Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Andreoletti, Désirée Moharamzadeh*, Davide Molisani, Giorgio Piarulli and Costante Emanuel Grismondi
Received: July 28, 2017; Published: August 22, 2017
Corresponding author: Désirée Moharamzadeh, Department of Orthopedics and Traumatology, Policlinico San Marco, Corso Europa 7, Osio Sotto (BG), Italy
DOI: 10.26717/BJSTR.2017.01.000292
Background: Amongst the different techniques for scaphoid non-union, the Matti-Russe procedure is a simple method where a corticocancellous bone graft from the iliac crest is packed in the scaphoid. A variant of the technique used in our Department involves a longer incision and bone graft from the radius. Aim of the study was to evaluate the outcome of our variant of the Matti-Russe procedure for scaphoid nonunion.
Materials and Methods: During a 30-year period (January 1986-June 2016), 29 patients referred to our Hospital with a scaphoid nonunion and underwent our modified Matti-Russe procedure. We sampled 16 patients (14M; 2F) with complete data who referred consecutively between January 2000 and June 2016 (age range: 15.6-59.8 years; average 34 years). Scaphoid non-union was classified according to Alnot. Post-operatively the wrist and thumb were immobilized in a cast for 6 weeks. Patients’ outcomes were assessed at 4-months and at 12-months post-op using the Mayo wrist score (MWS) questionnaire. Average follow-up was 18.4 ± 5.6 months.
Results: Of 16 patients, 14 (87.5%) had good clinical and radiological outcome with union after 4.9 months. The MWS scores at 4-month and 12-month follow-up were respectively: excellent in 4 (25%) and 8 (50%) patients; good in 9 (56.3%) and 6 (37.5%) patients; satisfactory in 3 (18.8%) and 2 (12.5%) patients.
Conclusion: Our variant the Matti-Russe procedure is a valid procedure, with a high union rate and has a further advantage of being less invasive. Our post-operative shorter time of immobilization leads to an improved range of motion and excellent and good MWS scores.
Scaphoid fractures are a common type of fracture, accounting for up to 70% of carpal fractures [1,2], which occur frequently after a fall on the outstretched hand (hyperextension of the wrist joint). Usually patients present pain, with tenderness in the snuffbox, and limitation of movement especially in extension and radial deviation. A delayed diagnosis and subsequent delayed treatment may lead to avascular necrosis and non-union (up to 10% of fractures), mostly when there is involvement of the waist or the proximal pole of the scaphoid, due to its compromised vascularization [3,4]. A wide range of methods have been described for the treatment of these fractures, which comprise non-surgical (electostimulation) [5] and surgical techniques (open reduction, internal fixation with a screw and bone grafting) or a combination of both [6-10]. The aim of the surgical treatment is to correct the deformity, in order to avoid the carpal collapse and radiocarpal osteoarthritis. The rate of success of surgical fixations for scaphoid non-union is around 70% up to 90% [11,12]. When conventional non-vascularized bone grafting fails, due to a complete necrotic proximal pole, vascularized grafts may be used, which possess angiogenic and osteogenic factors [13- 15]. Amongst the different techniques, the Matti-Russe procedure is a simple method, described by Hermann Matti in 1937 [16,17] and later modified by Otto Russe in 1960 [18]. In the past it was a widely applied method and involves a volar incision, lateral to the flexor carpi radialis; the non-union site is exposed and a cavity extending to adjacent fragments is created. A cortico-cancellous bone graft taken from the iliac crest is packed in the corresponding trough in the scaphoid. A variant of the technique used in our Department involves a slightly longer incision proximally and a bone graft taken from the distal volar portion of the radius, rather than from the iliac crest. In this study we decided to evaluate the outcome of our variant of the Matti-Russe procedure for scaphoid non-union.
During a 30-year period between January 1986 and June 2016, 29 patients referred to our Hospital with a scaphoid non-union and underwent our modified Matti-Russe technique. Of these patients, during the period between January 2000 and June 2016 we sampled retrospectively 16 patients (14 M; 2 F) with complete data, with an age range between 15.6 and 59.8 years (average age: 34 years), who referred consecutively to our out-patient dedicated clinic, with a diagnosis of non-union of a scaphoid waist fracture, documented by x-rays (standard antero-posterior, lateral, oblique and 30° ulnar deviation radiographs), which occurred on average 11.6 months before. The non-union of the scaphoid was classified according to Alnot classification [19]. All patients underwent MRI of the hand/wrist at the moment of diagnosis. Inclusion criteria: patients with complete clinical and radiological data, with a documented scaphoid waist fracture; Grade II according to Alnot. Exclusion criteria: patients with simultaneous fractures of other carpal bones; Grade III and IV according to Alnot; radiologically documented scapho-lunate dissociation.
The surgical procedure is our variant of Matti-Russe procedure with cortico-cancellous bone graft from the distal volar portion of the radius, always performed by the same surgeon. Informed consent of each patient was obtained. Post-operatively the wrist and thumb were immobilized in a cast for 6 weeks, and subsequently the cast was removed and mobilization initiated. Average time to radiological union for all fractures is nine weeks [20,21], therefore patients’ functional outcomes were assessed 4-months and 12-months post-op approximately using the Mayo wrist score (MWS) questionnaire which consists of questions assessing pain intensity, functional status, range of motion and grip strength. Scores are recorded in 4 groups: 90-100: excellent; 80- 90: good; 60-80: satisfactory; <60: poor. Serial x-rays were taken to asses radiographic union at 4-months and 12-months postop.
Figure 1: Surgical technique (i)-(ix).
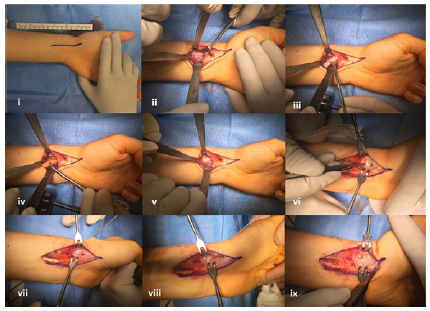
Our variant of the Matti-Russe procedure involves i) a slightly curved volar 6-8 cm incision, centered on the radial styloid process, lateral to the flexor carpi radialis tendon (protecting the superficial branches of the radial nerve), prolonged proximally on the distal portion of the radius; longitudinal incision of the palmar joint capsule and retraction of the volar radio-carpal ligaments (radioscapho- capitate and radio-lunate ligaments). ii-v) In the distal volar portion of the radius a rectangular-shaped cortico-cancellous bone graft of approximately 2 cm x 0.5 cm is harvested; vi) the non-union site is more easily accessible after dorsiflexion of the wrist, and,when exposed, all the fibrous tissue and sclerotic/necrotic bone must be removed and the underlying cancellous bone revealed; vii-viii) a similar rectangular cavity is created with a dedicated burr in the scaphoid (along its longitudinal axis). ix) The trough is then packed with the cortico-cancellous graft as it has to be filled completely in order to guarantee an appropriate distraction and therefore restoration of the height of the scaphoid. The stability of the graft is tested with flexion and extension movements of the wrist. Suture of the capsule and the radio-carpal ligaments. Postoperatively the wrist is immobilized in a short arm thumb spica cast, with the thumb in abduction, and the cast is removed after 6 weeks, when the mobilization is initiated.
In our study, we collected data on 16 patients with scaphoid non-union, all treated with our modified Matti-Russe procedure. Fourteen were men (87.5%) and two were women (12.5%). All non-unions were classified radio graphically as Grade II according to Alnot. MRI documented a vascularity of the proximal pole in only 1 male patient, who subsequently underwent 2 years later a four-corner fusion for a necrosis of the proximal pole. The average follow-up duration was 18.4 ± 5.6 months.
Of 16 patients, 14 (87.5%) had no complications; the 2 complications we had were:
A. A male patient developed a necrosis of the proximal pole and needed further surgery;
B. A female patient with a good radiological outcome with a scaphoid union, developed a CRPS 1 which required physical therapy.
Table 1: Patients’ MWS pre-op, 4 months post-op and 12 months post-op.
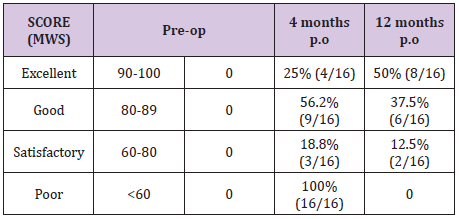
The functional scoring system used was the Mayo Wrist Score. The scores at 4-month and 12-month follow-up were respectively: excellent in 4 (25%) and 8 (50%) patients; good in 9 (56.3%) and 6 (37.5%) patients; satisfactory in 3 (18.8%) and 2 (12.5%) patients. We had no poor results (Table 1). Radiographic union was considered when there was evidence of trabeculae crossing the non-union site on standard antero-posterior, lateral, oblique and 30° ulnar deviation radiographs. In 15 patients we had a scaphoid union after 4.9 months.
Amongst the various surgical options for the treatment of scaphoid non-union, the cortico-cancellous bone grafting technique according to Matti-Russe is one of the most commonly used. Mulder [22] is probably the first Author to use the term “Matti-Russe” in 1968 to describe the technique which includes suggestions from both authors. In 1937 Herman Matti [16] suggested a dorsal radial approach to the non-union site and a cancellous bone graft harvested from the greater trochanter; Otto Russe [18] in 1960 proposed a few modifications regarding the surgical approach and the type of graft. Firstly, he suggested the palmar approach in order not to damage the vascularization and, secondly, a cortico-cancellous graft harvested for the iliac crest. The cortical portion is important for the process of osteoinduction (bone cell differentiation), due to the presence of BMP (Bone Morphogenetic Protein), whilst the cancellous paortion is necessary for osteoconduction (bone growth).
The Matti-Russe technique has uncountable advantages, which include mainly the high rate of success, ranging from 81% to 97% of bony union [4,22-24] confirmed also by our results, where the bony union rate was around 94%. In a study, Raju P et al. [25] compared three different surgical techniques: Herbert screw fixation, Matti- Russe bone grafting and Kohlman modification of the vascularized muscle pedicle graft procedure. Although the Kohlman method had the shortest time to union, there was no statistically significant difference between the three techniques, and the worth of the Matti-Russe technique was confirmed. Another study [26] analogously described the shorter union time for vascularized grafts, compared to other techniques, however without a statistical correspondence and sustaining the high union rate for the Matti- Russe procedure. Considering the above mentioned, an additional undeniable advantage of the Matti-Russe with respect to other techniques is that hardware is not necessary (and therefore hardware removal in a second surgical time), as there is no need for fragment compression (for example, by using a screw). As a matter of fact, the aim of the Matti-Russe method is to restore the height of the scaphoid, which is obtained by packing the cavity previously created with a cortico-cancellous graft of bigger dimensions. In our patients, we never compressed the 2 fragments, as a shortening of the longitudinal axis of the scaphoid must be avoided; on the contrary, often distraction of the fragments given by the bone graft (necessary for restoring the height of the scaphoid), determined an incomplete contact at the non-union site. This, however, differently from another study [27], did not impair our results as our patients had a good radiological outcome at follow-up in 93.8% of cases and scored excellent or good in 81.2% of cases with the MWS at 4-months postop. It must be specified that all our patients were carefully selected and all were classified as grade II according to Alnot, therefore with no, or very little, arthritic deformity. Surely the rigorous selection of patients who must undergo the Matti- Russe technique, leads to excellent and good results despite the position of the fragments [27,28].
The variant of the Matti-Russe technique used in our study contemplates a bone graft harvested from the distal volar ipsilateral radius. This implies that only one surgical incision is required, without risks on the donor site (in the original technique: iliac crest) [4,18] and a general anaesthesia can be avoided. Zoubos et al. [28]described a similar approach, although in their study an instability of the fragments after grafting was reported in 17.4% of cases, which required an osteosynthesis with 2 Kirschner wires. We never had an in stability and never required the use of hardware. Our patients were immobilized postoperatively with a short arm thumb spica cast for 6 weeks, differently from the 3 months described in other studies [28], eliminating the long immobilization period of the original technique. As a matter of fact, the clinical evaluation of the wrist range of motion at 4-months postop was improved, although not in a statistically significant way.
One limitation of the technique, as shown by the only complication we had, is the integrity of the vascularization of the proximal pole, which has to be big enough to create a cavity in it. Our patient had a MRI documented avascularity of the proximal pole, which after the Matti-Russe procedure progressed in a necrosis and collapse of the scaphoid and required a second surgery with a four-corner fusion. However, the reported MWS was satisfactory. In conclusion, the Matti-Russe procedure is a valid, low cost procedure, with a high union rate after 4 months postop. Our variant of the technique has a further advantage of being less invasive, requiring only one incision, no need for general anaesthesia and no need for hardware implant and removal. Our post-operative shorter time of immobilization leads to an improved range of motion and excellent and good MWS scores.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Research Ethics Committee (or Institutional Review Board). For this type of study formal consent is not required.
Informed consent was obtained from all individual participants included in the study.


