Introduction
Chimeric antigen receptor based therapy is the most promising and new treatment for cancer. This therapy is very effective in many types of cancer. And the most innovative part of this treatment is that it can be considered the most effective treatment when other treatments get failed. This treatment gives the most satisfying results and the success rate is very high. This process is directly linked to the immune system of the body. It is a type of cell based therapy that uses the T cells of the immune system, collectively worked in the lab to get hold of cancer cells and destroy them. This treatment involves the alteration of genes inside the T cells resulting in expression of unique cluster of differentiation which identify and investigate tumorigenic cell surface receptors providing immunophenotyping of cells. This therapy is highly used to attack the dangerous cancer cells. Our immune system has the most complicated system yet the simplest one. Our immune system has special powers to identify the foreign substances that usually enter inside the system. This process starts with, where the body finds the antigens that is present on the surface of cells. T cells are very specialized cells of the immune system, they have their specialized proteins. These proteins get attached to the foreign substances and this helps in triggering rest all parts of the immune system, which helps in killing those foreign substances. To better comprehend CAR T-cell therapy, first we have to perform more extensive research about T cells. Lymphocytes, which are white blood cells, play a crucial role in battling infection and disease, including cancer. There are various types of lymphocytes. T cells are one sort of cell.
T cells have special powers, so they travel all through the body looking for and getting hold of damaged cells. Whenever we come in contact to a new illness or disease, our body automatically produces certain amount of T cells to fight with that infection or disease. The mechanism of our body is very clever, so it stores some in reserve mode so that if we again come into contact with the virus, our body will definitely recognize it and kill it right away with very less time from the earlier ones. T cells are very effective at fighting infection. However, during cancer it becomes very difficult for them can to discriminate between a cancer cell and a normal cell. As a result, cancer cells sometimes go unnoticed and unobserved. T cells are being trained in vitro to recognize these deadliest cancer cells by scientists. And one of the novel approaches to this is the CAR cells. These CAR T cells are genetically engineered to get hold of the cancer cells ad help in the treatment. There are certain patient derived immune cells that are designed to express recombinant or chimeric antigen receptors on its surface to recognize and target specific tumor-associated antigens and induce a cell-mediated attack. This ability to reuse T cells has opened up many new techniques for having a very personalized cancer treatment, notably for hematologic malignancies. Furthermore, there is a history of performance of CAR T cells in cancers such as leukaemia and lymphoma, now-a-days there are lots of undergoing clinical trials involved for the treatment of solid tumours. These tumors are quite dangerous and expand rapidly inside the cell. Cancer, from the past years has been established as the main cause of death on a global scale. Several novel treatments and cytotoxic immunotherapies have been developed and commercialized. But till now there has been no complete cure for cancer. It is indeed an epidemic disease in nature.
Cancers has a very complicated behaviour and it involves several genetic and cellular variables in tumorigenesis and metastasis, successful immunotherapy that targets tumors at both the cellular and genetic levels are required. And to revolutionize the whole process, CAR T cell therapy has proven to be a novel approach. In this, the T cells which are obtained from patient blood are altered in vitro to express artificial receptors targeted to a specific tumor antigen. These are able to directly detect the tumor antigen without using the major histocompatibility complex. The application of this therapy in almost all types of cancers has proven to be very effective. This is because; T lymphocytes are genetically engineered to stand as a strong fighter in front of deadliest cancer cells. This novel therapy is known as immunotherapy, gene therapy, or cancer therapy. The human defence system is capable of distinguishing between self and non-self-molecules, such as bacteria, viruses, and aberrant cancer cells. There are certain principles on which human immune system works. Based on the principle of antigenicity sand immunogenecity, tumor cells can be identified with little bit detailing of foreign substances. Cancer cells, on the other hand, are quite clever enough in manipulating our whole immune system for their advantage. These cells make the symptoms quite hard to get noticed in the early days. As a result, situation gets out of control at the later stages. Immunotherapy commonly called as biotherapy has some scientific insights that make it naturally capable of recognizing infections and malignant cells. Immunotherapy has emerged as a major treatment option in recent years. Depending on the condition, each treatment method has advantages and downsides. With an increased understanding of the immune system, several novel immunotherapies are being explored, including techniques for stimulating the immune system to work impertinently to target cancerous cells. CAR T cell therapy has been most successful in treating hematological malignancies; however, research is still going on its efficacy against solid tumors.
Car T Cell Therapy
CAR-T cell therapy has shown promising results for a number of malignancies. This is a medical procedure that engineers T lymphocytes to kill tumor as well as cancerous cells. The initial step in this therapy is to isolate a patient’s peripheral blood. Through the process of apheresis, blood from patients is extracted, divided into its component parts, and genetically modified with CAR construct before being reinserted back into the patient’s body. Apheresis is now a common technique used by blood banks to separate platelets and other blood components for the treatment of a number of illnesses, including hematologic and renal issues. It is acknowledged as a risk-free approach for both healthy people and sick as a result.
Challenges Involved in the Process of Car T Cell Therapy
Although CAR treatment has emerged as a potential anticancer method, it is still not waived off from the problems. The improved performance and efficacy profile office hours CAR T cell treatment are important areas of research that require long-term clinical trial follow-up. Furthermore, CAR T cell therapy has been linked to a number of serious side effects, including neurological toxicity, cytokine release syndrome (CRS), B cell aplasia, tumour lysis syndrome, and allergy. When CAR T cells are multiplied in the body, it helps the other cells to create cytokines that helps in destroying the cancer cells. Few known side effects are fatigue, nausea, headache, fever, and chills, as well as a drop in blood pressure, tachycardia, and capillary leakage. Another uncommon result is CAR T cells affects the metabolism of B cells resulting in aplasia.
Mechanism Involved in the Process of Car T Cell Therapy
The ability of chimeric receptors to fuse or split discrete critical activities, such as identification, co-stimulation, and activation, in separate chains of a receptor molecule expressed on a cell surface by replicating the complexity of the original T cell receptor structure, distinguishes them. T cells are proved to be very advanced and complicated cells of our body which generates maximum iummunity to fight against fatal diseases. It basically doesn’t require any outside formulation for the activation and proliferation of cells. This technique is indeed the most natural process in an artificial treatment. As this treatment uses one’s own immune system to proliferate and perform its mechanism. T cell activation and proliferation require the presence of stimulatory molecules, which also aid in CAR T cell cytokine production. This technique uses an engineered chimeric receptor that works with scFv fragments for T cells. In comparison to other small functional compounds, this mechanism improves the capability of T cells. This mixture of a ‘living medication’ and artificial technique in the immune system fights cancer. Furthermore, CAR T cells can survive in the body as long-term memory cells for several years. Whenever there is any chance if relapse of cancer in the cells, these CAR T cells that has been stored as memory cells helps in the detection and destroying the cancer cells. Another benefit of CAR T cells is that they specifically target tumour cells rather than auto antigens. As a result, it is non-lethal to host cells. Once produced on the surface of an engineered T cell, the synthetic immunoreceptor’s scFv selectively binds to target antigens expressed on a cancer cell.
CAR consists of extracellular antigen-binding domains derived from monoclonal antibodies and intracellular signalling domains connected together by a hinge and a transmembrane domain. The CD3 chain of the T cell receptor complex is present in first-generation CARs, but second-generation receptors have one stimulatory molecule (CD28) and third-generation CARs contain two stimulatory molecules, such as CD28 and OX40. CARs are typically delivered into primary T cells using a vector. CAR-T cells’ cytotoxic effector activity is often maintained by CD3. CD28 (blue) has a role in T cell proliferation and cytokine production. The intricacy of each CAR generation grows due to the presence of costimulatory molecules or the triggered promoter for CAR, chimeric antigen receptor; scFv, single-chain variable fragment; IL, interleukin and transmembrane. The mechanism of genetically engineered CAR T cell is very simple yet the most complicated one. It indeed takes huge research to design a specific cell. And this deadly combination of in vitro and in vivo takes lots of time to be perfect and get inserted inside the host cell. The most interesting part of it is, the efficacy depends on the immune system.
What are the Various Modes of Delivery in this Treatment
Gene therapy works on various methods for the introduction of DNA into cells. The most common method employs recombinant viruses (also known as viral vectors), biological nanoparticles, and non-viral methods based on naked DNA delivery.
The Viral Vector Gene Delivery
In gene therapy, viral vectors such as -retrovirus, lentivirus, and adenovirus vectors are commonly employed. One of the most frequent ways of gene therapy is the retrovirus transduction. In this method a reverse transcriptase is used to enhance the integration of artificial genes inside the host genome. These Retroviral vectors have an inbuilt potential to disrupt the genomic region, resulting in neoplastic transformation. As a result, retroviral vectors play a vital role in the process of gene therapy. There are certain lentivirus that have proven the best in expressing cells of both nature that is dividing and non-dividing cells, which as a result helps a lot in the in vivo and in vitro methods.
Few Methods of Non-Viral Delivery
4.1.1. Transposon Conjugation: Transposon method is a very unique method and it differs greatly from rest others. Transposon delivery is a non-viral technique that combines transposon DNA and a transposase enzyme to convey stable genes. In this process the two important vectors are PiggyBac (PB) and sleeping beauty (SB). Transposons use a cut-and-paste technique to move from one gene location to another.
Electroporation
Electroporation has evolved as an effective method for changing the genes of several cell types. In this process, Electric fields are used to temporarily damage the cell membranes of the target cells. As a result, it helps the charged molecules to enter inside the cells. Human T cell electroporation has been linked to a 40-60% increase in gene expression and an increase in cell viability of up to 80%. The low transfection efficiency and redundant cell injury are two of the disadvantages of electroporation.
Advancements in Car T Cell Therapy
There are Many Advanced and New Versions of CAR T Cell
a. Tandem Car: A single intracellular domain is coupled to a single CAR structure that targets two tumour antigens and, more significantly, its own antigen recognition domain. Researchers are aiming to create a complex technology known as a Tan-CAR, which consists of two distinct antigen recognition sites that are connected by a linker, placed next to one another on an intracellular domain, and produced as a single CAR on the cell surface.
b. Bispecific Car: That is targeting T cells, two CARs are generated simultaneously, each of which has two distinct antigen-recognition domains that target two tumour antigens. When this CAR interacts with two tumour antigens, it can start a cascade of effector chemicals that works synergistically.
c. Crispr Cars: CRISPR is a gene-editing method that modifies a DNA sequence using a guide gRNA. This approach offers a dependable and skilled gene knock-in process as a gene integration technique. The use of CRISPR technology in immunotherapy might be beneficial. CRISPR has been extremely important in the scientific community nowadays.
Advantages of Car T Cell Therapy
The quick turnaround time, single CAR T cell injection, and successful outcomes of CAR T cell therapy over other cancer treatments are its biggest advantages. Additionally, the patient only needs cautious monitoring and care for two to three weeks. Because CAR T cells may stay in the host body for extended periods of time and have a consistent capacity to identify and eliminate cancer cells during recurrence, they are regarded as the muchneeded treatment for cancer, and their efficacy may endure for decades. The use of CAR T cell therapy in those who are unable to receive a transplant has been authorised in the modern world. The CAR T cell therapy has been developed to offer an alternative to other transplants [1,2].
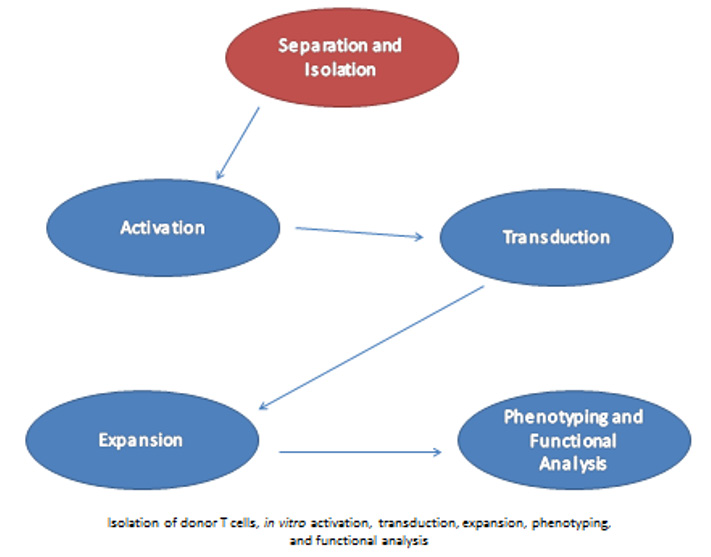
CAR T Cell Generation Flowchart
Flowchart 1.
Protocol for CAR T Cell Generation
a. Isolation of Peripheral Blood mononuclear cells:
• Directly separate lymphocytes from whole Blood.
• Density gradient centrifugation of whole blood sample helps to identify different layers, which signifies the concentrated RBC deposited at the bottom part whereas various WBC and platelets lies in middle.
• Discard the plasma/ water part from the tube after a complete centrifugtaion and collect the platelet part.
• Add a mixture of biotinylated monoclonal antibodies against the non-CD8+ and non-CD4+ T cells to the sample followed by incubation.
• Add MyoneTM SA Dynabeads, which will bind to the antibody labelled cells during short incubation.
• Separate the beads bounded cells on a magnet and discard.
• Remaining sample is now ready to carry forwarded for further process.
b. Activation of T cells:
• Use T Cell TransAct™.
• Lentiviral transduction of activated T cells with a CAR gene construct.
c. Expansion of activated T cells:
• Use serum media to initiate T cell propagation.
• Scale up and exppansion with TexMACS medium (Adapted from serum suspension).
d. Phenotyping and functionality test:
• Use Immunophenotypic markers in T cells.
• Flow cytometry for immunophenotyping.
Conclusion
CAR T CELL therapy has indeed proven to be the most successful treatment in treating cancer. The success rate is quoting high in this process. This technique has proven to be a boon in amidst of dangerous disease. Researchers have got many benefits through this therapy. And still, many researches are going on to get further advancements in this therapy. Cancer, being the most deadly disease, Car T Cell has been a life savior which uses immune cells to get solutions of cancers a highly effective technique that needs more novel innovations. CAR T cells are offered in a variety of scientific frameworks, which can vary greatly between countries. The combination of obstacles and technology necessitates uniformity; yet, CAR T cells provide patients with hope for advanced treatment. Because the first therapy is already on the market, there is a chance that a more precise and improved alternative will become accessible in the coming decades.
References
- Mohanty R, Chowdhury CR, Arega S, Sen P, Ganguly P et al. (2019) CAR T cell therapy: A new era for cancer treatment (Review). Oncol Rep 42(6): 2183-2195.
- Salyka M Sengsayadeth, Bhagirathbhai R Dholaria, Bipin N Savani, Olalekan O Oluwole (2021) Chimeric antigen receptor‐T cell therapies: The changing landscape. eJHaem 3(1): 3-5.

 Review Article
Review Article