Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Alexander Valdés Martín*1, Lila Alicia Sifontes Echevarría2, Alexer Torres Figueroa3 and Giorgis Carlos Reyes Navia2
Received: July 20, 2017; Published: July 24, 2017
Corresponding author: Alexander Valdés Martín, Assistant researcher and Professor, Fellow of the American College of Cardiology (FACC), Cuba
DOI: 10.26717/BJSTR.2017.01.000221
Mitral Insufficiency (MI) is currently the second most common cause of valvular disease accounting for one-third of valvulopathies. The early detection of deteriorating systolic function in patients with chronic mitral regurgitation, and thus the ability to identify the most appropriate moment for surgery remains a challenge to physicians. The analysis of myocardial deformation has recently emerged as a quantitative means of reliably estimating myocardial contractility. In the assessment of left ventricular function it is therefore less dependent on the load than traditional methods. There are currently two ways to assess myocardial deformation: tissue Doppler (TD) and a new method known as speckletracking (ST). The aim of the present revision was to deepen the study of the longitudinal myocardial deformation of the left ventricle using these techniques for predicting the LVEF deterioration in patients who have undergone surgery for chronic severe mitral valve regurgitation
Mitral Insufficiency (MI) is currently the second most common cause of valvular disease accounting for one-third of valvulopathies. It situation represent an important public health problem. Severe grade chronic MI represents a disease of slow progression. Within the first 10 years of its diagnosis about 90 % of patients will present symptoms like heart failure or they will probably die. The only treatment capable of increasing survival in these patients is surgical intervention [1].
The long-term development of left ventricular dysfunction is a major concern in the management of patients with chronic severe mitral valve regurgitation [2-5]. In the preoperative period alterations in myocardial contractility may be ‘invisible’ with the traditional methods used to assess systolic function, a consequence of the loading conditions present. Mitral regurgitation provides a low impedance alternative for left ventricular ejection, and increases the left ventricular ejection fraction (LVEF) [6]. The early detection of deteriorating systolic function in patients with chronic mitral regurgitation, and thus the ability to identify the most appropriate moment for surgery remains a challenge to physicians.
The analysis of myocardial deformation has recently emerged as a quantitative means of reliably estimating myocardial contractility. The strain represents the percentage shortening of the myocardial fibers while the strain rate which represents the speed of myocardial deformation, is derived as a function of strain and time. The main advantage of this method over those that analyze myocardial displacement is that it differentiates between active contraction and the passive movement resulting from the general translation of the heart or through the traction of neighboring myocardial regions. In the assessment of left ventricular function it is therefore less dependent on the load than traditional methods.
There are currently two ways to assess myocardial deformation: tissue Doppler (TD) and a new method known as speckle-tracking (ST). The latter is not based on Doppler analysis but on the following of bright points via gray scale analysis (Figure 1). The aim of the present revision was to deepen the study of the longitudinal myocardial deformation of the left ventricle using speckle-tracking and TD for predicting the LVEF deterioration in patients who have undergone surgery for chronic severe mitral valve regurgitation.
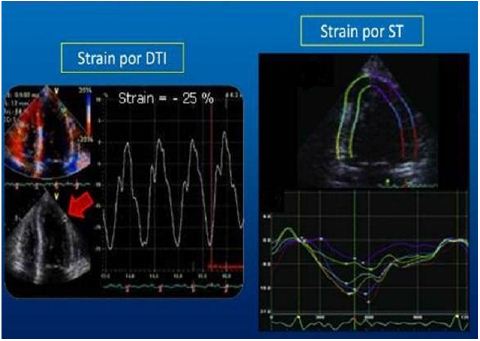
Figure 1: Strain Modalities.
The introduction of the DT has allowed obtaining information about the velocity and displacement of the myocardium throughout the cardiac cycle and has become an important aid in the diastolic function study and in the synchrony evaluation [7]. The estimation of contractility in patients with chronic MI by measuring the systolic velocity of the mitral annulus has allowed the prediction of postoperative ventricular dysfunction in this patients group. The DT has some limitations such as the dependence of the ultrasound angle incidence on the region under study, the respiratory changes, the traction effect exerted by the neighboring normal segments on the adjacent abnormal ones, and the influence of the heart general mobility (translation, torsion and rotation). The DT studies myocardial velocities that approach or move away from the transducer fundamentally longitudinal, that by derivation or integration of these give us information that allows to estimate the segmental displacement (Tissue Tracking) in millimeters, the tissue synchrony in milliseconds (TSI), the Strain or segmental deformation, in percentage, and the strain rate (in cm/s) [8].
Magne et al. [9] assumed that the evaluation of echoestress in patients with chronic and asymptomatic MI also presented promising results. A decreased preoperative contractile reserve (defined as an increase in LVEF < 4 %) proved to be a powerful predictor of postoperative ventricular dysfunction. The main disadvantage of this method is that the contractile reserve analysis was performed by assessing the LVEF whose limitations in MI have already been commented. On the other hand, post-exercise evaluation may be technically difficult in some patients such as those with a poor acoustic window [10].
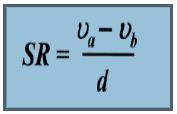
The velocities of the walls obtained in the study with conventional DT do not differentiate between active or passive contraction [11]. That’s why it was necessary to create and improve new muscle Doppler techniques that allow a segmental analysis of the contractile function of the heart, based on high resolution images and offering greater sensitivity and specificity [12]. This technique included the measure of two parameters that reflect the deformation properties of the myocardial fiber: the strain or regional deformation (Є) and the deformation velocity (SR) strain rate. In the past, both parameters were investigated live in laboratory animals using various measurement techniques, but for the past few years they have been available as noninvasive techniques for measuring heart disease.
According to Bierin-Sorense et al. [13], Mirsky and Parmley where the first introduced the concept of deformation and strain velocity as a measure of the myocardium mechanical properties. In the last decade of the last century, this technique was implemented in real time to evaluate Ventricular performance by echocardiography. Myocardial deformation is defined as the transformation that the myocardium undergoes during a cardiac cycle when a force or stress is applied on it. It can be in the sense of shortening (negative) or elongation (positive) in relation to the original length, being a function of distance. Then, for a one-dimensional object, it is calculated with the formula Є = L-L0 / L0, where L is the length after the deformation and Lo is the original length [14].
Myocardial deformation can also be defined as a dimensional less Index of myocardial length change throughout the cardiac cycle. On one hand, the myocardial deformation is a relative measurement does not carry a unit and its value is expressed as a fraction or percentage change [14]. On the other hand, the rate of deformation is the shortening or stretching of the myocardial fiber per unit of time and uses as unit of measure 1 / S or S-1. [15] It can be calculated as follows:
Many studies have demonstrated its clinical applicability from the initial evaluation of these parameters through M mode to the present. It is undoubtedly in this field of echocardiography that the technological progress has been more evident, both in the acquisition method and in the analysis. Several publications have referred to its utility in the assessment of right and left ventricular function, particularly in the identification of subclinical affection in entities such as cardiomyopathies, valvular conditions, atrial function, stress techniques and viability assessment [16].
From the different levels of gray within the two-dimensional image, in the myocardium can be observed small overlapping granules generated by the interaction of ultrasound with myocardial structure. These granules were given the name of speckles.
When we analyze the movement of these granules in relation to the cardiac structure, it observes that these can move (tracking). The speckle tracking technique appears by the unit of these two concepts [14]. This is a method designed for the analysis of S and myocardial SR not based on tissue Doppler but in the analysis of the movement of bright gray dots throughout the cardiac cycle [14]. The results of this analysis can be expressed in different graphs: the two-dimensional mode with its deformation color scale, the anatomic M mode along the myocardium, and the graphical curves versus time. To obtain the longitudinal S must be acquired Images from the apical views of 4, 3 and 2 cameras. Like the S analyzed by DTI, an electrocardiographic record and a Doppler record of opening and closing of the aortic valve should be acquired. Subsequently, the regional longitudinal S is obtained corresponding to each of the segments in the “bullock’s-eye” format, and in turn the S longitudinal global systolic peak defined as the average of the 16 segments analyzed [17].
In ventricular contraction, the myocardium is shortened longitudinally and circumferentially (S negative), and thickened radially and transversely (S positive). The longitudinal global S in a normal subject varies between -16 and -22 % while the circumferential is slightly larger and varies between -21 and -27 %. In contrast, the normal value of the radial global S is significantly higher and Varies between 35 % and 59 % [18].
In turn, it is possible to evaluate the “squeezed” function of the left ventricle by calculating the difference between the rotation of the base (clockwise) and the rotation of the apex (counterclockwise). This function is defined as torsion (systolic) and distortion (diastolic) [18]. The analysis of myocardial deformation using speckle tracking has been used successfully in the evaluation of the contractile function of other pathologies such as hypertrophic cardiomyopathy and aortic stenosis, as well as in the evaluation of patient’s candidates for myocardial resynchronization therapy. This method would solve some of the limitations of S and SR obtained by DTI. The main advantages over this method are:
A. It is independent of the angulations of the ultrasound beam, thus allowing the analysis of segments that are not aligned parallel to the ultrasound beam. At the same time, it allows measurements of S and SR radial in both the parasternal short axis and the apical plane of 4 cameras. On the other hand, it is possible to evaluate the movement of torsion and rotation of the left ventricle which allows a better study of the contractility of the left ventricle.
B. Allows performing a direct measurement of the myocardial deformation while the tissue Doppler makes estimation through the integral of the velocity gradient in the space.
C. It is not affected by myocardial translational movement.
D. It presents less inter- and intraobserver variability
The major drawback of this method is the susceptibility to be affected by artifacts when the image is not of sufficient quality. This makes it difficult to analyze poorly visualized segments and patients with poor acoustic window [19].
The evaluation of systolic function through the analysis of myocardial deformation is a useful method in the prediction of postoperative ventricular dysfunction in patients with mitral valvular replacement.


