Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
*Daniela Vazquez Capdepon
Received: June 06, 2017 Published: June 09, 2017
Corresponding author: Daniela Vazquez Capdepón, Medical Director of the Centro Oncológico campana, Oncologist of the Perú Hospital Gral. Galarza, Oncologist of the Centro Medico San José, French 374 – Campana, Pacia. BS. AS
DOI: 10.26717/BJSTR.2017.01.000124
Lung cancer is the most common cause of cancer death in Western countries, and non-small cell lung cancer (NSCLC) accounts for 80% of these neoplasms. Despite the efforts in the early diagnosis and advances in the treatment of these patients, overall survival remains very low, approximately 18% at 5 years2. The relatively low (30-50%) survival of patients with limited, potentially curable disease probably reflects the inability to detect advanced disease at initial staging. The stage of the disease is considered the most important prognostic factor and determines the therapeutic options. It is therefore crucial to perform a correct initial staging for the administration of an appropriate treatment, avoiding unnecessary surgeries. In this sense, the identification of contralateral mediastinal lymphatic involvement and distant metastasis is particularly relevant, since it classifies patients as stages IIIB and IV, excluding them from a curative treatment.
Computed tomography (CT), the most widely used technique for evaluating patients with lung carcinoma, is based on morphological criteria and has limited accuracy for the diagnosis of tumor infiltration in normal-sized nodes, as well as detection of post treatment disease. Positron emission tomography (PET), on the other hand, provides valuable functional information in detecting metabolically active tumor cells before morphological changes occur and allows disease to be detected in clinically unsuspected locations.
Currently, PET has become an important tool in the evaluation of lung cancer due to its high sensitivity in the detection of distant and lymph node metastases and has been incorporated into the protocols for preoperative staging of NMSC. The integration of CT and PET in the hybrid PET / CT system allows the acquisition in a single session of the anatomical and metabolic images, combining the benefits of both, while minimizing the limitations of each modality. In addition to the technical advantages involved9, it provides greater sensitivity and specificity than each of its components separately.
For the evaluation of the solitary pulmonary nodule, PET and PET / CT are useful in the characterization of the solitary pulmonary nodule (NPS), since most malignant nodules show an increased glucose metabolism and, therefore, an increase in uptake of 18F-FDG. The metabolism of 18F-FDG in PET and PET / CT clinical studies can be assessed semi-quantitatively using the SUV index.
This index is a semi-quantitative value that expresses the uptake of 18F-FDG in the tissue or injury relative to the injected dose, and is defined as the ratio between the tissue radiotracer concentration and the injected dose divided by the body weight in grams. This value is affected by several factors, such as blood glucose, patient weight, time since radiotracer injection, and size and heterogeneity of the lesion or selected area of interest. Although, in general, an SUV threshold> 2.5 is considered to indicate malignancy, it is recommended that a visual estimate be considered in the assessment of lung nodules and that lesions with increased 18F-FDG uptake with respect to activity of the organ or of the vessels of the mediastinum. In addition, the detection of PET uptake depends on the size of the nodule and its avidity by 18F-FDG, and is difficult in lesions smaller than the spatial resolution of the equipment (6-10 mm) and in tumors well differentiated or hypo cellular. There are also false positive results (PF) caused by inflammatory-infectious processes.
PET / CT have a sensitivity of 97%, a specificity of 85% and a diagnostic accuracy of 93% for the characterization of nodules> 7 mm. In a recent study, PET / CT showed a significantly higher specificity than CT and PET alone (77 versus 66 and 71%, respectively), maintaining the same sensitivity as PET (88%), by combining the analysis of the morphological and metabolic findings of solid and partially solid NPS. It should be noted, however, that this study excluded NPS with attenuation in dull glass.
For tumor staging, the various studies agree on the greater accuracy of PET / CT compared to PET and / or CT in NSCLC staging. The combined technique improves the identification and localization of hyper capturing foci, the detection of infiltration in small lymph nodes, the identification of lesions with low avidity by 18F-FDG, and allows the morphological assessment of lesions.
In a prospective study PET / CT was superior to CT, PET and visual correlation of both techniques in NSCLC staging, providing additional information in 41% of cases, mostly anatomical, as an exact location of lymphadenopathy, Infiltration of the thoracic wall or the mediastinum and localization of distant metastases (Figures 1 & 2). The combined use of PET / CT allows a better differentiation of the hyper metabolic tumor of the distal atelectasis lung parenchyma and adjacent areas of pneumonitis. Thanks to hyper metabolism of the neoplastic tissue, the tumor mass appears with an intense focal uptake, distinguishable from the collapsed parenchyma or with pneumonitis that presents a diffuse mildmoderate uptake. Although there is some overlap in the degree of uptake, as measured by the SUV, it has been reported that PET / CT fusion improves the interpretation of these findings.
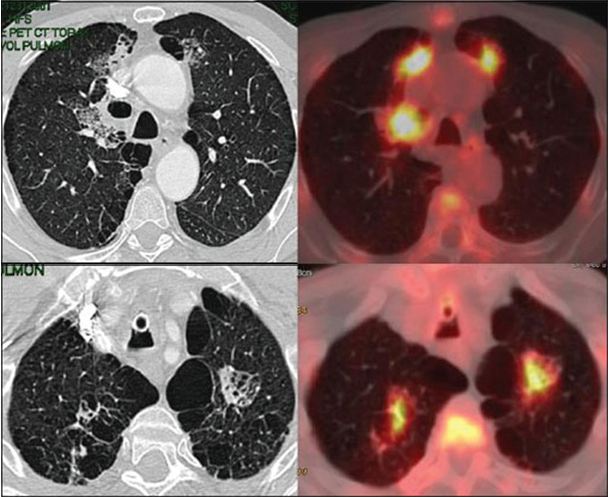
Figure 1: Hyper caption of contrast in lung tumor.
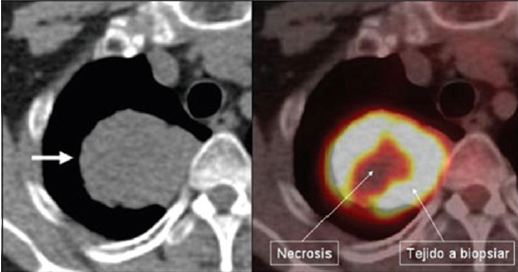
Figure 2: Hyper caption of contrast in adenopathy.
In the evaluation of nodal involvement (N), the morphological size criterion for the characterization of lymphadenopathy has important limitations, so that 21% of the <1 cm lymph nodes have neoplastic infiltration in the pathological analysis, while the 40 % of the> 1 cm show benign changes29. PET, which is less dependent on size, has been shown to be superior to CT in node lymph node evaluation, with sensitivity (79-85%) and specificity (89-92%) significantly higher than CT (sensitivity 57-61% , Specificity 77- 82%). The sensitivity and specificity of PET, and also of PET / CT, vary, however, with lymph node size, so it is more sensitive (100%) but less specific (78%) when the nodes are enlarged , And less sensitive (82%) and more specific (93%) with normal-sized nodes 32,34. Probably the most important value is its high NPV, higher than 90% 35,36, while PPV remains relatively low (70%), due to PF caused by inflammatory pathologies.
Thus, the combination of PET / CT avoids some of the sources of error in the interpretation of PET studies, by differentiating lesions from mediastinal vascular activity, distinguishing the uptake of hilar adenopathy from mediastinal lymphadenopathy close to the hilios, differentiating between a Central tumor and hilar involvement or distinguishes thyroid uptakes from lymphadenopathy in low cervical chains. With regard to CT, the most important benefit is the increased sensitivity of the combined technique which, in a recent study, correctly classified 81% of false negative interpretations (by uptake in normal-sized lymph nodes) and 72% Of PF (non-uptake pathologically sized nodes) on CT.


