Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Saberi Masoud1* and Mortazavi Nafiseh2
Received: July 26, 2017; Published: August 22, 2017
Corresponding author: Saberi Masoud, Orthopedic Surgeon, Consultant at Loghman General Hospital, Iran
DOI: 10.26717/BJSTR.2017.01.000291
Although conventional osteosarcoma is one of the most common type of primary bone malignancy but fibroblastic subtype is rare enough to push us to report this case. We had experience with scapulectomy for conventional osteosarcoma with dominant fibroblastic component. The technique of surgery and safe margin in scapula were our debates.
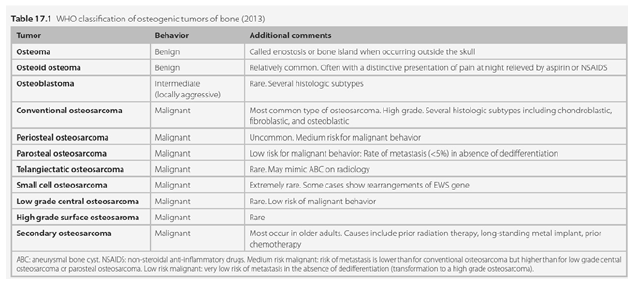
Osteosarcoma is the most common malignant bone tumor (if one excludes myeloma). Figure 1 show WHO classification of osteogenic tumors of bone (2013). Conventional probably is almost common type of osteosarcoma but about one percent of all conventional occur in flat bones and the number of fibroblastic presumably is rare, however, Frequency of fibroblastic subtype osteogenic sarcoma in 13 SEER registries between the years 1994 and 2008 was 111, and mean age in this series was 32 between 10 to 90 years old for this subtype [1]. Acceptable treatment for high grade conventional is wide resection after neoadjuvant chemotherapy and continue chemotherapy [1,2].
Figure 1: WHO Classification of osteogenic tumors of bone.
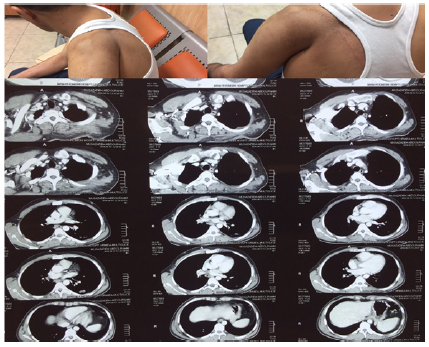
Our Patient is a 34 years old young healthy man without any previous comorbidity, with history of couple of month progressing pain and bump on his scapula. After tumor work up including lab tests, Xray, CT scan, whole body bone scan, open biopsy was done in other center. Report of pathological paper was conventional osteosarcoma of scapula, then refer to us. Diagnose was not difficult because of characteristic of sarcoma. At the time of visit we faced with ill patient had severe pain, unable to sleep. We perform CTscan and MRI for lesion and chest, thorax surgeon and oncologist consulting (Figure 2). In Enneking system for staging benign and malignant musculoskeletal tumor that got high-grade with intra compartmental disease have no metastasis, means II-A.
After patient and family negotiation we do neo adjuvant chemotherapy then after two month surgery was done intra articular total scapulectomy as Malawer et.al type 3 technique with elliptical oblique incision at lateral decobutos position as Duspital described (Figure 3). We followed patient for 18 months at time of this paper and any recurrence haven’t seen yet according to MRI (Figure 4).
Figure 2: Pre-operative.
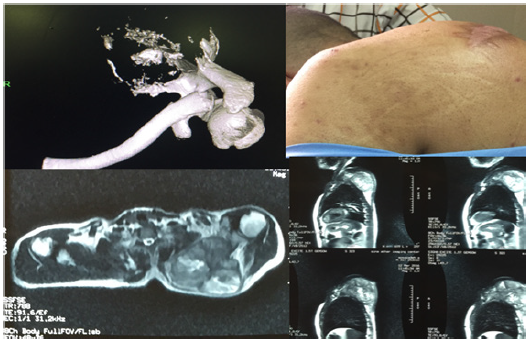
Figure 3: A&B-Fibroblastic osteosarcoma consist predominantly of atypical spindle cells; C-Direct formation of neoplastic osteoid by tumor cells; D-Fibroblastic osteosarcoma are highly vascular sometimes with hemangioprericytomatous appearance.
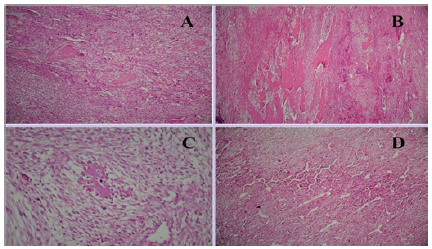
Figure 4: Enneking et al.
According to report of our pathologist: Specimen was 20 cm in greatest dimension and additional dimension 18*10 cm. grade 3 (high grade) conventional osteosarcoma with fibroblastic component. Distance of sarcoma from lateral, medial, inferior, superior and posterior margins are: 0.3cm, 0.7cm, 6cm, 0.6cm and 0.3cm respectively. Anterior margin uninvolved by sarcoma but very close less than 1mm glenoid cavity uninvolved by sarcoma.
High-grade intramedullary osteosarcoma accounts for about 75% of all lesions and is also referred to as conventional osteosarcoma [1]. The microscopic pathology of conventional osteosarcoma has traditionally been subdivided into three categories: osteoblastic (50%), chondroblastic (25%), and fibroblastic (25%) [3]. The radiologic features of osteosarcoma vary over a wide spectrum. In most cases, typical radiographic features clearly suggest the aggressive bone-forming nature of the lesion. Common features of osteosarcoma include tubular bone metaphyseal location, mixed pattern of osteolysis and osteosclerosis, cortical destruction, periostitis, and soft-tissue mass [1,4].
Figure 5: Post operation.

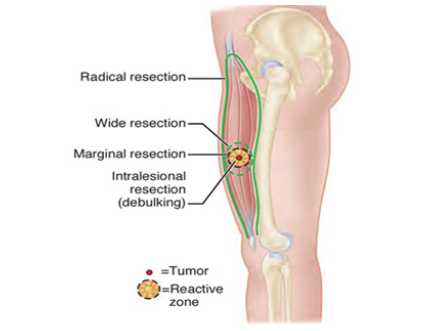
The differential diagnosis of purely lytic osteosarcoma includes other bone malignancies that do not form osteoid, such as malignant fibrous histiocytoma, fibrosarcoma, metastatic disease, and Ewing’s sarcoma [5] Enneking classification of local procedures (From Enneking WF: Musculoskeletal tumor surgery,vol1,New York,1983,Churchill Livingstone) (Figure 5). According to evidences [6,7] to achieve best result for treatment high grade osteosarcoma is wide resection with or without chemo radiotherapy. When we can’t achieved safe margins as wide it called marginal resection and not safe for high grade tumors unless it’s not accessible such scapula.
Figure 6: After six month follow up.
For scapula as a bone without adorable compartment to get safe margins many debates are ,in other hand not a common site for primary bone sarcomas fore enough evidences, so almost always treatment for high grade scapula malignant tumor is marginal resection with adjuvant chemo radiotherapy (Figure 6). For this case we consult with thorax surgeon and decided not disturbing chest wall unless obvious involvement figure out, during surgery we find a fine seudo capsule separate safe, tumor from chest wall [8].
Figure 7: One year after surgery.
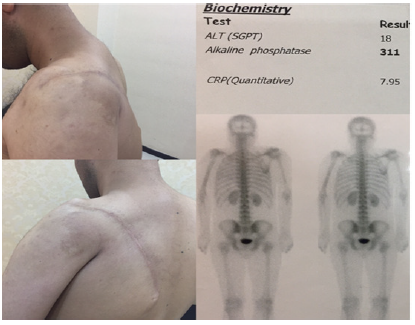
Secondarily respect to not involving gelenoid neck and gelenohumeral joint in preoperative imaging, modification of Tikhoff-Linberg (intra articular total scapulectomy) was done to give chance of some motion in humerus without massive reconstruction (Figure 7). We done search in PubMed for procedure of high grade scapular body sarcoma and not a straight forward procedure found. Conflicting data is for definitive treatment such a lesions so our debates are: what are safe margins for scapular body high grade malignant mass? Which procedure (technique) is preferable?
Goal of this report was help to solve the issue of it is better not violate chest wall other than get safe margin in osteosarcoma of scapula. We believe this is long way stairs and this report can be a step for that.
At the time of definitive surgery consent was performed.
The authors wasn’t receiving any found from any sources for this paper. The cost of hospitalization and procedures paid by ordinary public health insurance.


