileum located in the proximal jejunum is a rare condition and the treatment post minimum invasive technic tends to be the best therapeutic option when available.
Material and Method: case report of 87 years old female diagnosed with duodenum biliary post acute cholecystitis.
Results: After frustrated attempt of gallstone removal by upper digestive endoscopy, the gallstone migrated to proximal jejunum. After observation expecting for the gallstone to evolve through the small bowel, surgery was opted due to the obstrucion maintenance. The patient was submitted for a videolaparoscopy to remove the 4 cm gallstone by enterotomy and enterorrhaphy. No complications were presented after surgery.
Conclusion: The option for a videolaparcopy approach showed effective, even more in a elderly patient in a matter of fact of decrease morbidity and mortality related to the abdominal wall.
Keywords: Biliary Jejunum; Chronic Cholecystitis; Videolaparoscopy
Abbreviations: JB: Jejuno Biliar; CT: Computed Tomography
Gallstone intestine obstruction, named by jejunobiliar (JB) ia an uncommon complication and a potentialchronic cholecystitis [1]. The autors presente a case of obstructive bowel by a gallstone located in the proximal intestine in a 87 years old patient with cholecystitisntreated by minimally invasive approach.
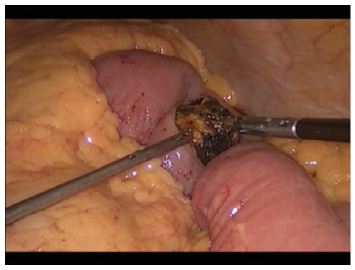
Female, 87 years old with symptomatic cholecystitis interned in the hospital emergency with abdominal pain and vomit. Blood count presented an importante leucocytosis. Total abdominal ultrassonography was performed indicating gastric cavity distension containing residue in it’s interior; gallbladder non dilataded bile ducts (common bile duct measuring 0.5cm of diameter). A abdominal computed tomography (CT) identified a large gallstone in duodenal bulb interior in the first duodenal portion confluence, measuring between 2,5 to 3,5cm in it’s axial axis (Figure 1). The patient was submitted by an upper digestive endoscopy to remove the gallstone, wich was not successful (Figure 2). The gallstone migrated for the third duodenal portion (Figure 3). It was decided for a non opertative treatment, expecting the gallstone to decrease it’s volume through endoscopy manipulation and evoluing without surgery approach. On the sixth day of hospitalization, as the patient persisted with drainage of gastrointestinal secretion by naso-gastric probe, was performed another abdominal CT (Figure 4) demonstrateing a gallstone in the proximal jejunum It was opted foa a surgeric approach. The patient was submitted to a videolaparoscopy wich identified a gallstone in the proximaljejunum 10cm after the Treitz angle. The gallstone was removed by enterotomy (Figure 5). Cholecystectomy was not performed in this procedure. The patient presented a good postoperative evolution, being discharged in the second postoperative day.
Figure 1: Abdominal CT - 1st day.

Figure 2: Upper gastric endoscopy gallstone extraction attempt.

Figure 3: Abdominal CT - 3rd day.

Figure 4: Abdominal CT - 6th day.
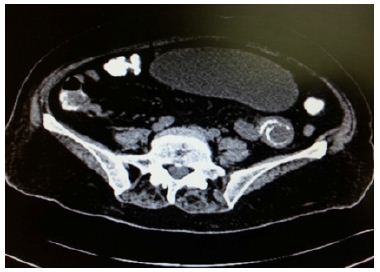
Figure 5: Gallstone removal by videolaparoscopy enterotomy.
JB, for the first time described by Bartholin in 1654 [1,2] refers to an obstruction of any segment of gastrointestinal tract by gallstone [3]. It’s incidence is between 0,3% to 0,5% of gallstone carriers [4]. For a obstruction in intestinal lumen, the gallstone must have more than 2, 5cm [5]. Elderly are mostly affected, usually the the female gender, besides the obese probably due to a higher incidence of biliar lithiase [3,6,7]. JB occurs by a fistula formation between tha gallbladder and another small intestine segment making possible the passagem ofone or more gallstones wich can obstruct the intestinal transit specially in narrowing anatomical áreas like the Treitz angle and the ileocecal valve [4,8].
The gallstone migrates to the small intestine normally by a cholecystitis fistula. The obstruction can occur in any part of the ileus intestine (60,5% of cases), jejunum (16%), stomach (14,2%), colon (4,1%) and duodenum (3,5%) [6]. The patient can presente itself with inespecific symptoms or signs of intestine obstruction such as nausea, vomit, distension and abdominal pain [3,9]. Despite being unusual in the population JB responds for 25% of no strangulation obstruction [6,8] being related to the age progression.
It’s responsible for 1% to 3% of all surgeries of bowel obstructions [1,8]. Mortality associated to intestinal lumen obstruction caused by gallstone veries between 12% to 27% [6]. The image exame goal in the evaluation of a suspect clinical condition of JB is to specifiy the diagnosis in an effort to dermine the ideal surgery treatment. CT is the most efificient exame due to it’s agility and it’s image resolution [10]. The dissemination of it’s use enhence the diagnosis to 99% [9]. Flexible endoscopy can help both diagnosis and small gallstone extraction. Despite being less invasive the gallstone extraction can fail if the gallstone is too big [11]. JB surgeric treatment is usually done in matter of urgency. The surgery options are enterolithotomy and cholecystectomy and fistula repair in the inicial approach when used one stage surgery or enterolithotomy with cholecystectomy only after the patiente recovery when two stage surgery [12,13]. Is wise designate the one stage surgery for patients clinically stable and the two stage surgery for patients with severe cholecystitis and high risk perioperative degree [13].
Mortality rate in one stage procedure is 16,9% and two stage is 11,7% for enterolithotomy [14]. The main complications of JB surgeric treatment are: infection, pneumonia and evisceration. Mortality rates varies from 5% to 25% in larger studies [3]. Recently studies demonstrate that morbimortality in patients with JB decrease when antibiotics and intensive care are applied [3]. Videolaparoscopy surgery enable a better recovery postoperative [3,15,16]. In the reported case the gallstone removal by flexible endoscopy was not possible due to gallstone’s size and because of absence of technological device to crack the gallstone. Non surgical treatment posteriorly proposed aimed avoid a duodenal surgery exploration, mainly in it’s third and forth portions with a complex access. In the moment in wich the gallstone positioned itself in the jejunum and was clear that it’s evolution in the digestive tract would be slowly because of it’s size, was indicated it’s removal by videolaparoscopy, wich is technically simple and well succed. Nonperformance of cholecystectomy was due to a lack of symptoms related to a biliar lithiasis beyond wich in a matter of fact was already treated by a wide cholecystitis fistula.
JB treatment by minimally invasive surgery approach is interesting once the desease express by an acute condition of intestinal obstruction commonly in patients with other comorbities. However the use of flexible endoscopy techniques and videolaparoscopy depend on training and proper technologial equipament.


