ABSTRACT
Bony ankylosis of the temporomandibular joint (TMJ) in a male patient was not diagnosed until the patient reached his late teens. This case report demonstrates the surgical intervention for unilateral Tmj ankylosis using kaban’s protocol. We describe a 17 years old patient with unilateral Tmj ankylosis following a trauma to his chin in his childhood. Interposition gap arthroplasty was done followed by aggressive physiotherapy. A good functional and esthetic result was achieved without further surgery. The results conclude that the following suggested best practice protocol is effective in treating unilateral tmj ankylosis.
Introduction
Ankylosis is a Greek terminology meaning «stiff joint.» It can be defined as «inability to open mouth due to either a fibrous or bony union between the head of the condyle and glenoid fossa Ankylosis is a Greek terminology meaning “stiff joint”. It can be defined as “inability to open the mouth due to either a fibrous or bony union between the head of the condyle and the glenoid fossa [1]. TMJ ankylosis is a disorder that results in restricted mouth opening and inability to perform normal jaw functions or may sometimes lead to immobility of jaws. It may occur as a result of trauma (13- 100%), local or systemic infections (0-53%) or systemic diseases like psoriasis, ankylosing spondylitis, rheumatoid arthritis [2]. In ankylosis, the normal architecture of the joint is altered. It is a severe disability that results in restricted mouth opening, difficulty in mastication, speech, yawning, and nutrition. There may be associated restricted airway problems (obstructive sleep apnea– hypopnea syndrome). When this disease occurs in a growing child, it mostly affects the mandibular development, leading to complex and extensive dentofacial deformities with associated malocclusion [3,4]. Temporomandibular ankylosis is one of the most common pathologies encountered in children but it mostly remains undiagnosed and unmanaged resulting in social and psychological impacts on their lives.
Discussion
Ankylosis of temporomandibular joint (TMJ) is an intracapsular union of the disc-condyle complex to temporal artic-ular surface that restricts mandibular movement, including the fibrous adhesions or bony fusion between condyle, disc, glenoid fossa, and articular eminence [1]. Tmj ankylosis is “the pathological fusion between glenoid fossa of temporal bone and the condylar process of the mandible “. Ankylosis of the temporomandibular joint is an intracapsular union of disc-condyle complex to the temporal articular surface that restricts the functional capacity of the mandible which can be either fibrous adhesions or bony fusion between the condyle, disc , glenoid fossa and articular eminence. [5] This condition may lead to chronic, persistent, and progressive inability to open the jaw, facial deformity, and obstructive sleep apnea–hypopnea syndrome. [6] It affects the quality of life by interfering with mastication, speech, maintenance of oral hygiene and poor esthetics It affects the quality of life by interfering with mastication, speech, maintenance of oral hygiene and poor esthetics. TMJ ankylosis often occurs in young age and hampers the growth resulting in facial deformity and poor airway space. The etiological factors include trauma (most commonly), infection (otitis media, parotitis etc), previous TMJ surgery, and systemic illnesses like psoriasis, rheumatoid arthritis, etc [7]. Other etiological factors are: myositis ossificans, osteochondroma, ankylosing spondylitis (Bechterew Disease) psoriatic arthritis [8], systemic lupus erythematosus, radiotherapy or surgical treatment of TMJ [9].TMJ ankylosis has also been described as a complication after orthognathic surgery [10]. Ankylosis of the TMJ may be classified using a combination of the site (intraarticular or extraarticular), type of tissue involved (bony, fibrous, or fibro-osseous), and extent of fusion (complete or incomplete) [11]. Tripathy et al. have classified ankylosis as true or false. In true ankylosis there is bony or fibrous adhesion between the surfaces of the joint within the capsule, whereas in false ankylosis the problems lie in the surrounding structures [12].
El-Hakim and Metwalli Classification of TMJ Ankylosis
• Class I: Unilateral and bilateral fibrous ankylosis, where condyle and glenoid fossa retain their original shape, and maxillary artery lies in normal anatomical relation to the ankylosed mass
• Class II: Unilateral or bilateral bony fusion between the condyle and the temporal bone, but the maxillary artery lies in normal anatomical relation to the ankylosed mass
• Class III: Distance between maxillary artery and the medial pole of the mandibular condyle is less on the ankylosed than on normal side or the maxillary artery runs within the ankylotic bony mass (seen on coronal CT scan)
• Class IV: The ankylosed mass appears fused to the base of the skull with extensive bone formation, especially in the medial aspect of the condyle such that the ankylosed bony mass lies in close relationship to the vital structures at the base of the skull, such as pterygoid plates, carotid and jugular foramina, and foramen spinosum, and no joint anatomy can be defined from the radiograph (visualized on axial CT scan ) [13].
Radiographic assessment plays an important role in the diagnosis of Tmj ankylosis. CT scan remains to be the gold standard . Axial and coronal sections and three-dimensional reconstruction show the medial extent of ankylosis, which is not visible on conventional radiograph. Axial and coronal sections and three-dimensional reconstruction show the medial extent of ankylosis, which is not visible on the conventional radiographs. CT angiography can be a useful adjunct in the treatment of patients with TMJ ankylosis with a large mass or recurrence or a history of multiple previous TMJ surgeries to determine the relationship of the medial vasculature to the mass [14].
Management
Treatment of TMJ ankylosis is very challenging and rewarding. The aims of the treatment are to establish movement of the joint with adequate mouth opening, maintain a functional occlusion, reconstruct the joint using biological material, correct facial deformity, and to prevent recurrence. Treatment options are listed as follows: Gap arthroplasty with coronoidectomy [15], Lateral gap arthroplasty [16] Interpositional arthroplasty with Temporalis muscle and fascia (Kaban, et al. [17]), Dermal fat (Dimitroulis, et al. [18]), Buccal fat (Rattan, et al. [19]), Auricular cartilage (Lei, et al. [20]), Fascia lata (Narang, et al. [21]), Lyophilized cartilage (Raveh, et al. [22]), Dura (Schobel, et al. [23]), Full thickness skin (Chossegros, et al. [24]). In 2019 Rawaa Y. Al-Raweea, Ali Mohammad Saeed Al-Khayat b, Saud salim Saeed published a case report with similar treatment plan [25].
Case Report
A 17 year-old boy reported with the complaint of inability to the open mouth since 7 years. He gave a history of a trauma to his chin from height fall at age 10 years, and there was a Para symphyseal fracture for which he got operated on then. He eventually recognized the inability to open the mouth within 1-2 years after trauma. No medical or surgical intervention was done in the past. Extra oral examination revealed facial asymmetry with fullness of cheek on the right, ramus height and mandibular body was small, with increased gonial angle. His feeding was characterized by an inability to masticate food, limiting intake to liquids or semisolids. He had a convex profile , severely retrognathic mandible , absence of chin button and bimaxillary protrusion . Figure 1 Intra oral examination revealed null mouth opening. Upper and lower teeth were misaligned and proclaimed due to lack of apical basal bone Figure 2. Radiographic examinations comprised of the orthopantomogram Figure 3 and computerized tomography Figure 4 that revealed a lack of structural organization and the obliteration of right TMJ space. Based on these findings, a diagnosis of unilateral left bony TMJ ankylosis was confirmed. He was also suffering from social and psychological disturbances with low self-confidence.
Treatment
A sequential protocol for the treatment of TMJ ankylosis is based on aggressive resection of ankylotic mass. While respecting, a special approach has to be directed particularly to the medial aspect of the joint which is in close proximity to the internal maxillary artery to ensure that the bony, fibrous, and granulation tissues are completely removed. After complete evaluation, a surgical treatment with interpositional gap arthroplasty on the left TMJ using Kaban’s protocol was planned under general anesthesia. The surgical approach consisted of alkayat and bramley preauricular incision. Figure 5 Full thickness mucoperiosteal flap was reflected Figure 6 and the ankylotic mass was exposed. Figure 7 The section consisted of two horizontal osteotomy cuts which were placed at the level of the joint (below the zygomatic arch) and removal of a bony wedge was done so that a gap were created between the roof of the glenoid fossa and the ramus. It is not possible to remove the entire block in toto; hence, the bone was removed carefully by using surgical burs until the bone is thinned which was then removed using a chisel or osteotome. Next step was to perform cricoidectomy on the same side The joint cavity was then irrigated with normal saline, and the bony margins were smoothed using bone file.
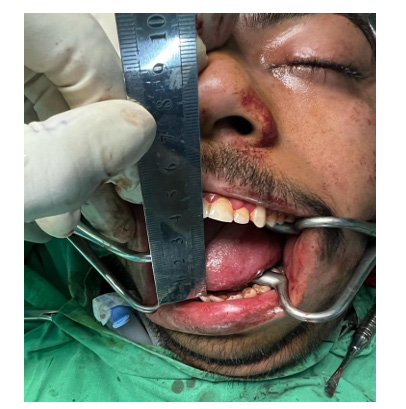
Aggressive early mobilization of the jaw by creating a Forceful mouth opening of about 45 mm using the mouth gags at the time of surgery. Figure 8 Temporalis fascia flap harvested from the same surgical site and rotated over the zygomatic arch to cover the whole of the glenoid fossa and sutured anteriorly, laterally, and posteriorly. Figure 9 Suction drain was placed, and the flap was sutured using 3-0 vicryl for deeper layers and the skin was closed using staple sutures. The width of the bone removal is considered crucial. It is recommended to create a gap of at least 1 cm to prevent ankylosis. It is also important to create a gap of equal dimension both laterally and medially, so that the possibility of ankylosis due to bone contact is avoided. Post-operative Course: The postoperative course was uneventful. A mouth opening of 30 mm was noted 2 days after surgery. Vigorous postoperative physiotherapy was started to maintain the mobility of the joint. After 7 days with physiotherapy using a wooden spatula, the mouth opening was noted to be 30mm. Later,mouth opening exercises were started. His mouth opening improved to 35mm after 6 months. Figure 9 The patient is on regular monthly followup and he is instructed to continue with the exercises for at least a period of 1 year
Conclusion
As a result of Tmj ankylosis patient’s mouth opening is restricted which carries a mental stigma that overweighs the physical disability posed by the problem. Such patients are psychologically handicapped and hence call for a unique approach to their rehabilitation. A detailed history, clinical and functional examination, radiographic examination facilitating correct diagnosis followed by immediate effective surgical intervention, and physiotherapy can help us to restore the physical, psychological, and emotional health of the Tmj ankylosis patient.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
References
- Malik NA (2002) Textbook of oral and maxillofacial surgery (1st )., New Delhi: Jaypee Brothers Medical Publishers (P) Ltd, pp. 207-218.
- Kaban L, Pogrel MA, Perrott DH (1997) Complications in oral and maxillofacial surgery (1st)., Philadelphia: WB Saunders.
- Zhu S, Wang D, Yin Q, Jing Hu (2013) Treatment guidelines for temporomandibular joint ankylosis with secondary dentofacial deformities in adults. J Craniomaxillofac Surg 41(7): e117–e127.
- Gundlach KKH (2010) Ankylosis of the temporomandibular joint. J Craniomaxillofac Surg 38(2): 122-130.
- Rishiraj B, McFadden LR (2001) Treatment of temporomandibular joint ankylosis: a case report. Journal-Canadian Dental Association 67(11): 659-663.
- Zhang Y, He DM (2006) Clinical investigation of early post-traumatic temporomandibular joint ankylosis and the role of repositioning discs in treatment. Int J Oral Maxillofac Surg 35: 1096-1101.
- El-Sheikh MM, Medra AM, Warda MH (1996) Bird face deformity secondary to bilateral temporomandibular joint ankylosis. Journal of Cranio-Maxillofacial Surgery 24(2): 96-103.
- Zhi K, Ren W, Zhou H, Gao L, Zhao L, et al. (2009) Management of temporomandibular joint ankylosis: 11 years' clinical experience. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 108(5): 687-692.
- Gundlach KK (2010) Ankylosis of the temporomandibular joint. Journal of Cranio-Maxillofacial Surgery 38(2): 122-130.
- Wright GW, Heggie AA (1998) Bilateral temporomandibular joint ankylosis after bimaxillary surgery. Journal of oral and maxillofacial surgery 56(12): 1437-1441.
- Sidebottom AJ, Salha R (2013) Management of the temporomandibular joint in rheumatoid disorders. British Journal of Oral and Maxillofacial Surgery 51(3): 191-198.
- Tripathy S, Yaseen M, Singh NN, Bariar LM (2009) Interposition arthroplasty in post-traumatic temporomandibular joint ankylosis: A retrospective study. Indian Journal of Plastic Surgery 42(02): 182-187.
- El-Hakim IE, Metwalli SA (2002) Imaging of temporomandibular joint ankylosis. A new radiographic classification. Dentomaxillofacial Radiology 31(1): 19-23.
- Susarla SM, Peacock ZS, Williams WB (2014) Role of computed tomographic angiography in treatment of patients with temporomandibular joint ankylosis. J Oral Maxillofac Surg 72(2): 267-276.
- Roychoudhury A, Parkash H, Trikha A (1999) Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: a report of 50 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87(2): 166-169.
- Nitzan DW, Bar-Ziv J, Shteyer A (1998) Surgical management of temporomandibular joint ankylosis type III by retaining the displaced condyle and disc. J Oral Maxillofac Surg 56(10): 1133-1138.
- Kaban LB, Perrott DH (1990) A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg 48(11): 1145-1151.
- Dimitroulis G (2004) The interpositional dermis-fat graft in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg 33(8): 755-760.
- Rattan V (2006) A simple technique for use of buccal pad of fat in long-term viability of temporalis muscle/fascia flap. J Oral Maxillofac Surg 64(9): 1447-1451.
- Lei Z (2002) Auricular cartilage graft interposition after temporomandibular joint ankylosis surgery in children. J Oral Maxillofac Surg 60(9): 985-987.
- Narang R, Dixon RA (1975) Temporomandibular arthroplasty with fascia lata. Oral Surg Oral Med Oral Pathol 39(1): 45-50.
- Raveh J, Vuilleman T, Ladrach K (1989) Temporomandibular ankylosis: surgical treatment and long-term results. J Oral Maxillofac Surg 47(9): 900-906.
- Schobel G, Millesi W, Watzke IM (1992) Ankylosis of the temporomandibular joint (follow-up of thirteen patients). Oral Surg Oral Med Oral Pathol 74(1): 7-17.
- Chossegros C, Guyot L, Cheynet F (1997) Comparison of different materials for interposition arthroplasty in treatment of temporomandibular joint ankylosis surgery: long term follows up in 25 cases. Br J Oral Maxillofac Surg 35(3): 157-160.
- Al-Rawee RY, Al-Khayat AM, salim Saeed S (2019) True bony TMJ ankylosis in children: case report. International journal of surgery case reports 61: 67-72.

 Case Report
Case Report