Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Jacqueline Sidman*, Max D Lechtman, H Vernon Roohk and Steven J Hershey
Received: July 21, 2017; Published: August 07, 2017
Corresponding author: Jacqueline Sidman, The Sidman Institute, University Tower, 4199 Campus Drive, Suite 550, Irvine, California, 92612, USA
DOI: 10.26717/BJSTR.2017.01.000255
The goal of this pilot study was to evaluate psychometric testing to establish objective assessments for treating depression and co-morbid anxiety. Clients of The Sidman Institute were asked to take the BDI-II and BAI before and after three therapy sessions. Short-Term Sidman Hypnotherapy (STSH), independent of antidepressants, resulted in significant improvement by Wilcoxon analysis of BDI-II (Z=3.264, p=0.0011) and BAI (Z=3.233, p=0.0013) with large effect sizes (>0.9). Rumination-associated symptoms decreased significantly, and retrospective followup with previous clients indicated no relapse from one to three years post therapy, further indicating treatment effectiveness.
Psychometric tests are used to compare subjective and objective responses to anti depression and anti anxiety therapies. The 2004 FDA’s Black Box Warning, concerning potentially serious side effects of antidepressants, has changed attitudes about these medications. Effective therapy generally occurs with psychotherapy and antidepressants, requiring many weeks of therapy, followed by periodic monitoring [1]. Antidepressant use is controversial, medical compliance is often difficult, and extends for long periods of time [2-4]. After initial improvement, those most susceptible to remission of depression ruminate, and this was considered a predictor of relapse [5,6]. Short-Term Sidman Hypnotherapy (STSH), requiring only three to six sessions, is an alternative modality for various psychological and physical conditions.
This one-group, pretest/post-test pilot study with a relatively small sample size utilized clients of the Sidman Institute, during 2009, who expressed a desire for anti depression therapy. The criteria for selection were ages 18 through 75, a baseline BDI-II score of at least 6, and an informed consent agreement. An assessment of visual, auditory and kinesthetic abilities served as the determinant for exclusion, since they are critical to STSH. Clients were not excluded because they used antidepressants. Post-test administration of the BDI-II and BAI followed a variable latency period. Since pretreatment and post-treatment BDI-II and BAI severity appears to be equivalent among men and women [7], both were combined into a single experimental group. Mean (m) pretest and post-test scores and their s.d. were calculated for the various experimental groups and are shown in Table 1. The mean time in days between pretest and post-test scores, as well as the mean times between the first and third therapy sessions and between the third therapy session and post-test, are presented in the text along with their standard deviations. Because of the small sample size, modern nonparametric statistical methods were employed in order to minimize heteroscedasticity. This allowed for the treatment of potential outliers by Wilcoxon Analysis (WA) [8]. WA is robust enough for analyzing the main effect of the dependent variable scores (BDI-II and BAI). Participants taking antidepressants were compared to the non-medicated participants by the Mann-Whitney U test (U).
Effect size was estimated by Probability of Superiority for Dependent Groups (PSdep), a statistic with a value of 0 to 1.00 [9]. For the sake of clinical utility, improvement in effect size was referenced to one full s.d. for BDI-II published data and two-thirds s.d. for BAI published data [10,11]. Simple regression was used as an initial indicator of treatment permanence by regressing the time in days between the final session and post-test onto the post-test scores. Pretest and post-test scores using seven BDI-II test items representing rumination: self-dislike, concentration difficulty, indecisiveness, past failures, guilt feelings, self-criticalness and worthlessness and five BAI test items: unable to relax, fear of the worst happening, fear of losing control, nervousness, and being terrified-were totaled and compared by WA. Finally, rumination subset scores of the BDI-II and BAI inventories were obtained retrospectively by the therapist via telephone interviews of 10 former clients treated for depression at least one year prior to this study. The longevity of STSH was then quantified by comparing scores from these clients, who had each completed a six-session course of treatment, to the post-test pilot cohort scores by U.
Thirty-two clients met the selection criteria and participated in the study. Seventeen did not complete the study due to early satisfaction, economic reasons or indifference. One was excluded. The study population was 14, with 2 M and 12 F. Client ages had a range of 20 – 59 years, m = 43.2, at the time of initial therapy. Table 1 contains the m and s.d. for BDI-II and BAI pretest and post-test scores for the four medicated and 10 non-medicated clients. No significant differences were found between medicated and nonmedicated STSH clients regarding pretest and post-test scores by U analysis for both depression and anxiety. Significant improvements (WA) with large effect sizes (PS) were demonstrated for the 14 clients as a whole for both depression and anxiety. The mean time between the first and third therapy sessions was 34.6 days (s.d. 15.73). The mean time between the pretest and post-test was 61.71 days (s.d. 31.17) and, between the third therapy session and the post-test 25.5 days (s.d. 24.64).
Table 1: The Effectiveness of Short-Term Sidman Hypnotherapy for Depression and Anxiety.
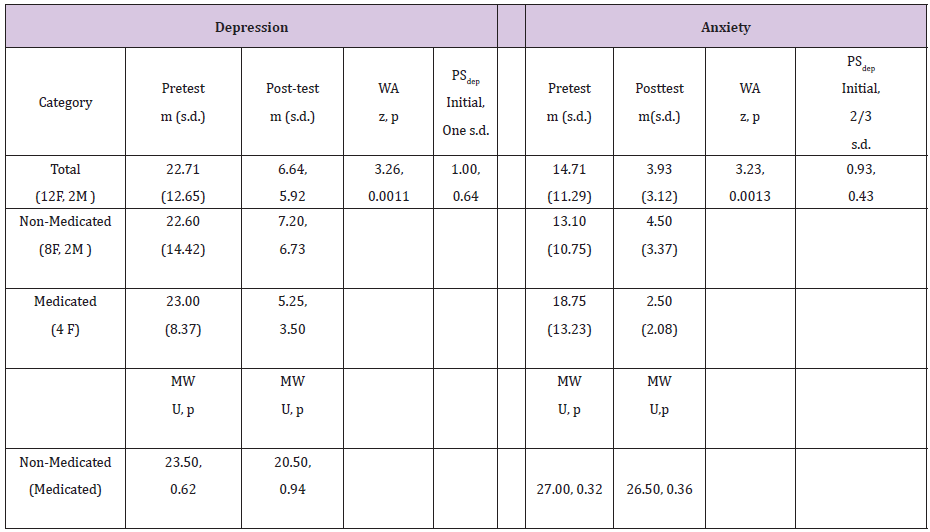
Significant improvements in rumination subset scores for the 14 pilot clients were seen for BDI-II (WA: Z = 3.33, p = 0.0012) and BAI (WA: Z = 3.23, p = 0.0012). Rumination subset scores of 10 former clients (7 F and 3 M) tested retrospectively 1-3 years after completing six sessions of STSH totaled 20 (m = 2.0) for BDI-II and 8 (m = 0.8) for BAI. No significant difference was found between these retrospective scores and the post-test scores of the 14 pilot clients for BDI-II (U = 71.0, p = 0.98) and BAI (U = 86.5, p = 0.340. Treatment permanence was further indicated when no relationship was found by simple regression as a result of regressing the difference in latency between third session and post-test onto the post-test scores for the pilot clients (r=0.070, alpha=0.81, beta=0.20).
Objective measures of treatment effectiveness were sought in the analyses of psychometric data. In a pilot study limited to 14 clients, depression and anxiety symptoms were significantly reduced with a strong effect size within three STSH treatment sessions. In another population, six sessions of STSH produced permanence of therapeutic gains over a 1-3 year period without follow-up and known side effects. A case study reported that the use of STSH for a client with interstitial cystitis resulted in substantial pain reduction after 2-3 sessions and no symptoms after 6 sessions, persisting for 5 years [12]. Pilot and retrospective patients provided favorable testimonials.
Psychotherapy typically produces sustained effects on depression-relapse prevention equivalent or superior to those achieved with antidepressant maintenance treatment [13]. Successful standard hypnotherapy relies on reinforcement by repeated visualization and self-hypnosis [14]. Conventional treatment requires extensive follow-up to mitigate rumination [15]. STSH treatment involves a subtle approach that eliminates negative, outdated defense mechanisms that are the root cause of repetitive patterns. Once these emotional triggers are eliminated,the resultant emotional, physical and behavioral problems invariably disappear. STSH utilizes conscious communication with one’s own subconscious mind, interactively restructuring emotional memories with guidance by the therapist. Unlike traditional hypnotherapy, psychotherapy and antidepressants, STSH has proven effective for considerable periods of time; most often without follow-up therapy and known risk factors alluded to in the FDA’s Black Box Warning. Reliance on psychometric data for assessing treatment effectiveness and predicting treatment permanence warrants further research.
All authors’ duties included design of the study, writing and approval of the manuscript, having full access and responsibility for the integrity and accuracy of the data analysis. Jacqueline Sidman’s primary function was as STSH therapist. She also participated in data collection. Max D. Lechtman’s primary function was as general manager. His duties included data collection and preliminary analyses. H. Vernon Roohk’s primary role was to serve as biostatistician. His duties included assisting with general management. Steven J. Hershey’s primary role was to serve as the clinical psychologist to assist in the interpretation of the data.
This pilot study was sponsored by the The Jacqueline Sidman Health Foundation in conjunction with The Sidman Institute.
We are very grateful to Steven M. Harris, PhD, for assistance with the selections for psychometric testing and to Joseph McKean for performance of the Wilcoxon analyses.


