ABSTRACT
Abbreviations: LVEF: Left Ventricular Ejection Fraction; HFpEF: Heart Failure with Preserved Ejection Fraction; eGFR: estimated Glomerular Filtration Rate; Hb: Hemoglobin; BNP: Brain Natriuretic Peptide; SV: Stroke volume; BMI: Body Mass Index; eGFR: Estimated glomerular filtration rate; MNA-SF: Mini Nutritional Assessment- Short Form. SIDE: The Standing test for Imbalance and Disequilibrium; CFS: Clinical Frailty Scale; NYHA: New York Heart Association; NYHA: New York Heart Association
Introduction
The number of patients with heart failure increases year by year with the aging of the population [1], and the frequency of physical therapy for maintaining daily activities (ADL) from the acute stage is increasing. It is known that the prevalence of heart failure increases with age [2]. In Japan, a super-aging society, there is an urgent need to prepare for a “heart failure pandemic” in which heart failure patients are increasing. In addition, heart failure patients have a very poor prognosis, with 3-year survival rates of 15-24% for chronic heart failure [3] and 5-13% mortality in 30 days for acute heart failure [4-6]. Heart failure has traditionally been thought to be mainly in patients with reduced Left Ventricular Ejection Fraction (LVEF). However, in recent years, it has become clear that heart failure patients with LVEF account for about 30- 50% [7], and heart failure with reduced ejection fraction (HFrEF) at JCS 2017 / JHFS 2017. Heart failure with preserved Ejection Fraction (HFpEF) was defined [8]. HFpEF is characterized by a higher proportion of elderly, female, atrial fibrillation, and chronic obstructive pulmonary disease than HFrEF [9]. Furthermore, in daily life, patients suffering from heart failure are said to suffer from exercise intolerance and thus have a reduced quality of life [10]. There are many previous studies suggesting various characteristics of each of HFpEF and HFrEF. However, HFpEF has not established treatment guidelines like HFrEF. HFrEF is caused by lesions of myocardial injury, whereas HFpEF is caused by lesions of vascular endothelial injury caused by increased inflammation and oxidative stress such as obesity, hypertension, diabetes mellitus, and atrial fibrillation [11].
Furthermore, in Japanese society with declining birthrate and aging, an increase in HFpEF patients is predicted even in heart failure. Therefore, it is necessary to distinguish between HFpEF and HFrEF, although they are classified as the same heart failure. Patients with acute heart failure need to regain mobility by early ambulation under risk management. Walking ability is a fundamental movement in everyday life. Also, in clinical practice, self-care independence is often a condition of discharge from home as Needs of a family. Walking independence is an indispensable condition for independence of self-care. Physical therapy for patients with heart failure in acute care hospitals aims to maintain ADL function before admission. Therefore, the biggest issue is how to prevent the disuse syndrome associated with hospitalization. In addition, shortening the number of hospital stays is indispensable because the Japanese government’s medical cost optimization policy aims to shorten the number of hospital stays. Therefore, elucidating the risk factors for decreased walking ability will lead to efficient exercise therapy and support for early discharge from the time of admission, which will help shorten the length of hospital stay. There have been reports of factors related to ADL in elderly patients with heart failure who do not distinguish between HFpEF and HFrEF, such as skeletal muscle weakness and dementia [12,13]. However, no previous studies have identified risk factors for functional decline in HFpEF patients alone. In addition, the number of late-stage elderly HFpEF patients is expected to continue to increase. Therefore, it is considered that the examination of factors related to the decrease in walking ability from the time of admission to the time of discharge from HFpEF patients is extremely clinically significant. Therefore, the purpose of this study was to investigate the risk factors of decreased walking ability from the time of admission to the time of discharge from elderly patients with late-stage acute HFpEF who maintained their walking ability before admission.
Materials and Methods
Research Design and Participants
This has been a retrospective cohort study. We have used data on patients admitted to a secondary emergency care hospital with 500 beds. Subjects included patients who were admitted to our hospital from February 2016 to March 2019 and whose physician was diagnosed with “heart failure”. The following patients were excluded: (Patients under 75 years old, died patients, patients with BI gait less than 10 points before hospitalization, patients with difficult evaluation.) One hospitalization was defined as one patient. Participants in this study were at least 75 years of age at admission and had a pre-hospital Barthel Index mobility score of at least 10 and a LVEF of at least 50% among patients diagnosed with heart failure who were prescribed physical therapy Patients. This study has been reviewed by our ethics committee. (Clinical study number: 2019-902) In addition, the study was disclosed in paper and electronic form, allowing individual patients to withdraw consent to use the data at any time.
Data Collection
We have extracted the following information from the electronic medical record information. (Age, Gender, Estimated glomerular filtration rate (eGFR), hemoglobin (Hb), brain natriuretic peptide (BNP), Stroke volume (SV), LVEF, E / E ‘, NYHA (New York Heart Association: NYHA) severity classification at admission, period from admission to start of physical therapy, hospitalization Days and physical therapy period). We have calculated the eGFR value using the age at admission and the creatinine level at admission, using the formula of Matsuo, et al. [14]. We have extracted the pre-hospital ADL (BI) from electronic medical record information or interviewed patients and their families. In addition, we have performed the following physical therapy assessments: Grip strength for muscle strength assessment, The Standing Test for Imbalance and Disequilibrium [15] (SIDE) for balance assessment, Mini Nutritional Assessment-Short Form (MNA-SF) [16] for nutritional status, Clinical Frailty Scale(CFS) [17] for the amount of activity before hospitalization and dementia were evaluated by Mini-Cog. 18) Mini-Cog is an assessment of dementia [18] that has the same validity as MMSE [19]. SIDE for balance evaluation is a balance evaluation [15] that has a strong correlation with the Berg Balance Scale (BBS) [20]. We have evaluated physical therapy assessment within 3 days from the start of physical therapy. In addition, six physical therapists evaluated physical therapy.
Statistical Analysis
We have used IBM SPSS ver.21 (IBM Japan, Ltd.) for statistical analysis. First, we have defined the group that decreased from the time of admission to the time of discharge in the BI movement items as the “walking function reduced group”, and the others as the “walking function maintenance group”. In these two groups, we have performed a Mann-Whitney U test and an X² test for the following items (Age, Gender, BMI, Hb, eGFR, BNP, SV, EF, E / E ‘, Days to start therapy, hospital stay, Duration of physical therapy, Dementia, CFS, SIDE, grip strength, NYHA).Next, in order to clarify the risk factors for decreased walking ability from the time of admission to the time of discharge from the hospital, we performed a univariate analysis of the “gait function reduction group ‘’ and “gait function maintenance group ‘’ as dependent variables and a comparison between the two groups. Multiple logistic regression analysis was performed using the variable increase method based on the likelihood ratio, using the items with significant differences (P <0.05) and the adjustment factors as independent factors. We have adjusted for age, Gender, and BMI. We have examined odds ratios and 95% confidence intervals, and the fit of the regression analysis was determined by the Hosmer and Lemeshow test. In addition, we have considered the problem of multicollinearity when performing logistic regression analysis. The statistical significance level was 5%. (P <0.05)
Results
Participants Characteristics
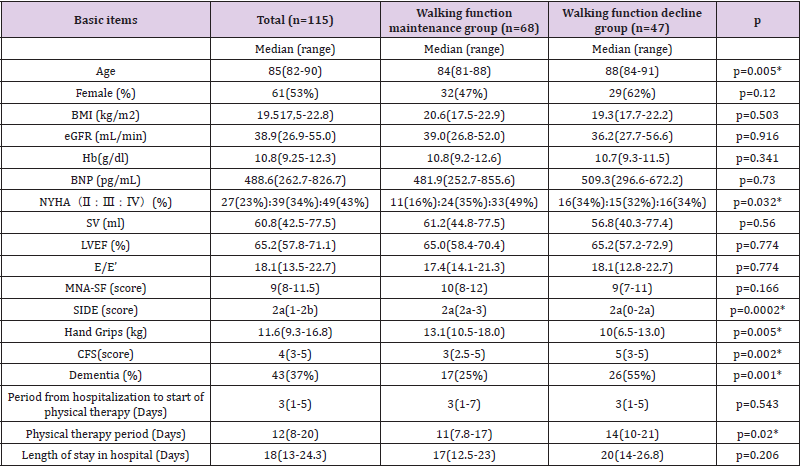
We have identified 115 patients who were 75 years old or older at the time of admission, had a Barthel Index (BI) score of 10 or more before hospitalization, and had an LVEF of 50% or more. The median age in this study was 85 (82-90) years, with 61 women (53%). BMI19.5 (in kg / m (2)) (17,5-22.8), eGFR 38.9 mL / min (26.9-55.0), Hb10.8 g / dl (9.25-12.3), BNP488. 6 pg / mL (262.7- 826.7), NYHA, StageⅡ27 (23%): StageⅢ: 39 (34%), StageⅣ: 49 (43%), SV60.8 (42.5-77.5) mL, LVEF65. 2% (57.8-71.1), E / E’18.1 (13.5-22.7), MNA-SF 9 points (8-11.5), SIDE2a (1-2b), grip strength 11.6 kg (9.3-16.8), CFS 4 points (3- 5), the number of people with dementia (%) 43 (37%), the period from hospitalization to the start of physical therapy 3 days (1-5), physical therapy period 12 (8-20) days, hospital stay 18 (13-24.3) days (Table 1).
Comparison of two Heart Failure Groups
As a result of comparison between the two groups of elderly HFpEF patients, significant differences were found in age, CFS, dementia, Hand grips, SIDE, duration of physical therapy, and NYHA. On the other hand, there were no significant differences in gender, BMI, period from hospitalization to physical therapy, MNASF, eGFR, length of stay, SV, EF, E / E ‘, and BNP.
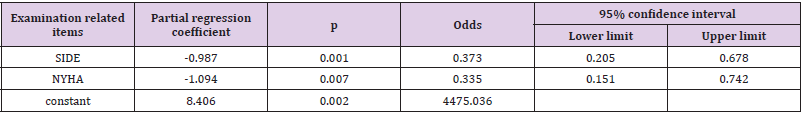
Multiple Logistic Regression Analysis
Multiple logistic regression analysis has extracted SIDE and NYHA in late elderly HFpEF patients related to walking ability. The OR of SIDE has been 0.373 (95% CI, 0.205-0.678, p = 0.001), and the OR of NYHA was 0.335 (95% CI, 0.151-0.742, p = 0.007) (Table 2).
Table 2: Results of multiple logistic regression analysis.
Note: Adjustment factor: Age, Gender, BMI
Discussion
In this study, we have performed a comparison between the groups with maintenance of walking ability and those with reduced gait function to examine risk factors for decreased mobility in elderly patients with HFpEF in the acute phase. The results have shown significant differences in Age, CFS, Dementia, Grip strength, SIDE, Duration of physical therapy, and NYHA. On the other hand, there were no significant differences in Gender, BMI, Period from hospitalization to physical therapy, MNA-SF, eGFR, length of stay, SV, EF, E / E ‘, and BNP. First, we have considered the items for which a significant difference was found between the two groups. Age is defined as sarcopenia, as aging itself causes muscle weakness and muscle weakness, which causes a decrease in walking ability. The cause of sarcopenia is not only aging but also a decrease in physical activity [21]. This time, the subjects were the elderly people aged 75 years or older. The median of each control group was very old, 84 (81-88) years in the maintenance group and 88 (84-91) years in the decline group. Previous studies reported that 38% of patients aged 80-84 and 50% of patients aged 85-89 reported that ADL was reduced by hospitalization [22].
Unlike orthopedic and central nervous system diseases, patients with acute internal illness do not have local weakness or paralysis. Especially in the case of the late- elderly, the reserve function of physical function is low, and the whole-body function is apt to decline due to the bed resting to reduce the cardiac load. In addition, the age group in this study is higher. and older than the age group in previous studies [23]. Compared to HFrEF, HFpEF is said to be characterized by a higher proportion of elderly, female, atrial fibrillation and chronic obstructive pulmonary disease[9]. In this study, HFpEF, and in the case of previous studies, both HFpEF and HFrEF were considered, so it is considered that this study became older. In addition, in this study, it is assumed that there is a difference in the age group from the previous study because the indoor movement was supposed and the study was conducted using the BI mobility items. Dementia has been reported to affect functional independence in patients with heart failure [24]. In addition, previous studies have pointed out the possibility of independent walking when dementia is suspected but not severe [25]. In this study, Mini-Cog was used to determine the presence or absence of dementia, but not the severity. However, patients who did not receive the instruction were regarded as severe cases and used as exclusion criteria. We have targeted patients who could be evaluated even with dementia. Patients with dementia can understand simple instructions, but difficult to understand detailed instructions, and it is highly likely that treatment cannot be performed efficiently. It seems that physical therapy was not able to be carried out efficiently, and the opportunity to improve function was lost, and it was impossible to recover.
CFS shows the amount of physical activity before hospitalization in this study. Frailty is defined as a condition in which vulnerability to health disorders increases due to various functional changes and a decrease in reserve capacity with aging [26]. It is said to cause a decrease in muscle strength, a decrease in maximal oxygen uptake, and the like [27]. Fraily has a profound effect on the prognosis and readmission of heart failure [28]. In this study, the state of the patient two weeks before hospitalization was examined from medical records. In the present study, the median of the maintenance group with CFS was 3 points of “habitual walking”, and the median of the decline group was 5 points of “slow movement and need for advanced IADL support”. Was. Pre-hospital ADL has been reported to decrease in patients with poor ADL prognosis. In this study, it was considered that high physical activity before hospitalization affected ADL at discharge even if the HFpEF patients were classified as late-stage elderly patients with heart failure.
Hand Grips is an index of overall muscle strength and is said to correlate with lower limb strength related to walking ability [29]. In patients with heart disease, the higher the lower limb muscle strength, the lower the incidence of events such as acute exacerbations [30]. In the acute phase of HFpEF patients, skeletal muscle dysfunction is said to occur with the occurrence of a resting bed period to reduce cardiac load [8]. There are many reports of the relationship between walking speed and walking efficiency. Furthermore, walking speed has been a factor in ADL independence in elderly patients with heart failure [31]. In elderly HFpEF patients, it is considered that muscle weakness was caused such that it became difficult to walk about 45 m during the resting bed due to low physical function reserve. It was suggested that HFpEF patients who maintained their general muscle strength at admission could maintain their gait function. There were no significant differences in the echocardiographic SV or E / E ‘. Previous studies have reported that SV and E / E ‘have no correlation with ADL [31]. In this study, although it was a walking item of BI unlike previous research, it was a study focusing on walking ability, which is the basic movement of ADL, so it seems that the same result as the previous research was shown. We have examined the possibility of walking a short distance of 45 m in this study. Therefore, we believe that the results of this study show that the 45-m walking ability of late-stage elderly HFpEF patients is more related to factors such as balance ability and muscle strength than to the factors of whole-body durability.
Next, we have considered the results of logistic regression analysis. NYHA is a severity classification based on subjective symptoms of physical activity ability in daily life [32]. NYHA has been reported as an independent factor in the outcome of patients with HFpEF [33]. Patients with HFpEF have difficulties in prolonged bedtime and appropriate physical exercise physiotherapy due to strong subjective symptoms, and elderly patients with HFpEF have poor walking ability due to poor physical function reserve. It is considered that it was extracted as a factor. SIDE is a balance evaluation of the static balance and shows a strong correlation with BBS [13]. The balance function affects walking ability. When the balance ability decreases, the walking opportunity decreases, and the walking ability decreases. A decrease in walking ability leads to a spiral of a vicious cycle that causes muscle weakness, etc., and further reduces balance ability. Therefore, it is considered that it was extracted as a decrease factor of walking ability. This study has the following limitations. In this study, we found that ADL before admission was difficult to evaluate directly because of retrospective extraction. And the number of participants was small. Furthermore, it was a study of a single facility, and there was a possibility of locality bias.
Conclusion
The purpose of this study was to examine the risk factors of decreased walking ability from the time of admission to the time of discharge from late elderly HFpEF patients admitted to an acute care hospital where walking ability was maintained before admission. The results showed significant differences in age, presence or absence of dementia, CFS, NYHA, duration of physical therapy, SIDE, and grip strength. We extracted two factors from the multiple logistic regression analysis: SIDE for balance assessment and NYHA for severity based on subjective symptoms. It is suggested that it may be necessary to consider a walking ability improvement program that considers subjective symptoms and balance ability when intervening in elderly HFpEF patients. In the future, it will be necessary to reconsider by adding the number of subjects and conducting multi-institutional joint research.
Conflicts of Interest
There are no conflicts of interest to disclose in this study.
Acknowledgment
I would like to thank the proofreading company I was indebted to and the people who looked at the support that I could not describe as a co-star in this publication.
References
- Okura Y, Ramadan MM, Ohno Y, Mitsuma W, Tanaka K, et al. (2008) Impending epidemic future projection of heart failure in Japan to the year 2055. Circ J 72(3): 489-491.
- E Braunwald (2015) The war against heart failure: the Lancet. lecture Lancet 385: 812-824.
- Ushigome R, Sakata Y, Nochioka K, Miyata S, Miura M, et al. (2015) CHART-2 Investigators : Temporal Trends in Clinical Characteristics, Management and Prognosis of Patients With Symptomatic Heart Failure in Japan. Report From the CHART Studies. Circulation Journal 79(11): 2396-2407.
- Cleland JG, Chiswell K, Teerlink JR, Stevens S, Fiuzat M, et al. (2014) Predictors of post discharge outcomes from information acquired shortly after admission for acute heart failure. Circ Heart Fail 7(1): 76-87.
- Cohen Solal A, Logeart D, Huang B, Cai D, Nieminen MS, et al. (2009) Lowered B-type natriuretic peptide in response to levosimendan or dobutamine treatment is asociated with improved survival in patients with severe acutely decompensated heart failure. J Am Coll Cardiol 53(25): 2343-2348.
- O Connor CM, Hasselblad V, Mehta RH, Tasissa G, Califf RM, et al. (2010) Triage after hospitalization with advanced heart failure: the ESCAPE risk method and discharge score. J Am Coll Cardiol 55(9): 872-878.
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, et al. (2013) American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines 2013 ACCF/AHA Guideline for the Management of Heart Failure A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62(16): e147-e239.
- Tsutsui H, Isobe M, Ito H, Okumura K, Ono M, et al. (2018) Guidelines for Diagnosis and Treatment of Acute and Chronic Heart Failure. pp. 10-15.
- Bhatia RS, Tu JV, Lee DS, Austin PC, Fang J, et al. (2006) Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med 355(3): 260-269.
- Upadhya B, Haykowsky MJ, Eggebeen J, Kitzman DW (2015) Exercise intolerance in heart failure with preserved ejection fraction: more than a heart problem. J Geriatr Cardiol 12: 294-304.
- Okumura T, Murohara T (2018) Heart failure in the elderly focused on the heart failure with preserved ejection fraction. Japanese journal of geriatrics 55: 34-40.
- Dumitru L, Iliescu A, Dinu H, Badea R, Savulescu S, et al. (2013) Disability in COPD and Chronic Heart Failure is the skeletal muscle the final common pathway? Maedica 8(2): 206-213.
- Zuccalà G, Onder G, Pedone C, Cocchi A, Carosella L, et al. (2001) Cognitive dysfunction as a major determinant of disability in patients with heart failure: results from a multicenter survey. J Neurol Neurosurg Psychiatry 70(1): 109-112.
- Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, et al. (2009) Collaborators developing the Japanese equation for estimated GFR. :Revised equations for estimated GFR from serum crainine in Japan. Am J Kidney Dis 53: 982-992.
- Kondo I, Hosokawa K, Iwata M (2004) Development and interrater reliability of standing test for imbalance and disequilibrium (SIDE). Jpn J Rehabil Med 41: 483.
- Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, et al. (2009) Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging 13(9): 782-788.
- Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, et al. (2013) Frailty consensus:A call to action. J Am Med Dir Assor 14(6): 392-397.
- Borson S, Scanlan JM, Chen P, Ganguli M (2003) The Mini-Cog as a Screen for Dementia: Validation in a Population-Based Sample. J Am Geriatr Soc 51(10): 1451-1454.
- Soo Borson, James Scanlan, Michael Brush, Peter Vitaliano, Ahmed Dokmak (2000) The Mini-Cog:aA cognitive vital signs measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry 15(11): 101-1027.
- Teranishi T, Kondo I, Sonoda S, Kagaya H, Wada Y, et al. (2010) A discriminative measure for static postural control ability to prevent in-hospital falls: Reliability and validity of the Standing Test for Imbalance and Disequilibrium (SIDE). Jpn J Compr Rehabil Sci 1: 11-16.
- Cruz Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, et al. (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39(4): 412-423.
- Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, et al. (2003) Loss of independence in activities of daily living in older adults hospitalized with medical illness:increased vulnerability with age. J Am Geriatr Soc 51(4): 451-458.
- Yaku H, Ozasa N, Morimoto T, Inuzuka Y, Tamaki Y, et al. (2018) KCHF Study Investigators. :Demographics, Management, and In-Hospital Outcome of Hospitalized Acute Heart Failure Syndrome Patients in Contemporary Real Clinical Practice in Japan. Observations From the Prospective, Multicenter Kyoto Congestive Heart Failure (KCHF) Registry Circ J 82(11): 2811-2819.
- Alosco ML, Spitznagel MB, Sweet LH, Josephson R, Hughes J, et al. (2015) Cognitive Dysfunction Mediates the Effects of Poor Physical Fitness on Decreased Functional Independence in Heart Failure. Geriatr Gerontol Int 15(2): 174-181.
- Arai T, Kaneko S, Fujita H (2011) Decision trees on gait independence in patients with femoral neck fracture. Japanese Journal of Geriatrics 48(5): 539-544.
- Qian Li Xue (2011) The Frailty Syndrome: Definition and Natural History. Clin Geriatr Med 27(1): 1-15.
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, et al. (2001) Cardiovascular Health Study Collaborative Research Group.: Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56(3) : M146-56.
- Vidán MT, Blaya Novakova V, Sánchez E, Ortiz J, Serra Rexach JA, et al. (2016) Prevalence and prognostic impact of frailty and its components in non-dependent elderly patients with heart failure. Eur J Heart Fail 18(7): 869-875.
- Fragala MS, Alley DE, Shardell MD, Harris TB, McLean RR, et al. (2016) Comparison of Handgrip and Leg Extension Strength in Predicting Slow Gait Speed in Older Adults. J Am Geriatr Soc 64(1): 144-150.
- Kamiya K, Masuda T, Tanaka S, Hamazaki N, Matsue Y, et al. (2015) Quadriceps Strength as a Predictor of Mortality in Coronary Artery Disease. Am J Med 128(11): 1212-1219.
- Watanabe S, Morio H, Izawa K, Nagata N, Omiya K, et al. (2016) About an exertion function to distinguish the independence of the everyday life activity in patients with old cardiovascular disease. Journal of Japanese Association of Cardiac Rehabilitation 2(3): 163-168.
- (1994) The criteria committee of the New York Heart Association. In: Nomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels. (9th)., Little Brown & Co, USA, pp. 253-256.
- Dalos D, Mascherbauer J, Zotter Tufaro C, Duca F, Kammerlander AA, et al. (2016) Functional status, pulmonary artery pressure, and clinical outcomes in heart failure with preserved ejection fraction. J Am Coll Cardiol 68(2): 189-199.

 Research Article
Research Article