Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Yi-Shan Chen1* and Wei-Tso Chia2
Received: July 27, 2017; Published: August 07, 2017
Corresponding author: Yi-Shan Chen, Department of Orthopaedics, National Taiwan University Hospital Hsin-Chu Branch, No.25, Lane 442, Sec. 1,Jingguo Rd, Hsinchu City 300, Taiwan
DOI: 10.26717/BJSTR.2017.01.000254
Raynaud’s phenomenon, characterized by recurrent vasospasm in the fingers and toes, is a common clinical disorder encountered by dermatologists. Hand-arm vibration syndrome is well known to cause secondary Raynaud’s phenomenon. The goal of treatment is to improve microcirculation and decrease inflammation, platelet activation, and vasospasm. We have reported a chronic case of Raynaud’s phenomenon in a 46-year-old aboriginal man with gastric carcinoma who simultaneously underwent gastrectomy and chemotherapy. The patient had developed gangrene at the tip of the right index finger and toes previously, and his fingers and toes had been amputated. The patient was hesitant to have another finger amputated. Hence, he was administered a combination therapy of pentoxifylline, extended-release nifedipine, and low molecular weight dextran for treating the acute symptoms of Raynaud’s phenomenon. At the later stages of his disease, only extendedrelease nifedipine was administered. Treatment with nifedipine resulted in an improvement in the symptoms.
Abbreviations: HAVS: Hand-arm vibration syndrome; LMWD: Low Molecular Weight Dextran; TNF: Tumor Necrosis Factor
Raynaud’s phenomenon is a common clinical disorder encountered by dermatologists. This condition usually occurs in response to exposure to cold temperature or emotional stress, and it is characterized by recurrent vasospasm in the fingers and toes. Hand-arm vibration syndrome (HAVS) is a well-recognized cause of secondary Raynaud’s phenomenon. The pathogenesis of HAVS involves a complex interplay of vascular, neural, and intravascular effects, and its pathologic characteristics include fibrosis and vasoconstriction [1]. The goal of treatment is to improve microcirculation and decrease inflammation, platelet activation, and vasospasm. Infusion of low molecular weight dextran (LMWD) has been successful in treating systemic sclerosis with Raynaud’s phenomenon without any adverse effects [2]. Buell [3] reported the successful resolution of fingertip ulceration with pentoxifylline and nifedipine in a case of secondary Raynaud’s phenomenon caused by HAVS. Here, we have reported a case of chronic Raynaud’s phenomenon in a patient who simultaneously underwent gastrectomy for gastric carcinoma and chemotherapy.
Figure 1A: Tip of the right ring finger with ischemia. Radial side of the tip of the right ring finger shows necrosis.
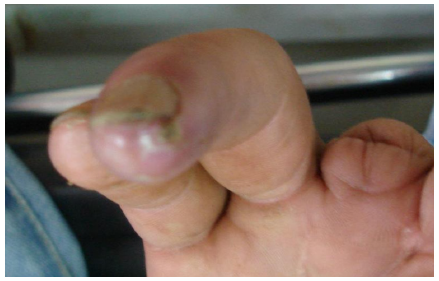
Figure 1B: Tip of the right ring finger with ischemia. Volar side of the tip of the right ring finger shows necrosis.

A 46-year-old aboriginal man with gastric carcinoma and a 5-year history of Raynaud’s phenomenon presented at our emergency department with pain in the tip of his right ring finger that had started a week prior. His occupation exposed him to handarm vibration. His right index and middle fingers were amputated 4 years ago, and the big toe and fourth toe of the right leg were amputated 2 years ago. He did not have any other systemic diseases or traumas; however, he had a smoking history of 0.5 pack-years. The patient was scheduled to undergo surgery for the gastric carcinoma. The ischemic area identified by pale skin was approximately 2 × 1 cm, and the area of necrosis was 0.6 × 0.3 cm over the right index finger tip (Figures 1A & 1B). He was prescribed pentoxifylline (400 mg twice daily), extended-release nifedipine (30 mg/d), and LMWD (500 mL/12 h) for treating Raynaud’s phenomenon. In addition, he was advised to stop smoking.
His symptoms markedly improved after the first LMWD injection was administered. After the third day of treatment, he underwent total gastrectomy in our general surgical department. Owing to this surgery, the medications for Raynaud’s phenomenon were temporarily withdrawn for 3 days. Unfortunately, the necrotic area enlarged in these 3 days and hence, his medications were resumed. After 1 week of treatment, the symptoms improved, but the necrosis remained unchanged. After 16 days of treatment, the symptoms continued to improve, but necrosis was still present.
Figure 2: Tip of the right ring finger after treatment.

he patient was subsequently discharged, and he was followed up 1 week later at the OPD in the oncology department. He was then admitted to the oncology department to receive chemotherapy for the treatment of his gastric cancer. Pentoxifylline was withdrawn, as it could cause bleeding of the gastric ulcers surrounding the previous operative wound. Additionally, LMWD was withdrawn because the patient did not exhibit acute symptoms. The necrotic region healed, and the symptoms were relieved after another 2 weeks of treatment with nifedipine (Figure 2). We have reported a case of chronic Raynaud’s phenomenon in a patient who simultaneously underwent gastrectomy and chemotherapy. The patient had previously developed gangrene at the tip of the right index finger and toes, and his fingers had been amputated. He responded to combination therapy with pentoxifylline, extendedrelease nifedipine, and LMWD for acute symptoms; during the later stages of the disease, he was treated with extended-release nifedipine alone.
In this case, a combination of 3 medications (pentoxifylline, extended-release nifedipine, and LMWD) ameliorated the symptoms of Raynaud’s phenomenon. Pentoxifylline decreases leukocyte deformability and chemotaxis by decreasing the responsiveness of interleukin-1 and tumor necrosis factor (TNF), decreases TNF-α production in monocytes and macrophages, decreases platelet aggregation and adhesion, decreases fibroblast response to TNF-α, and improves red blood cell deformability [4]. In our case, treatment with pentoxifylline was stopped due to gastric ulceration during the later stages of Raynaud’s phenomenon. Nifedipine, a calciumchannel blocker, increases vasodilation and decreases vasospasm [5]. The patient underwent chemotherapy and continued treatment with nifedipine for Raynaud’s phenomenon. In addition to an improvement in the symptoms, the necrotic region healed after treatment with nifedipine.
Here, we have reported a case of Raynaud’s phenomenon in a patient who was admitted to our emergency department with pain in his fingertips. Because of his previous experience with the amputation of his fingers and toes, he was afraid of having another finger amputated. Further, a gastrectomy was necessary for gastric carcinoma. Hence, he was depressed and frustrated. To our knowledge, there has been no definite treatment for Raynaud’s phenomenon thus far. We have suggested an alternative treatment option for such patients; it is important that medical care providers are aware of all possible treatments.


