ABSTRACT
Background: In the revised version of WHO classification of 2017th the group of high-grade B-cell lymphoma double-hit (HGBL DH) was distinguished from highgrade B-cell lymphoma not otherwise specified (HGBL NOS) based on revealing of rearrangements of genes c-MYC and BCL2 and/or BCL6. Nowadays we have more data telling us that these provisional entities are represented by different types of lymphomas which can develop from low-grade (LGL): follicular (FL) or marginal zone lymphoma (MZL).
Aims: to characterize clinical and laboratory features of c-MYC/BCL2 HGBL DH, HGBL TH, c-MYC/BCL6 HGBL DH and HGBL-NOS and to analyze treatment results of these patients concerning the biological features of disease.
Patients and Methods: We have analyzed the data of 99 patients with HGBLs that have been treated since 2010 till 2022 years in National Research Center for Hematology (Moscow, Russia). 6 patients had HGBL TH, 26 patients - c-MYC/BCL2 HGBL DH, 16 patients - c-MYC/BCL6 HGBL DH and 51 patients - HGBL NOS. We suggested an integral transformation index (ITI) indicating the probability of HGBL development from LGL (FL or MZL). It included following:
1. Histologically confirmed transformation;
2. Lymphoma history longer than 6 months;
3. Discordant bone marrow involvement.
Results: Morphological signs of transformation from LGL more frequently were revealed in of patients with c-MYC/BCL2 HGBL DH + HGBL TH - 14/32 (44%) (from FL) and in patients with c-MYC/BCL6 HGBL DH - 6/16 (38%), in patients with HGBL NOS – in 4/51 (8%) of patients only, p<0,001. Patients with c-MYC/BCL2 HGBL DH and HGBL TH, HGBL NOS were predominantly presented by GCB-subtype (93% and 75%) while c-MYC/BCL6 HGBL DH – by non-GCB (54%), (p=0,002). Double-expressor status was revealed more frequently in c-MYC/BCL2 HGBL DH +HGBL TH – 18/23 (78%) and c-MYC/BCL6 HGBL DH – 5/10 (50%), than in HGBL NOS – 16/51 (35%), p=0,004. Partner of c-MYC rearrangement was IgH gene in majority of c-MYC/BCL6 HGBL DH cases and in 67% of cases HGBL NOS, while in c-MYC/BCL2 HGBL DH +HGBL TH it was non-Ig partner in 50% and IgL gene (κ/λ) in 38% of cases, p=0,02. Paraprotein secretion (PS) was diagnosed in patients with c-MYC/BCL6 HGBL DH (18%) and HGBL NOS (20%) (M κ/λ, Bence-Jones protein λ/κ, IgGκ from trace to 5.6 g/l). PS was associated with spleen (p=0,008) and bone marrow involvement (BM) (p=0,004). In 7/11 (64%) out of cases BM involvement was discordant. Patients with c-MYC/BCL6 HGBL DH had a higher rate of spleen involvement 56% vs 28% and 24%, p=0,03. We observed DLBCL morphology in majority of c-MYC/BCL6 HGBL DH cases (81%), in 44% of c-MYC/BCL2 HGBL DH +HGBL TH cases, while HGBL NOS was represented either by Burkitt-like morphology, or by medium-size centroblasts and no cases of DLBCL were diagnosed in this category, p<0,001.
HGBL NOS had highest median of Ki-67 - 95% (87-100%), c-MYC/BCL2 HGBL DH and HGBL TH – 88% (50-100%), c-MYC/BCL6 HGBL DH – 82% (70-100%), p=0,003. When we estimated all HGBL patients considering additional signs such as a history of lymphoma longer than 6 months and discordant involvement of the BM we revealed that: 20/49 (41%) of patients with HGBL NOS, 19/32 (59%) of patients with c-MYC/ BCL2 HGBL DH and HGBL TH, 13/16 (81%) of patients with c-MYC/BCL6 HGBL DH had at least one sign of transformation. ITI significantly increased the probability to reveal the transformation from LGLs in patients with c-MYC/BCL6 HGBL DH (p=0,03) and HGBL NOS (p<0,001) but it didn’t influence on prognosis. TP53 mutations were revealed with compared frequency in all three groups and increased the probability of relapse or progression in patients with c-MYC/BCL2 and c-MYC/BCL6 HGBL DH.
Conclusion: According to clinal, morphological and cytogenetic data c-MYC/BCL2 HGBL DH and HGBL TH are more homogenous group of GCB-lymphomas that have a pathogenic link with FL and in majority of cases are represented by transformation of FL. C-MYC/BCL6 HGBL DH resembles DLBCL and in some cases can be represented by transformation of LGL. HGBL NOS is represented by lymphomas with aggressive morphology and clinical manifestation but has more illegible profile. We proposed to consider additional discordant involvement of the BM and a long (at least 6 months) history of the disease as signs of transformation. All the above justifies the use of some of the therapeutic approaches used for the treatment of FL and LMZ for the treatment of patients with c-MYC/BCL2 HGBL DH, c-MYC/BCL6 HGBL DH, and HGBL NOS.
Keywords: Side Effects; Adversary Reactions; Antiretrovirals; Arrhythmias
Abbreviations: HGBL DH: High-Grade B-Cell Lymphoma Double-Hit; HGBL NOS: High-Grade B-Cell Lymphoma Not Otherwise Specified; MZL: Marginal Zone Lymphoma; ITI: Integral Transformation Index; PS: Paraprotein Secretion; DLBCL: Diffuse Large B-cell Lymphoma; FL: Follicular lymphoma; NGS: Next-Generation-Sequencing; CR: Complete Remission; OS: Overall Survival; PR: Partial Remission; FISH: Fluorescent in Situ Hybridization; ITI: Integral Transformation Index; EFS: Event-Free Survival; CNS: Central Nervous System; LDH: Lactate Dehydrogenase; PFS: Progression Survival; DEL: Double-Expressor Lymphoma
Introduction
In the revised version of WHO classification the group of highgrade B-cell lymphoma double-hit (HGBL DH) was distinguished from high-grade B-cell lymphoma not otherwise specified (HGBL NOS) based on revealing of rearrangements of genes c-MYC and BCL2 and/or BCL6. HGBL DH comprise the cases with intermediate (BCLU), DLBCL and blastoid morphology [1]. Data on the biodiversity of lymphomas is expanding, and with the use of modern analytical platforms such as next generation sequencing, whole exome sequencing, it has become possible to determine the molecular and mutational profile of the tumor, in addition to identifying repetitive translocations used in routine diagnostics. Since 2017 year several research groups have differentiated diffuse large B-cell lymphoma (DLDCL) into 6 molecular subtypes with distinct pathogenic mechanisms and outcomes (C0 – no alterations, C1=BN2 (ABC), C2=TP53/CDKNA2 alterations, C3=EZB (GCB), C4=GCB other, C5=MCD (ABC)) [2-5]. The C1 (BN2) groups within in the ABC group but has superior prognosis, the C3 (EZB) group is within GCB-type with inferior prognosis. This segregation helps to explain clinical heterogeneity of DLBCL. Interestingly, the genetic aberrations of several DLBCL subtypes reveal potential pathogenetic links to indolent lymphomas. Mutations specific to BN2 associate this subtype with marginal zone lymphoma (LMZ). Translocations involving the BCL6 gene locus, detected in the BN2 subtype, are rare in indolent LMZ, but often occur in patients with LMZ when it has turned into an aggressive large cell variant [6,7]. Follicular lymphoma (FL) shares many genetic aberrations with the EZB subtype and, in cases of disease transformation, may histologically resemble both DLBCL and HGBL.
Differences between c-MYC/BCL2 and c-MYC/BCL6 HGBL DH were identified by Pillai R K, et al. [8]. The authors characterized 6 cases from the University of Pittsburgh Medical Center and 17 cases from the Mitelman c-MYC/BCL6 HGBL DH database. c-MYC/ BCL6 HGBL DH proceeded aggressively with frequent involvement of extranodal regions. However, in contrast to c-MYC/BCL2 HGBL DH, they were more likely to be CD10-negative but express IRF4/ MUM-1+ (p = 0.03). The authors also suggested that HGBL TH is pathogenetically related to c-MYC/BCL2 HGBL DH. Künstner et colleagues in 2021 performed whole-exome sequencing and deep panel next-generation-sequencing (NGS) of 47 clinically annotated cases of HGBL with MYC and BCL2 and/or BCL6 rearrangements. They provided evidence of a molecular divergence between BCL2 and BCL6 rearranged HGBL DH. Beyond a significant congruency with the C3/EZB DLBCL cluster in BCL2 rearranged cases on an exome-wide level, they observed an enrichment of the SBS6 mutation signature in BCL6 rearranged cases. SBS6 is associated with defective DNA mismatch repair and is found in microsatellite unstable tumors [9]. Differential gene set enrichment and subsequent network propagation analysis according to cytogenetically defined subgroups revealed an impairment of TP53 and MYC pathway signaling in BCL2 rearranged cases, whereas BCL6 rearranged cases lacked this enrichment, but instead exhibited showed impairment of E2F targets. Oncogenic drivers, mutational signatures and perturbed pathways were compared with data from follicular lymphoma (FL), diffuse large-B-cell lymphoma (DLBCL) and Burkitt lymphoma (BL) [9]. C-MYC/BCL2 HGBL DH usually attended to GCB lymphomas. They had definite gene expression signature which distinguish them from other GCB DLBCL and which is also typical for dark-zone lymphomas [10- 13]. C-MYC-rearrangement pattern could be distinct from Burkitt lymphoma and more frequently be related with non-Ig partner [11]. In pathogenesis of c-MYC/BCL2 HGBL DH plays an important role pre-existing BCL2 translocation. There are descriptions of clinical cases c-MYC/BCL2 HGBL DH development from FL in situ and up to one third of cases are represented by transformation of follicular lymphoma (tFL) [14,15]. Also, there are common mutations between c-MYC/BCL2 HGBL DH and FL in genes, evolving in epigenetic regulation, cell proliferation and apoptosis, such as BCL2, KMT2D, CREBP, EZH2, etc. [16]. Thus, FL and c-MYC/ BCL2 HGBL DH have common mutational profile.
According to the literature date the group of tFL counts from 11 to 30% of patients in studies devoted to the treatment of HGBL DH [17]. The meaning of revealing double-/triple translocations in untransformed FL is unclear. Analysis of publications showed that these lymphomas have a high potential to collect additional mutations and to transformation to more aggressive lymphomas. Transformed FL have the same poor prognosis as HGBL DH [17]. Rusconi et al., (2019) mentioned that the prognosis of TFL depended on the length of the period preceding transformation (the longer it is, the more favorable the prognosis of the disease), as well as the number of lines of previous therapy [18]. Li et al. (2016) identified prognostic factors for the c-MYC/BCL2 HGBL DH such as leukocytosis, elevated LDH activity, CNS involvement, widespread disease. Petrich et al. established that the most powerful prognostic factor was a chemosensitivity of the tumor (an achievement of complete remission (CR) after the first-line treatment) [19]. HGBL DH is a less homogeneous group compared to c-MYC/BCL2 and c-MYC/BCL6 HGBL DH, which are more well-defined in molecular profile and mutational landscape [5]. To date, it is difficult to trace certain patterns in this category, and rather, it is a basket of cases united by common morphological and phenotypic features, probably it contains certain amount of tFL and MZL.
Since 2014 to 2015 years, it has been made different attempts to improve the treatment results by chemotherapy intensification [19,20]. Event-free (EFS) was improved by R-DA-EPOCH and doseintensified (DI) therapeutic approaches comparing with R-CHOP-21. That was shown by different research groups. An autologous stem cell transplantation (auto-SCT) didn’t show any profit compared with observation. The role of CNS prophylaxis is recommended and highlighted by hematological community. But the group of patients with primary CNS involvement has a poor prognosis. The auto-SCT improved overall survival (OS) in patients with partial remission (PR) of HGBL DH MYC/BCL2, especially transformed from FL.Today the standard care for HGBL DH is not established (NCCN Guidelines version 5.2021). R-DA-EPOCH and toxic regimens applied in BL are possible to prescribe in cases with a good performance status. Nevertheless in 50% of patients the therapy with R-CHOP is effective. So, some clinicians recommend this therapeutic strategy in combination with 2 HD-MTX courses with or without auto-SCT and participation in clinical trials continue to be promising option.
Aim
The purpose of our study was to characterize clinical and laboratory features of c-MYC/BCL2 HGBL DH, HGBL TH, c-MYC/ BCL6 HGBL DH and HGBL-NOS and to analyze treatment results of these patients concerning the biological features of disease.
Patients and Methods
For 2010 year till present in National Research Center for Hematology, Moscow, Russian Federation have been treated 99 patients: 6 patients with HGBL TH, 26 patients had HGBL DH MYC/BCL2, 16 patients with HGBL DH MYC/BCL6 and 51 patients with HGBL NOS. The diagnosis was confirmed by histological and immunohistochemical study in all cases. Fluorescent in situ hybridization (FISH) was performed in all patients to reveal translocation of genes c-MYC (8q24), BCL2 (18q21) and BCL6 (3q27). In 20 patients was performed Sanger sequencing of gene TP53 (from 4 to 9 exons) to reveal any mutations. In 9 cases we had a convenient biopsy sample to evaluate 17p13 (TP53) deletion status. Also, for more precise diagnostics of the prevalence of lymphoma we used flow cytometry to reveal lymphoma population in peripheral blood, bone marrow and cerebrospinal fluid. We suggested an integral transformation index (ITI) indicating the probability of HGBL development from LGL (FL or MZL). It included following:
1. Histologically confirmed transformation (by two consequent biopsies or morphological signs of high- and low-grade lymphomas in one biopsy sample);
2. lymphoma history longer than 6 months; 3. discordant bone marrow involvement (infiltration by small B-cells).
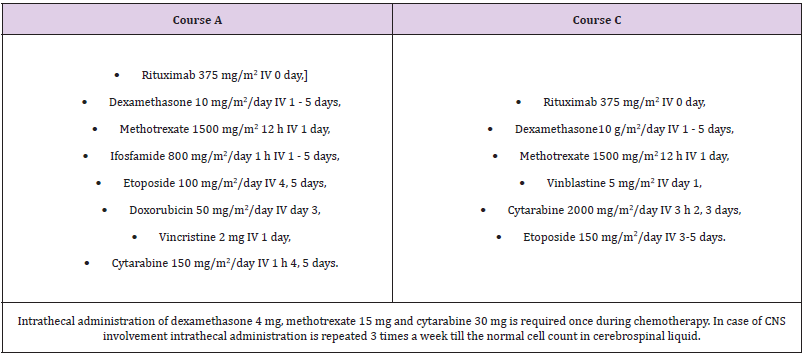
In 22 patients PET-CT results were available before treatment. Till 2018 year we have had a trend to prescribe Burkitt-like regimens similar as CODOX-M/IVAC or Hyper-CVAD in young and fit patients (Table 1 & 2). For 2018 year it was initiated randomized prospective trail «R-Burkitt Lymphoma-Moscow-04 Versus R-(DA)-EPOCH and Autologous Stem Cells Transplantation in Patients with High-Grade B-cell Lymphoma Double-hit (HGBL DH) and High-Grade B-cell Lymphoma Not Otherwise Specified (HGBL NOS) », NCT03479918. All patients signed informed consent to participate in the clinical study. This study had a restriction concerning of somatic status, age and comorbidity that should make possible intensified therapeutic intervention. Also, the prevention of recurrence of CNS consequences, as well as the use of high-dose methotrexate for therapeutic purposes, limits the use of R-DA-EPOCH in patients with a high CNS index IPI, as well as with CNS involvement at the time of disease onset. Thus, the feasibility of the protocol was limited by the above reasons. Also, there were unplanned deviations from the protocol due to the lack of intrathecal prevention of secondary CNS involvement in several cases, due to the lack of the possibility of its implementation.
Most of the patients received intensive regimens of immunochemotherapy. Thus, 56 patients were treated with BLM- 04+R or m-NHL-BFM-90+R, 23 with R-DA-EPOCH, 18 with R-CHOP-21, and 2 with other treatment protocols. In some patients, based on the anamnesis, clinical indications, and the decision of the medical commission, an integrated approach was used to combine immunochemotherapy with lenalidomide or ibrutinib, adding polatuzumab vedotin. Auto-HSCT was performed in 27 patients. Statistical analysis was performed in STATISTICA 12.0 software. Compassion between clinical characteristics was performed using χ2 test and ANOVA. Survival analysis was carried out using Kaplan- Meyer method and Log rank test. Differences were considered as significant at p-value < 0.05. When analyzing event-free survival (EFS), disease progression, relapse, and death from any cause were considered.
Results
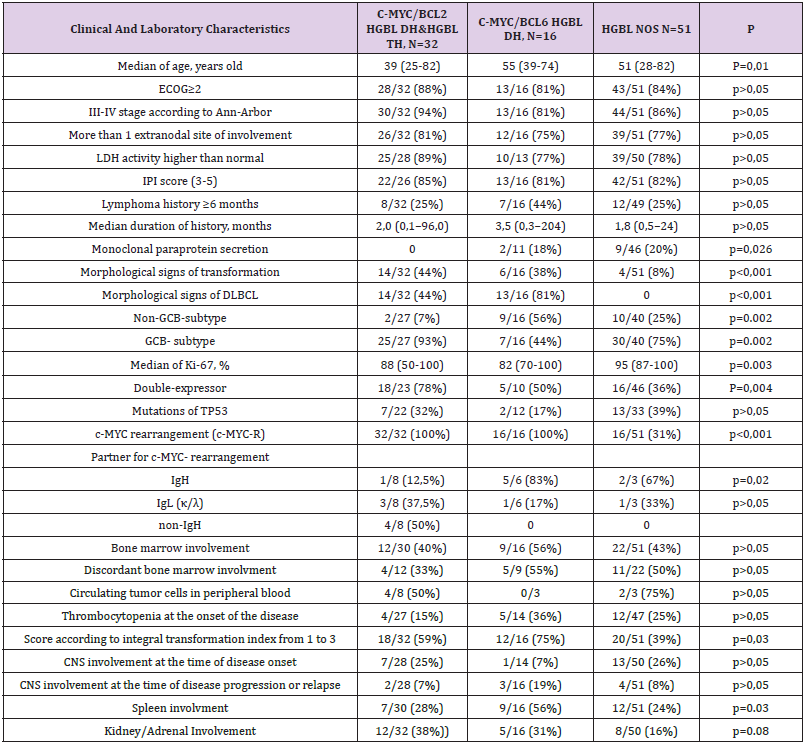
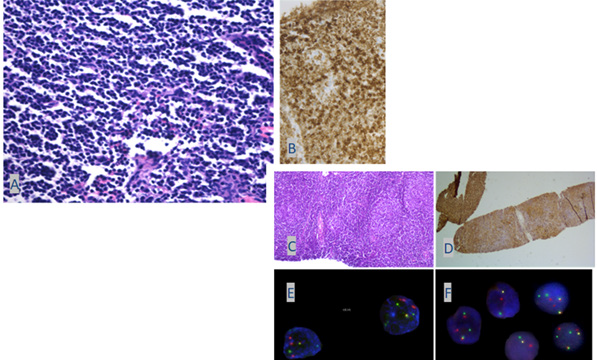
According to classical clinical and laboratory characteristics, patients with HGLs had a widespread tumor according to the Ann- Arbor classification, a high frequency of involvement of extranodal areas, the central nervous system (CNS) (Figure 1) and bone marrow involvement (which were strongly associated, p<0,001), high activity of lactate dehydrogenase (LDH), were belonged to the high-risk group according to the International Prognostic index (IPI) (Table 3). Patients with c-MYC/BCL2 HGBL DH and HGBL TH were younger than those in the c-MYC/BCL6 and HGBL NOS groups, p=0.01. Morphological signs of transformation from LGL more frequently were revealed in of patients with c-MYC/BCL2 HGBL DH + HGBL TH - 14/32 (44%) (from FL) (Figure 2) and in patients with c-MYC/BCL6 HGBL DH - 6/16 (38%), in patients with HGBL NOS – in 4/51 (8%) of patients, p<0,001.Patients with c-MYC/BCL2 HGBL DH and HGBL TH, HGBL NOS were predominantly presented by GCB-subtype (93% and 75%) while c-MYC/BCL6 HGBL DH – by non-GCB (54%), (p=0,002). Double-expressor status was revealed more frequently in c-MYC/BCL2 HGBL DH +HGBL TH – 18/23 (78%) and c-MYC/BCL6 HGBL DH – 5/10 (50%), than in HGBL NOS – 16/51 (35%), p=0,004. Partner of c-MYC rearrangement was IgH gene in majority of c-MYC/BCL6 HGBL DH cases and in 67% of cases HGBL NOS, while in c-MYC/BCL2 HGBL DH +HGBL TH it was non-Ig partner in 50% and IgL gene (κ/λ) in 38% of cases, p=0,02.
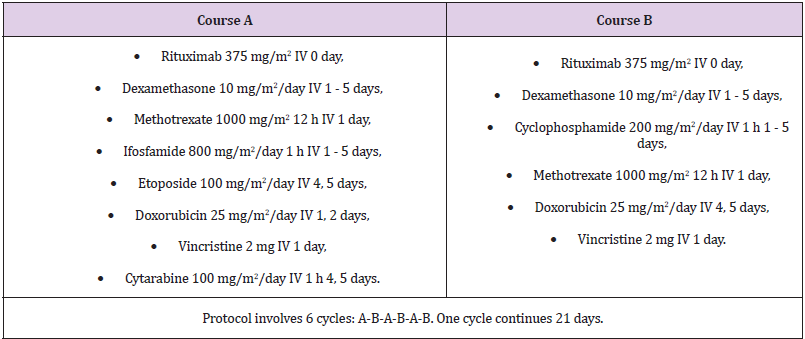
Table 3: Comparative characteristics of patients with c-MYC/BCL2 HGBL DH&HGBL TH, c-MYC/BCL6 HGBL DH и HGBL NOS.
Figure 1: Clinical portrait of a patient with c-MYC/BCL2 HGBL DH with multiple extranodal lesions (scapula, soft tissues, CNS). Tumor B-lymphocytes in the biopsy of the cerebrospinal fluid according to the cytological study.
Figure 2: An example of follicular lymphoma (cytological type 2) transformed into c-MYC/BCL2 HGBL DH after 9 years of follow-up.
A. Peripheral lymph node biopsy at the onset of the disease is represented by follicle-like structures without clear boundaries, represented by cells of different sizes (centrocytes and centroblasts), foci of large, atypical cells (hematoxylin-eosin staining).
B. Immunohistochemical staining with antibodies to BCL2 (cytoplasmic expression),
C. Cor biopsy specimen with diffuse infiltrate of large cells with rounded, irregularly shaped nuclei, high mitotic activity (8–9 mitotic figures in x400 field of view), morphological signs of apoptosis.
D. Staining with antibodies to Ki-67 (proliferative activity index up to 90%).
E. According to the FISH results, t(8;14) (q24;q32) translocation was detected.
F. according to the FISH results, a translocation involving the BCL2/18q21 gene locus was detected.
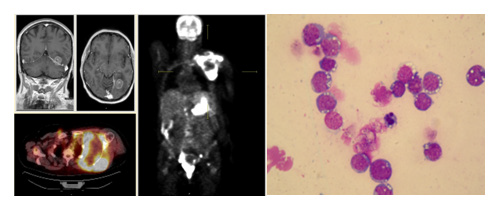
Figure 3:
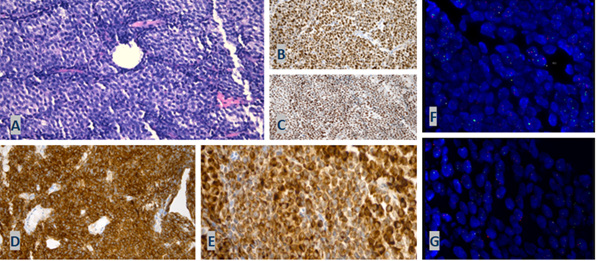
A. Morphological picture of c-MYC/BCL2 HGBL DH, staining with hematoxylin-eosin (the tumor is represented by a diffuse lymphoid proliferation of an average size of fairly monomorphic cells with blast morphology (lymphoblastoid morphology), the presence of mitotic figures. Compartmentalization of the tumor tissue due to thin fibrous layers is noted);
B. Immunohistochemical staining with antibodies to Ki-67 (proliferation index of 90–95% of positive cells);
C. Immunohistochemical staining with antibodies to c-MYC (over 90% of positive cells, intense nuclear reaction);
D. Immunohistochemical staining with anti-CD10 antibodies (membrane expression);
E. Immunohistochemical staining with antibodies to BCL2 (cytoplasmic expression).
F. FISH revealed a translocation involving the BCL2/18q21 gene locus and one additional signal from the centromeric part of the BCL2/18q21 gene locus (additional derivative of chromosome 18);
G. FISH revealed a translocation involving the MYC/8q24 gene locus.
We observed DLBCL morphology in majority of c-MYC/BCL6 HGBL DH cases (81%), in 44% out of c-MYC/BCL2 HGBL DH +HGBL TH cases (Figure 3), while HGBL NOS was represented either by Burkitt-like morphology, or by medium-size centroblasts and no cases of DLBCL were diagnosed in this category, p<0,001. HGBL NOS had higher median of Ki-67 - 95% (87-100%), compared with c-MYC/BCL2 HGBL DH and HGBL TH – 88% (50-100%), c-MYC/ BCL6 HGBL DH – 82% (70-100%), p=0,003.
Paraprotein secretion (PS) was diagnosed in patients with c-MYC/BCL6 HGBL DH (18%) and HGBL NOS (20%) (M κ/λ, Bence-Jones protein λ/κ, IgGκ, from trace to 5.6 g/l). Paraprotein secretion was associated with spleen (p=0,008) and bone marrow involvement (p=0,004). In 7/11 (64%) of cases bone marrow involvement was discordant BM. Patients with c-MYC/BCL6 HGBL DH had higher rate of spleen involvement 56% vs 28% and 24% in c-MYC/BCL2 HGBL DH and HGBL NOS, p=0,03. When we estimated all HGBL patients considering additional signs such as a history of lymphoma longer than 6 months and discordant involvement of the bone marrow we revealed that: 20/49 (41%) of patients with HGBL NOS, 19/32 (59%) of patients with c-MYC/BCL2 HGBL DH and HGBL TH, 13/16 (81%) of patients with c-MYC/BCL6 HGBL DH had at least one sign of transformation. ITI significantly increased the probability to reveal the transformation from LGLs in patients with c-MYC/BCL6 HGBL DH (p=0,03) and HGBL NOS (p<0,001) but it didn’t influence on prognosis. In some patients who underwent flow cytometry of bone marrow cells, two tumor clones of B-lymphocytes were detected, which indicates the ongoing clonal evolution of the disease. Interesting that we detected different tumor clones in different loci of lymphoma presentation. Thus, it was detected one B-cell clone in peripheral blood and pleural fluid, and another were found in cerebral fluid. Analyzing PET-CT data, we observed the difference between maximum and minimum FDG accumulation was at median of 5,5-fold (2-10). Probably there is a relationship between the presence of indolent lymphoma in some loci and degree differences between the maximum and minimum levels of FDG accumulation according to PET-CT.
The Effectiveness of Therapeutic Approaches
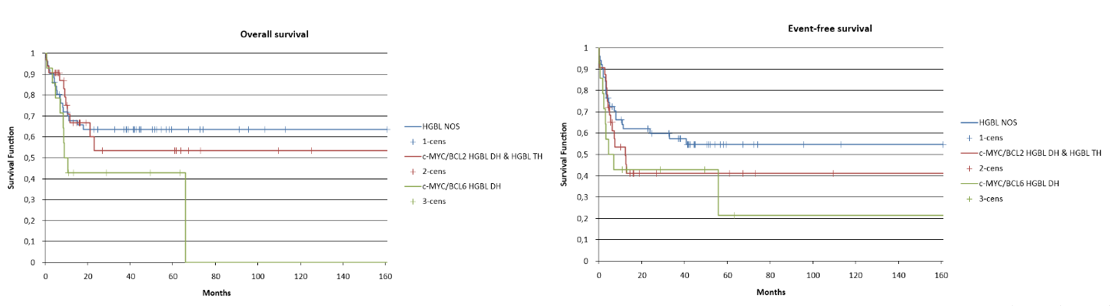
According to our data, the 5-year OS in HGBL NOS patients was 62%, in patients c-MYC/BCL2 HGBL DH and HGBL TH patients - 52%, and c-MYC/BCL6 HGBL DH - 42% (p>0.05); 5-year EFS was 52%, 41% and 22%, respectively, (p>0.05) (Figure 4). When assessing the rate of complete remissions with the use of various types of therapy (BL-M-04 with rituximab/R-NHLBFM- 90 vs R-(DA)-EPOCH, vs R-CHOP), despite the superiority of methotrexate-containing therapeutic approaches, no significant differences were found, probably, due to the limited number of observations. Response to induction chemotherapy was a strong predictor of survival, p<0.05. Interestingly, that relapses occurred only in the HGBL NOS cohort - 6 cases, including two relapses into the CNS - 20 and 8 months after the end of treatment. In a third of relapse cases, it was possible to achieve remission of the disease, while patients “double- hit” and “triple-hit” lymphomas had no delayed events, and treatment failure had a primary progressive nature which were practically incurable.
Figure 4: Overall and event-free survival of patients with c-MYC/BCL2 HGBL DH+HGBL TH, c-MYC/BCL6 HGBL DH and HGBL NOS (p>0,05).
TP53 mutations were revealed with compared frequency in all three groups and increased the probability of relapse or progression in patients with c-MYC/BCL2 and c-MYC/BCL6 HGBL DH, p<0,05. Interestingly that OS and EFS in cases with HGBL DH developed due to transformation of FL didn’t differ as we showed in previous publications than in de novo HGBL DH/TH [21]. The role of auto- HSCT is difficult to assess because primary progressive course of the disease in some cases didn’t allow to use this therapeutic option. In the c-MYC/BCL2 HGBL DH+HGBL TH group, auto-HSCT was performed in 15 patients, 8 of them were in partial remission, 5 out of 8 had disease progression despite auto-HSCT. In evaluating the role of prevention of secondary CNS involvement, we analyzed a population of 89 patients in whom it was possible to assess the status of CNS involvement at the onset of the disease. Most patients were prevented/treated for CNS involvement with HD-Mtx (1.0–1.5 g/m2), which was administered to 51/89 patients (57%), in 26/89 (29%) of patient’s methotrexate was administered systemically and endolumbally as part of a chemotheraputic triplet; in 22/89 (25%) of patients - only endolumbally. 18/89 (20%) patients did not receive any prophylaxis for a several reasons. The risk of secondary CNS involvement was high in all groups (p>0.05).
In 16 patients CNS involvement was detected at the onset of the disease: ten of them received methotrexate systemically and intrathecally, 6 received treatment only with intrathecal triplet administration due to advanced age and aggravated somatic status. The incidence of CNS involvement due to disease recurrence/progression was 4/51 (8%) in the HD-Mtx group, 1/22 (5%) in the intrathecal prophylaxis group, and 5/17 (29%) in group without any prophylaxis due to the lack of the possibility of its implementation (moreover, 2 two patients relapsed in the central nervous system occurred in the delayed period - after 20 and 8 months). Thus, despite 4 cases of resistance to systemic administration of methotrexate at a dose of 1.0-1.5 g/m2 (in 8% of patients), the probability of relapse involving the CNS after its use was statistically significantly reduced, p=0,02. Intrathecal administration of the triplet also showed benefits in the prevention of CNS relapses compared with no prevention, p = 0,04. Two out of 6 patients with CNS involvement at the onset of the disease, who were unable to undergo high-dose chemotherapy, achieved complete remission of the disease, as well as sanitation of the cerebrospinal fluid after R-CHOP therapy in combination with intrathecal triplet administration (one patient with HGBL NOS, one with HGBL TH). In the latter case, polatuzumab vedotin and lenalidomide were additionally used in therapy due to its ability to penetrate the blood-brain barrier.
Discussion
Thus, our analysis revealed the clinical heterogeneity of the groups of patients with c-MYC/BCL2 HGBL DH and HGBL TH, c-MYC/BCL6 HGBL and HGBL NOS. The c-MYC/BCL2 HGBL DH and HGBL TH had a close pathogenetic relationship with FL, as indicated by various co-authors. Among our patients, some had not only histological signs of transformation, but also a long-term (up to 9 years) history of FL. Lower median of age in this group (39 years old) compared with 60 years old, according to the literature data, may be due to some selection of patients on admission. The c-MYC/BCL2 HGBL DH and HGBL TH group was predominantly represented by the GCB subtype, with a certain c-MYC gene rearrangement pattern (predominantly non-IgG or IgL partner), which is consistent with the literature data. In most cases, a blastoid morphological type of tumor was detected, morphological features of DLBCL were detected in 44% of the patients. In 2 patients, several tumor populations were identified in the bone marrow, which indicates a clonal evolution of the disease. These tumors can consist of several clones with different mutational profile due to opportunity of divergent lymphoma subclones development and therefore different chemosensitivity. It can be partly reflected by clinicians when tumor foci with different intensity of accumulation of the radiopharmaceutical are detected according to PET-CT data and revealing of several tumor clones in biopsy samples according to flow cytometry.
In the c-MYC/BCL6 HGBL DH group, there were cases of transformation from both FL and MZL. Interestingly, most of patients showed a morphological pattern of DLBCL with a median value of the proliferative activity index of 82%, which was lower than in other groups and more convinient with DLBCL. The partner for rearrangement of the c-MYC gene in most cases was the IgH gene. More than half of the patients had tumor involvement of the spleen and 18% of patients had monoclonal paraprotein secretion. According to Wright, et al., 2020, the c-MYC/BCL6 HGBL DH mutation profile is similar to the MZL mutation profile, despite the fact that there were no morphologically confirmed cases of MZL transformation in the group studied by the authors [5]. In our study, cases of MZL transformation into c-MYC/BCL6 HGBL DH were verified. The HGBL NOS group is less well defined. All cases in it are united by morphological features of “aggressive lymphoma”. So, the tumor was presented either by a Burkitt-like morphological picture, or by medium-sized centroblasts. The median proliferative activity index was 95%. Interestingly, a quarter of the patients had a long history of the disease (more than 6 months), which indicates that morphological cases of transformation of indolent lymphomas can also occur in this group.
Response to first-line therapy correlated with TP53 mutation status. The accurate testing of mutational profile should be widely applicated in diagnostics of HGBL DH/TH or NOS, especially for TP53 mutation status to learn more about tumor diversity, to estimate a prognosis, and to get a potential for individualized treatment. The data obtained by us are not only of scientific importance but can be applied to the development of therapeutic approaches that consider the pathogenesis of a particular type of HGBL.As we can trace the connection in pathogenesis between FL and c-MYC/BCL2 HGBL DH, we can assume a potential benefit from the application of new drugs used in the FL treatment. We had a very different experience ranged from positive to dramatic in the treatment of c-MYC/BCL2 HGBL DH and HGBL TH. Thus, we have seen CR achievement in two patients with HGBL TH: one underwent R-CHOP-21 (№6) with polatuzumab and lenalidimide and another - conventional treatment with R-CHOEP-21 (№8), resulted with PR, followed by HD-Mtx and auto-SCT. In both cases was diagnosed wild type of TP53. Although we observed treatment failure in c-MYC/ BCL2 HGBL DH and HGBL TH after DI regimens and consequent therapy including CAR-T therapy, auto-SCT and salvage.
According to current studies, prevention of secondary CNS involvement is recommended for patients with HGBL DH and can reduce the risk of an adverse event to 5.4% [22,23]. Despite of this HD-Mtx-containing treatment does not cure CNS involvement in all cases. We couldn’t to achieve a CR in young patient with primary CNS involvement with intratumor and leptomeningeal infiltration using HD-Mtx-containing treatment. We observed an appearance of TP53 mutation (that hasn’t been revealed in primary biopsy) in progression of c-MYC/BCL2 HGBL DH resulting in enlargement of tumor in CNS, despite of HD-Mtx-containing treatment. Thus, in patients with CNS involvement, the addition of drugs that cross the blood-brain barrier to methotrexate should be considered. Considering heterogeneity of patients in concerning to chemotherapy response, all cases of CR achievement using new therapeutic approaches (immunotherapy, target-therapy, immunomodulating treatment) should be validated on the lager cohort of patients in a randomized trial. There is a data that lenalidomide can improve treatment results in DLBCL patients [24]. Also, lenalidomide maintenance for 24 months after obtaining a CR or PR to R-CHOP significantly prolonged PFS in elderly patients with DLBCL [25].
Clinical trail «Polatuzumab Vedotin and Combination Chemotherapy for the Treatment of Previously Untreated Double or Triple Hit Lymphoma» (ClinicalTrials.gov Identifier: NCT04479267) will expand our knowledge about the role of immunoconjugates in the therapy of HGBL DH/TH. Younes et colleagues in 2019 showed that in patients age younger than 60 years, ibrutinib plus R-CHOP improved EFS, PFS, and OS with manageable safety. In patients age 60 years or older, ibrutinib plus R-CHOP was associated with increased toxicity, leading to compromised R-CHOP administration and worse outcomes [26]. Unfortunately, this work does not provide information on the presence of a mutation/deletion of the TP53 gene. The findings from this monocentric retrospective study performed by Porpaczy and colleages in 2021 indicate that TP53 mutation status does not seem to affect outcomes in DLBCL patients treated with CAR T-cell therapy [27]. According to our center, we had a negative experience with CAR-T cell therapy in a patient with a progressive course of HGBL DH and the presence of a TP53 mutation and deletion. Perhaps the clinical effect could be achieved with earlier use of CAR-T therapy.
Thus, the analysis of therapy failures serves as a basis for us to search for new approaches. Nowadays an attempt to improve therapeutic results considering LymphGen algorithm give promising results [5]. An addition of tucidinostat (histone deacetylase inhibitor) to patients with double-expressor lymphoma had a benefit especially in double-expressor group, according to Zhang MC et colleagues, 2020 [28]. Thus, according to the study data among 49 patients, the complete response rate was 86%, with overall response rate achieving 94%. The 2-year progression survival (PFS) and overall survival (OS) rates were 68% (95% CI 52-79) and 83% (95% CI 68-91). Comparing with historical control (NCT01852435), the 2-year PFS and OS rates of double-expressor lymphoma (DEL) were improved, and negative prognostic effect of histone acetyltransferases CREBBP/EP300 mutations was also mitigated by CR-CHOP. Continuing the theme of the use of genetic diagnostics in order to select therapy encouraging results have been reported from the phase 2 Guidance-01 clinical trial (NCT04025593) [28]. This was a randomized phase II study comparing R-CHOP-X with R-CHOP in newly diagnosed DLBCL.
Targeted sequencing was performed used a simplified method to classify patients into six genetic subtypes MCD, BN2, N1, EZB, TP53 and NOS, using mutations in 18 genes, BCL2 translocation, and BCL6 fusion. MCD and BN2 patients were treated with BTK inhibitor ibrutinib 420 mg/d, N1 and NOS patients with immunomodulatory agent lenalidomide 25mg d1-10, EZB patients with histone deacetylase inhibitor tucidinostat 20mg d1, 4, 8, 11, and TP53 patients with intravenous demethylating agent decitabine 10 mg/ m2 d1-5 followed by standard R-CHOP. The complete and overall response rates were 85% and 91% in R-CHOP-X arm, and 65% and 72% in R-CHOP arm, respectively. With a median follow-up of 14.1 months, 1-year PFS and OS rates were 96% and 98% in R-CHOP-X arm, and 79% and 94% in R-CHOP arm, respectively (PFS: HR 0.22, 95%CI 0.09-0.61; OS: HR 0.28, 95%CI 0.05-1.60). However, the limitation of this study is the selection by somatic status, as well as the lack of information on the presence of a prognostically unfavorable group of c-MYC/BCL2 HGBL DH or TH as well as data about patients with CNS involvement.
Conclusion
According to clinal, morphological and cytogenetic data c-MYC/ BCL2 HGBL DH and HGBL TH are more homogenous group of GCBlymphomas that have a pathogenic link with FL and in majority of cases are represented by transformation of FL. C-MYC/BCL6 HGBL DH resembles DLBCL and in some cases can be represented by transformation of LGL. HGBL NOS is represented by lymphomas with aggressive morphology and clinical manifestation but has more illegible profile. We proposed to consider additional discordant involvement of the bone marrow and a long (at least 6 months) history of the disease as signs of transformation. All the above justifies the use of some of the therapeutic approaches used for the treatment of FL and LMZ for the treatment of patients with c-MYC/BCL2 HGBL DH, c-MYC/BCL6 HGBL DH, and HGBL NOS.
Acknowledgement
Alla Mikhailovna Kovrigina, PhD, head of pathology department in National Research Center for Heamatology, – performing morphological and immunohistochemical diagnostics, providing photographs.
Tatiana Nikiforovna Obukhova, MD, PhD, head of cariology department in National Research Center for Heamatology, – performing cytogenetic diagnostics, providing photographs.
Zakharko Ekaterina Igorevna, head of the flow cytometry group, as part of the central clinical diagnostic laboratory in National Research Center for Heamatology, – performing flow cytometry.
Biderman Bella Veniaminovna, PhD, Senior researcher in laboratory of molecular oncology in laboratory in National Research Center for Heamatology, – performing molecular diagnostics.
Conflict of Interest
The authors declare no conflict of interest.
References
- Swerdlow S H, Elias Campo, Stefano A Pileri, Nancy Lee Harris, Harald Stein, et al. (2016) The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 127(20): 2375-2390.
- Chapuy B, Chip Stewart, Andrew J Dunford, Jaegil Kim, Atanas Kamburov, et al. (2018) Molecular subtypes of diffuse large B cell lymphoma are associated with distinct pathogenic mechanisms and outcomes. Nat Med 24(5): 679-690.
- Lacy S E, Sharon L Barrans, Philip A Beer, Daniel Painter, Alexandra G. Smith, et al. (2020) Targeted sequencing in DLBCL, molecular subtypes, and outcomes: a Haematological Malignancy Research Network report. Blood 135(20): 1759-1771.
- Schmitz R, George W Wright, Da Wei Huang, Calvin A Johnson, James D Phelan, et al. (2018) Genetics and Pathogenesis of Diffuse Large B-Cell Lymphoma. N Engl J Med 378(15): 1396-1407.
- Wright G W, Da Wei Huang, James D Phelan, Zana A Coulibaly, Sandrine Roulland, et al. (2020) A Probabilistic Classification Tool for Genetic Subtypes of Diffuse Large B Cell Lymphoma with Therapeutic Implications. Cancer Cell 37(4): 551-568.
- Flossbach L, Elias Antoneag, Michaela Buck, Reiner Siebert, Torsten Mattfeldt, et al. (2011) BCL6 gene rearrangement and protein expression are associated with large cell presentation of extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. Int J Cancer 129(1): 70-77.
- Ye H, Ellen D Remstein, Chris M Bacon, Andrew G Nicholson, Ahmet Dogan, et al. (2008) Chromosomal translocations involving BCL6 in MALT lymphoma: Haematologica 93(1): 145-146.
- Pillai RK, Malini Sathanoori, Stephen Branden Van Oss, Steven H Swerdlow (2013) Double-hit B-cell lymphomas with BCL6 and MYC translocations are aggressive, frequently extranodal lymphomas distinct from BCL2 double-hit B-cell lymphomas. Am J Surg Pathol 37(3): 323-332.
- Künstner A, Hanno M Witte, Jörg Riedl, Veronica Bernard, Stephanie Stölting, et al. (2021) Mutational landscape of high-grade B-cell lymphoma with MYC-, BCL2 and/or BCL6 rearrangements characterized by whole-exome sequencing. Haematologica.
- Ennishi D, Aixiang Jiang, Merrill Boyle, Brett Collinge, Bruno M Grande, et al. (2019) Double-Hit Gene Expression Signature Defines a Distinct Subgroup of Germinal Center B-Cell-Like Diffuse Large B-Cell Lymphoma. J Clin Oncol 37(3): 190-201.
- Grande B M, Daniela S Gerhard, Aixiang Jiang, Nicholas B Griner, Jeremy S Abramson, et al. (2019) Genome-wide discovery of somatic coding and noncoding mutations in pediatric endemic and sporadic Burkitt lymphoma. Blood American Society of Hematology 133(12): 1313-1324.
- Hilton L K, Jeffrey Tang, Susana Ben-Neriah, Miguel Alcaide, Aixiang Jiang, et al. (2019) The double-hit signature identifies double-hit diffuse large B-cell lymphoma with genetic events cryptic to FISH. Blood 134(18): 1528-1532.
- Sha C, Sharon Barrans, Francesco Cucco, Michael A Bentley, Matthew A Care, et al. (2019) Molecular High-Grade B-Cell Lymphoma: Defining a Poor-Risk Group That Requires Different Approaches to Therapy. J Clin Oncol 37(3): 202-212.
- Cucco F, Sharon Barrans, Chulin Sha, Alexandra Clipson, Simon Crouch, et al. (2020) Distinct genetic changes reveal evolutionary history and heterogeneous molecular grade of DLBCL with MYC/BCL2 double-hit. Leukemia 34(5): 1329-1341.
- Vogelsberg A, Julia Steinhilber, Barbara Mankel, Birgit Federmann, Janine Schmidt, et al. (2021) Genetic evolution of in situ follicular neoplasia to aggressive B-cell lymphoma of germinal center subtype. Haematologica 106(10): 2673-2681.
- Momose S, S Weißbach, J Pischimarov, T Nedeva, E Bach, et al. (2015) The diagnostic gray zone between Burkitt lymphoma and diffuse large B-cell lymphoma is also a gray zone of the mutational spectrum. Leukemia 29(8): 1789-1791.
- Li S, Annapurna Saksena, Parth Desai, Jie Xu, Zhuang Zuo, et al. (2016) Prognostic impact of history of follicular lymphoma, induction regimen and stem cell transplant in patients with MYC/BCL2 double hit lymphoma. Oncotarget Impact Journals 7(25): 38122-38132.
- Rusconi C, Antonella Anastasia, Annalisa Chiarenza, Luigi Marcheselli, Federica Cavallo, et al. (2019) Outcome of transformed follicular lymphoma worsens according to the timing of transformation and to the number of previous therapies. A retrospective multicenter study on behalf of Fondazione Italiana Linfomi (FIL). Br J Haematol 185(4): 713-717.
- Petrich A M, Mitul Gandhi, Borko Jovanovic, Jorge J Castillo, Saurabh Rajguru, et al. (2014) Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: a multicenter retrospective analysis. Blood 124(15): 2354-2361.
- Howlett C, Sonya J Snedecor, Daniel J Landsburg, Jakub Svoboda, Elise A Chong, et al. (2015) Front-line, dose-escalated immunochemotherapy is associated with a significant progression-free survival advantage in patients with double-hit lymphomas: a systematic review and meta-analysis. British Journal of Haematology 170(4): 504-514.
- Misyurina A E, S K Kravchenko, A M Kovrigina, A U Magomedova, L V Plastinina, et al. (2019) The role of translocations involving c-MYC/8q24, BCL2/18q21 and/or BCL6/3q27 genes in patients with follicular lymphoma. Retrospective analysis of single - centre data: 7. Terapevticheskii arkhiv 91(7): 52-62.
- Cheah CY, K E Herbert, K O Rourke, G A Kennedy, A George, et al. (2014) A multicentre retrospective comparison of central nervous system prophylaxis strategies among patients with high-risk diffuse large B-cell lymphoma. Br J Cancer 111(6): 1072-1079.
- Wilson MR, Toby A Eyre, Nicolas Martinez Calle, Matthew Ahearne, Katrina E Parsons, et al. (2020) Timing of high-dose methotrexate CNS prophylaxis in DLBCL: an analysis of toxicity and impact on R-CHOP delivery. Blood Adv 4(15): 3586-3593.
- Nowakowski G S, Fangxin Hong, David W Scott, William R Macon Rebecca L King, et al. (2021) Addition of Lenalidomide to R-CHOP Improves Outcomes in Newly Diagnosed Diffuse Large B-Cell Lymphoma in a Randomized Phase II US Intergroup Study ECOG-ACRIN E1412. J Clin Oncol 39(12): 1329-1338.
- Thieblemont C, Hervé Tilly, Maria Gomes da Silva, Rene-Olivier Casasnovas, Christophe Fruchart, et al. (2017) Lenalidomide Maintenance Compared with Placebo in Responding Elderly Patients With Diffuse Large B-Cell Lymphoma Treated With First-Line Rituximab Plus Cyclophosphamide, Doxorubicin, Vincristine, and Prednisone. J Clin Oncol 35(22): 2473-2481.
- Younes A, Laurie H Sehn, Peter Johnson, Pier Luigi Zinzani, Xiaonan Hong, et al. (2019) Randomized Phase III Trial of Ibrutinib and Rituximab Plus Cyclophosphamide, Doxorubicin, Vincristine, and Prednisone in Non-Germinal Center B-Cell Diffuse Large B-Cell Lymphoma. J Clin Oncol 37(15): 1285-1295.
- Porpaczy E, Philipp Wohlfarth, Oliver Königsbrügge, Werner Rabitsch, Cathrin Skrabs, et al. (2021) Influence of TP53 Mutation on Survival of Diffuse Large B-Cell Lymphoma in the CAR T-Cell Era. Cancers (Basel) 13(22): 5592.
- Zhang M C, Ying Fang, Li Wang, Shu Cheng, Di Fu, et al. (2020) Clinical efficacy and molecular biomarkers in a phase II study of tucidinostat plus R-CHOP in elderly patients with newly diagnosed diffuse large B-cell lymphoma. Clin Epigenetics 12(1): 160.

 Research Article
Research Article