Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Muringani BN and *Mutsvanga T
Received: June 19, 2017; Published: July 03, 2017
Corresponding author: Mutsvanga T, Department of Medical Microbiology, Faculty of Health Sciences, National University of science and technology, Zimbabwe
DOI: 10.26717/BJSTR.2017.01.000165
Background: This study conducted in a mining town in Matebeleland South Zimbabwe evaluated the prevalence of H. pylori infection and the presence of gastritis in HIV-infected patients coming from a low socioeconomic background.
Methods: Blood samples were collected from 110 patients, who came to healthy centres complaining of gastritis. H. pylori status and HIV status were serologically screened on these samples.
Results: The prevalence of H. pylori infection was significantly lowers (p < 0.001) in HIV-infected (37.2% males and 30% females) than in uninfected (75.8% males and 70% females) for patients. There were no significant differences between H. pylori status and gender. Ante retroviral treatment, Viral Load and CD4 assessments were not done on this group of patients.
Conclusion: We demonstrated that the prevalence ofH. pylori was significantly lower in HIV-positive patients compared with HIV-negative ones. However, gastritis was frequently observed in the HIV-positive patients as it was their major reason for coming to the clinics.
Abbreviations: CMV: Cyto Megalo Virus; GI: Gastro Intestinal; HIV: Human Immunodeficiency Virus; AIDS: Acquired Immuno Deficiency Syndrome
It is well known that the immune deficiencies caused by HIV give rise to many different gastrointestinal opportunistic infections, such as cytomegalovirus (CMV) infection and fungal esophagitis [1]. Helicobacter pylorus (H. pylori) is a gram negative, spiral, flagellate bacillus that naturally colonizes humans, living in their gastric mucus. And is the major etiologic factor of chronic gastritis and peptic ulcer in the general population. Gastrointestinal (GI) symptoms are frequent among patients infected with human immunodeficiency virus (HIV) and with acquired immunodeficiency syndrome (AIDS) [2] however, the role of H. pylori infection in the GI tract mucosa of HIV patients is not well defined [3]. Some studies suggested that interactions between the immune/inflammatory response, gastric physiology and host repair mechanisms play an important role in dictating the disease outcome in response to H. pylori infection, suggesting that the host’s immune competence might be an important issue in H. pylori infection [3].
Data in regard to the prevalence of H. pylori infection in HIV infected population are controversial. H. pylori related gastritis has been noted to occur less frequently (that is, in 5 to 59% of cases) in adult patients with the acquired immunodeficiency syndrome (AIDS) [4]. Some reports have shown that the rate of the infection in HIV-positive patients is remarkably low when compared with the general population [4,5]. Conversely, other studies have not found similar results.
To assess if there is any correlation between positive cases of H. pylori reporting to healthy centres in a mining town complaining of gastritis and their HIV status.
Blood samples were collected from 110 patients, who came to healthy centres complaining of gastritis. H. pylori status and HIV status were serologically screened on these samples. Plain tube blood collection tubes were collected from patients male or female complaining of gastrointestinal infections including those with peptic ulcers and gatsritis. Serum was taken from these samples and serologically screened for H. pylori and HIV.
(Tables 1 & 2)
Table 1: H.pylori status vs gender.
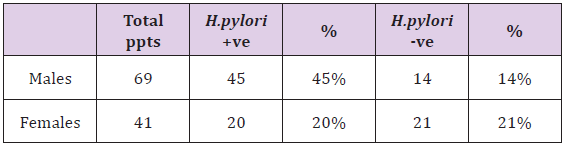
Table 2: H.pylori vs HIV Status.

The prevalence of H. pylori infection was significantly lower (p < 0.001) in HIV-infected (37.2% males and 30% females) than in uninfected (75.8% males and 70% females) for patients. There were no significant differences between H. pylori status and gender. Antiretroviral treatment, Viral Load and CD4 assessments were not done on this group of patients. The results are reflected in (Tables 1 & 2). These results are in agreement with results of studies of Olmos et al. (2004), however, they found that HIV-infected patients with H. pylori have a higher mean CD4 count than HIV-infected patients without H. pylori, but, in our study we didn’t assess any differences in CD4 count between these two groups. Probably, frequent use of antibiotic in HIV-infected patients has a role in eradicating or controlling H. pylori infection but cannot completely eradicate H. pylori from gastric of these patients. In conclusion, our results showed, by screening H. pylori in blood of HIV-infected patients that, prevalence of this bacterium in these patients is lower than in those HIV negative. In fact, this prevalence is similar to prevalence of H. pylori in population, but why this bacterium cannot show gastric symptoms in these patients is not clear and more studies are needed to clarify it.


