Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Metin Okşul1, Yusuf Ziya Şener1*, Cem Çöteli1, Burcu Ancın2 and Kenan Övünç1
Received: August 27, 2017; Published: September 11, 2017
Corresponding author: Yusuf Ziya Şener, Department of Cardiology, Hacettepe University Faculty of Medicine, Turkey
DOI: 10.26717/BJSTR.2017.01.000344
Dextrocardia is a rare clinical condition and usually accompanies with additional cardiac anomalies and ciliary dyskinesia syndromes. Intrathoracic space occupying pathologies can cause pseudodextrocardia. Herein we present a patient with pseudodextrocardia secondary to pneumothorax
Dextrocardia defines rightly positioned heart and its incidence ranges between 1/8,000 – 1/25,000. Patients with dextrocardia are classified into situs solitus, situs inversus and situs ambiguous according to the positioning of the visceral organs. Dextrocardia usually presents with additional cardiac anomalies especially in patients with situs solitus [1]. Pseudodextrocardia is a clinical condition that heart is dextroposed secondary to intrathoracic space occupying pathologies. There are two cases with pseudodextrocrdia in the literature one of which is due to bronchectasia and the other one ise due to diaphragmatic hernia [2,3]. Herein we present a young male patient with pseudodextrocardia due to spontaneous pneumothorax.
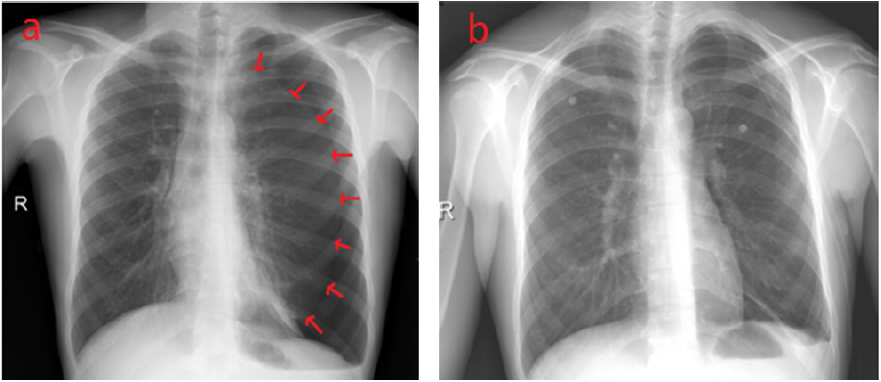
Figure 1: a) Pneumohorax line can be seen at the left side. b) Re-expansion of the left lung and migration of heart to the normal localization is seen.
A 19 years old male patient without any known diseases and drug use was referred to our department from another hospital due to the suspicion of dextrocardia. It is learnt that he had admitted to that hospital with the complaints of stinging type chest pain and dyspnea lasting since two weeks before. It was realised that his heart sounds could be heard best at his right hemithorax and his heart was positioned rightly at chest x-ray. His medical history revealed no diseases and substance use except smoking. His vital signs were all in normal range. His heart sounds was really could be heard best at the right hemithorax and his lung sounds couldn’t be heard at left hemithorax. Hyperresonance at the left hemithorax was also detected by percussion. His complete blood count, kidney and liver function tests were normal. Chest x-ray was performed and pneumothorax at the left side with rightly positioned heart was established (Figure 1). The patient was urgently consultated with Thoracic Surgery Department and thoracostomy tube was placed. After his left lung expansion, his complaints resolved and heart image came to the normal position (Figure 1). He was discharged after thoracostomy tube was displaced and referred to Pulmonology Department to evaluate either there is any underlying lung disease.
Primary spontaneous pneumothorax (PSP) which is more frequent in males two to three folds than females is seen usually among young patients with peak incidence at second decade.Smoking, familial predisposition and rapid changes of atmospheric pressure are the main risk factors for PSP. Emphysematous bullae or blebs, known as emphysematous like changes are seen in more than 80% of patients. Sudden onset chest pain and dyspnea is the most common presentation type. Close follow up without intervention can be an option in patients with mild pneumothorax while thorax tube insertion and air drainage should be prefferred in more serious cases [4]. To the our knowledge, this case is the first pseudodextrocardia case due to pneumothorax. PSP should come to mind in all practitioners who face with a young male paitent suffering from stinging type chest pain and dyspnea. This case also shows us again the importance of complete physical examination.


