ABSTRACT
Basal cell carcinoma is the most common type of non-melanoma skin cancer. There are several therapeutic options available for the treatment of non-melanoma skin cancers, such as irradiation, cryotherapy, and topical application of anti-metabolites like 5-Fluorouracil. However, the most common radical treatment approach is surgical excision. In this report, we describe the reconstruction of the wide upper and lower eyelid defects of a patient with basal cell carcinoma using a novel surgical approach that involved the use of a galeal graft and a mucosal flap, which were enveloped with a dermal regeneration template. The eyelid reconstructive surgery achieved satisfactory functional and aesthetic results and no complications were observed during the twelve months following surgery.
Keywords: Basal Cell Carcinoma; Eyelid Defect; Dermal Graft; Dermal Template; Full Thickness Eyelid Defect
Abbreviations: DRT: Dermal Regeneration Template
Introduction
Eyelid defects are congenital, traumatic or, more often, consequences of tumor excision, mainly non-melanoma skin cancer that generally affects the lower lid and the medial or lateral canthus while the upper eyelid is involved in less than 10% of cases. Basal cell carcinoma is the most common type of non-melanoma skin cancer [1]. Several therapeutic options such as irradiation, cryotherapy and topical application of anti-metabolites like 5-Fluorouracil, are used for the treatment of non-melanoma skin cancers. However, the most common radical approach is surgical excision. On the other hand, it is very difficult to find a tissue that can adequately cover the eyeball [2,3]. Several surgical techniques, ranging from the use of local, pedicled or free flaps, to the use of simple or composite grafts, have been proposed in the available literature; however, none of these techniques have been proven to be clearly superior to the other [2-4].The Dermal Regeneration Template (DRT; IntegraⓇ Dermal Regeneration Template, Integra LifeSciences Corporation, Plainsboro, N.J., U.S.A.), which was commercialized in the 1980s, is now an important tool employed in a broad spectrum of cases, from the treatment of scar contractures to the reconstruction of soft tissues loss due to trauma or cancer removal in all anatomical sites. In this report, we describe the first surgical case of a multilayered composite mucosal graft and flaps reconstruction of wide eyelid defects covered by using a DRT for the upper eyelid.
Clinical Case
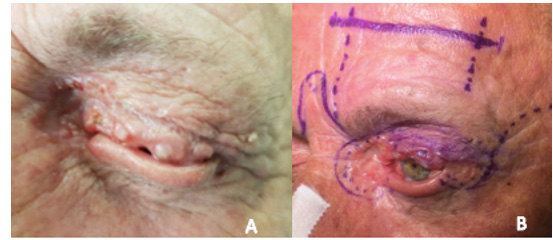
A 64-year-old man was referred to our ophthalmoplasty outpatient clinic for the treatment of an ulcerated left-side eyelid lesion. The patient was a farmer and had fair skin; in addition to his senile age, both are risk factors for skin cancer. He was otherwise healthy and denied symptoms of fatigue, fever, night sweats, weight loss. He reported that the lesion had progressively grown over the previous two years and that he made copiously use of topical treatments as advised by his primary eye care physicians. An external examination revealed that the multifocal lesion involved the entire left upper eyelid, the medial and lateral canthi, and the lower eyelid. We also observed a central ulcer, many small translucent nodules with pearly outer margins, and a complete loss of eyelashes (madarosis) along the free margin of the upper eyelid. In the nose area, we observed a big crater-like lesion with irregular rolled edges that involved the region of the medial canthus, including both lacrimal puncta, lacrimal canaliculi and the medial canthal ligament. An ectropion, tylosis of the free lid margin, and a mold ulcer on the temporal border were noted on the lower lid (Figure 1A). Slit lamp examination revealed a deep and quiet anterior chamber, pseudophakia, and rare hard drusen in the posterior pole on ophthalmoscopy. Intraocular pressure was 17 mmHg bilaterally, and his visual acuity was 0.33 and 0.18 (LogMAR) in the right and left eyes, respectively. The locoregional lymph nodes of the lesion were non-palpable.
Figure 1:
A. Pre-operative clinical photograph.
B. Schematic drawing of the applied surgical procedure.
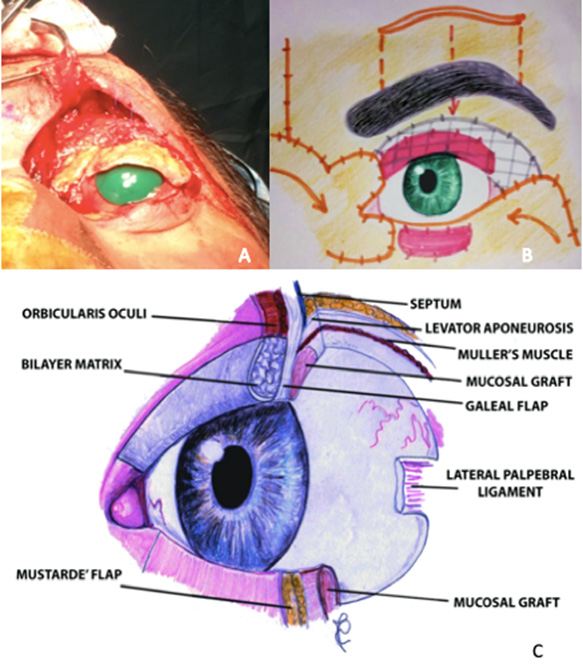
An incisional biopsy confirmed the clinical diagnosis of basal cell carcinoma. Thus, a complete, wide, free margin resection of the lesion was scheduled. After marking the lesion and the surgical plan (Figure 1B), the tumor was excised with a 3 mm safety margin under local infiltration anesthesia (2% lidocaine with epinephrine 1:200,000). Unfortunately, the extemporaneous biopsy results showed an excision margin involvement, leading to an unexpected excision of the entire lower lid. The complete excision of the basal cell carcinoma led to a full-thickness defect, which involved the upper and lower lids, the lateral and medial canthi, and the entire orbital skin (Zones I, II, III, IV, and V according to Spinelli HM et al., 1993). (Figure 2A) Therefore, in order to restore the integrity of the area, a combination of multiple surgical techniques that involve the use of complex flaps was required (Figures 2B & 2C).
Figure 2:
A. Intraoperative Results of Surgical Excision Waiting for Extemporaneous Biopsy.
B. Schematic drawing and section of the reconstruction plans.
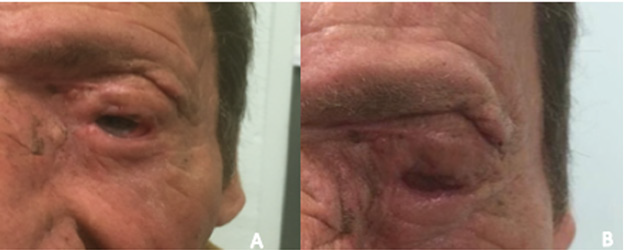
A dovetail-shaped glabellar flap, dissected up to the subcutaneous fat layer, was used to reconstruct the tissue defect in the medial canthal area. An oral mucosal graft was split and used to reconstruct the posterior lamella of the superior and inferior eyelids; thereafter, it was sutured to the remnant conjunctiva. The inferior-anterior lamella and the lateral canthus were reconstructed by using a Mustardé flap [5]. According to Brusati et al. [6], we completed the reconstruction of the anterior layer of the upper eyelid with a forehead galeal flap covered through DRT trimmed to the external surface of the flap size (5x3 cm). Then, a complete suture of the multilayered new free margins was performed to assure corneal protection. (Figure 3) After three weeks, the tarsorrhaphy and the DRT outer silicone layer were removed. A thin epidermal autograft taken from the contralateral eyelid skin was then placed over the new well-vascularized dermis. Intraoperative and early postoperative complications did not occur, and the scar healed well. Furthermore, the patient did not complain of epiphora that interfered with his daily life. The mucosal grafts, although hard to examine, showed good viability and no insertion problems. No local recurrence was reported during the 12 months of follow-up. Upper lid motility was limited but present, maintaining the ability to fully close the eye; no ectropion or entropion of both lids was reported (Figures 4A & 4B).
Discussion
In the present case, the complete excision of the basal cell carcinoma led to a very important full-thickness defect, which involved the upper and lower lids, the lateral and medial canthi, and the entire orbital skin. The method chosen to restore the integrity of the area depends on numerous factors and has to be customized according to the size of the tissue defect, clinical severity, lesion location, and the surgeon’s experience. Reconstructive procedures should provide good eyeball protection, prevent drying, and meet the aesthetic criteria. Therefore, the two-fold layered structure of the eyelid should be considered in the planning of reconstructive surgery because of anatomical and functional reasons [7]. In the case of a full-thickness defect of both superior and inferior eyelids, a single-stage surgical approach should be avoided because of the risk of a greater skin retraction. In the present case, we chose a hard palate mucosal graft as the posterior lamella for both lids, [8,9] given that it could better match the normal tissue. The Mustardé flap was the best option to cover the oral mucosal graft to ensure minimal donor tissue scarring, good reconstruction of the lower lid, and prevention of ectropion or lagophthalmos. For the upper lid, [10] the galeal flap is strong enough to reconstruct the tarsus, and the frontal muscle can still preserve lid elevation. Even if the skin graft healed well, significant depression and retraction with a poor cosmetic outcome were expected; therefore, for the first time we chose a DRT to cover the external surface of the galeal flap [11]. The DRT is perfectly integrated where it is placed, regenerating a tridimensional structure known as “neo-dermis”, in which fibroblasts, lymphocytes, macrophages and neovascularization are clearly detectable. This type of DRT offers multiple advantages. It allows for immediate wound closure, thus preventing fluid loss and restoring the functional barrier of the skin. It also prepares the wound before the positioning of a thin skin graft, improving the final outcome, reducing the risk of necrosis, and improving the scar’s appearance. The engrafted DRT adds softness to the tissues. The main drawback of the DRT is linked to its high cost, followed by the second intervention required for engrafting a skin flap. Notably, the main advantages of the DRT outweigh its disadvantages as it has the potential of filling larger surgical defects without sacrificing aesthetic results and the proper functionality of the lids.
Conclusion
Our experience indicates that, compared to traditional techniques, the DRT can be effective as an adequate reconstruction alternative for challenging cases and can provide good aesthetic and functional results, thereby guaranteeing a normal daily routine and a good quality of life to the patient.
Funding
The authors declare that no fundus, grants, or other support were received during the preparation of this manuscript.
Conflict of Interest
The authors have no financial or non-financial interests to disclose.
References
- Cook BE Jr, Bartley GB (2001) Treatment options and future prospects for the management of eyelid malignancies: An evidence-based update. Ophthalmology 108(11): 2088-2098.
- Brodowski R, Pakla P, Dymek M, Wojnar J, Stopyra W, et al. (2019) “Observations on surgical reconstructive management following the excision of malignant neoplasms of the eyelid and periocular area”. Adv Clin Exp Med 28(4): 535-539.
- Scuderi N, Ribuffo D, Chiummariello S (2005) Total and Subtotal Upper Eyelid Reconstruction with the Nasal Chondromucosal Flap: A 10-Year Experience. Plast Reconstr Surg 115(5): 1259-65.
- Iwanaga H, Nuri T, Okada M, Ueda K (2019) Functional reconstruction of total upper eyelid defects with a composite radial forearm-palmaris longus tenocutaneous free flap: A report of two cases. Microsurgery 39(6): 599-562.
- Mustardé J C (1968) Reconstruction of the upper lid, and the use of nasal mucosal grafts. Br J Plast Surg 21(4): 367-377.
- Brusati R, Colletti G, Redaelli V (2008) Upper eyelid reconstruction with forehead galeal flap. J Plast Reconstr Aesthet Surg 62(7): 901-905.
- Cutler N L, Beard C (1955) A method for partial and total upper eyelid reconstruction. Am J Ophthalmol 39(1): 1-7.
- Shi Y, Zhou X, Yu J, Liu H (2016) Reconstruction of full-thickness eyelid defects following malignant tumor excision: The retroauricular flap and palatal mucosal graft. J Craniofac Surg 27(3): 612–614.
- Fang S, Yang C, Zhang Y, Chunyu Xue, Hongda Bi, et al. (2016) The use of composite flaps in the management of large full thickness defects of the lower eyelid. Medicine (Baltimore) 95(2): e2505.
- Leone C R (1983) Tarsal-conjunctival advancement flaps for upper eyelid reconstruction. Arch Ophthalmol 101: 945.
- Jacobs MA, Christenson LJ, Weaver AL, Appert DL, Phillips PK, et al. (2010) Clinical outcome of cutaneous flaps versus full-thickness skin grafts after Mohs surgery on the nose. Dermatol Surg 36(1): 23-30.

 Case Report
Case Report