SUMMARY
Purpose of the Study: To study the relationship between the renal perfusion index and systolic heart function in type 4 cardiorenal syndrome in patients with type 2 diabetes mellitus.
Material and Research Methods: The study, which was performed from January to May 2022, included 48 patients with type 2 diabetes mellitus and stage 1-3 CKD. (16 F, 32 M, age 50±17 years, BMI 27.02±3.44 kg/m2.) according to the study protocol. Hypertensive nephropathy (HT-CKD) addressed 12 patients. None of the patients included in the study had heart failure. The control group consisted of 20 patients with DM2 without CHF and without CKD. The study used clinical and biochemical research methods (glycemia, glycated hemoglobin, IRI, C-peptide, ALT, AST, bilirubin, urea, creatinine, PTI, hormonal studies (renin, angiotensin, aldosterone) as well as instrumental methods of examination - ultrasound internal organs, ultrasonography with an assessment of the overall intensity of cortical perfusion of the kidneys and the renal perfusion index (RPI),ECG, Echo-ECG, indicators of the quality of life of patients (questionnaire), as well as statistical methods.
Research Results: Analyzing the data of dopplerography of the heart and kidneys, we present for the first time the effect of systolic heart function on RI in patients with type 2 diabetes with CKD. This allows with the probability of early non-invasive detection of cardiac systolic pathology during ultrasound of the kidneys, when highquality ultrasound examination of the structures of the heart is impossible (lack of technique, emphysema, obesity). Finally, it is likely that RI assessment may be useful for early detection of CRS associated with reduced cardiac output. However, the applicability of RI for diagnosing early anomalies of the cardio-renal axis requires further study.
Conclusion:
i. In the group of patients with DM 2 and CKD stages 1-3 without CHF, we detected Echo-ECG changes according to the type of LV diastolic dysfunction of 1-2 degrees with a tendency to increase the mean pressure in the pulmonary artery.
ii. RI can be used as an independent marker for predicting the outcomes of CKD in type 2 DM.
Keywords: Type 2 Diabetes Mellitus; Cardio-Renal Syndrome
Abbreviations: CRS: Cardio-Orenal Syndrome; CKD: Chronic Kidney Disease; CRS: Cardiorenal Syndrome; HT-CKD: Hypertensive Nephropathy
Relevance
Despite the growing number of studies on cardio-orenal syndrome (CRS), pathogenesis is still unclear [1,2]. Suspicion of CRS seems clear in the presence of renal or cardiac involvement with concomitant second organ dysfunction. Diagnostic difficulties arise at the stage preceding the clinical manifestation of the disease, or when the function of only one of the organs is impaired, and the function of the second organ does not arouse suspicion and does not require intervention. At the same time, even small pathological changes at the functional level in one of the organs can cause changes in the functioning of another. According to the authors, renal perfusion disorders are an important link in the pathogenesis of cattle [1,3]. It is known that preserved renal perfusion determines the appropriate oxygenation of organ tissues [2]. Both a decrease and an increase in renal perfusion lead to a decrease in tissue oxygenation and the onset of fibrosis. It has been established that left ventricular heart failure leads to a decrease in renal perfusion and the launch of compensatory mechanisms that improve cardiac output to restore normal organ perfusion [3-5]. According to a multi-country study (USA, Hungary, Italy) published in 2018, CKD may exacerbate the progression of chronic heart failure, leading to the development of type 4 CRS (T4CRS) [6-8].
The existence of a relationship between the heart and the kidney was first described in the 19th century by Robert Bright, who reported structural changes in the heart in patients with advanced disease kidneys [Bright R., 1836]. Since then, new discoveries have provided insight into the interaction between heart and kidney disease in terms of common risk factors (such as hypertension, obesity, diabetes, and atherosclerosis) and the pathophysiological pathways involved in each [Zannad F, Cabandugama PK, Banerjee S]. Clinically, general pathology of the heart and kidneys has a strong impact on clinical outcome and is associated with increased morbidity and mortality rates [McCullough PA, Raina R] The classic definition of cardiorenal syndrome (CRS) was proposed in 2010 by the Acute Dialysis Quality Initiative as a term that combines “diseases of the heart and kidneys in which acute or chronic dysfunction of one organ can cause acute or chronic dysfunction of another” [Ronco C]. In recent years, understanding of the clinical impact of interactions between the heart and kidneys has increased significantly. This work is evidenced by 142 articles in Pubmed related to the term “cardiorenal syndrome” (CRS) over the past 5 years. Dysfunction (structural or functional) in one organ causes dysfunction in another organ, which ultimately has been shown to increase morbidity and mortality. There has been a paradigm shift in the approach to diagnosis and treatment of this complex disorder. Currently, cardiovascular disease, type 2 diabetes and chronic kidney disease (CKD) are already considered as a single cardio-reno-metabolic syndrome, or continuum. It has been shown that the relationship between these diseases is permanent with common risk factors and progression mechanisms (Kobalava Zh). All of the above emphasizes the relevance of this study [7].
Purpose of the Study
To study the relationship between the index of renal perfusion and systolic function of the heart in cardio-renal syndrome in patients with type 2 diabetes mellitus.
Material and Research Methods
The study included 48 patients with type 2 diabetes mellitus and stage 1–3 CKD. (16 F, 32 M, age 50±17 years, BMI 27.02±3.44 kg/m2.) according to the study protocol. Hypertensive nephropathy (HT-CKD) addressed 12 patients. None of the patients included in the study had clinically diagnosed heart failure. The control group consisted of 20 patients with DM2 without CHF and without CKD. The study used clinical and biochemical research methods (glycemia, glycated hemoglobin, IRI, C-peptide, ALT, AST, bilirubin, urea, creatinine, PTI, hormonal studies (renin, angiotensin, aldosterone) as well as instrumental methods of examination - ultrasound internal organs, ultrasonography with an assessment of the overall intensity of cortical perfusion of the kidneys and the renal perfusion index (RPI),ECG, Echo-ECG, indicators of the quality of life of patients (questionnaire), as well as statistical methods. For kidney ultrasound, an Aloka ultrasound machine with a 4L convex probe (2-5MHz) was used. The renal resistive index in segmental arteries was assessed as described previously. The average value of RI was calculated from 2-3 measurements in the upper, middle and lower sections of the renal sinus. Renal perfusion was assessed using the DTPM method. Used for echocardiography Vivid e9 or Vivid I (General Electric, Fairfield, CT) with M4S-RS transducer (1.5-3.6 MHz). All measurements in M-mode were performed in accordance with the recommendations of the American Society of Echocardiography. Statistical calculations were carried out in the Microsoft software environment Windows using the software packages Microsoft Excel-2007 and Statistica version 6.0, 2003. The obtained data are reflected in the dissertation as M±m, where M is the mean value of the variation series, m is the standard error of the mean. The significance of differences between independent samples was determined by the Mann-Whitney method and
Results and Discussion
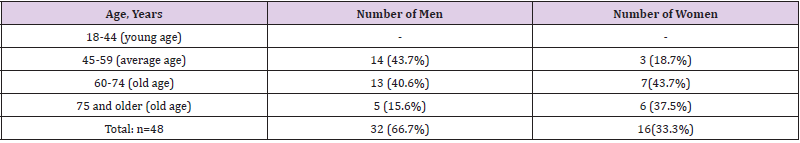
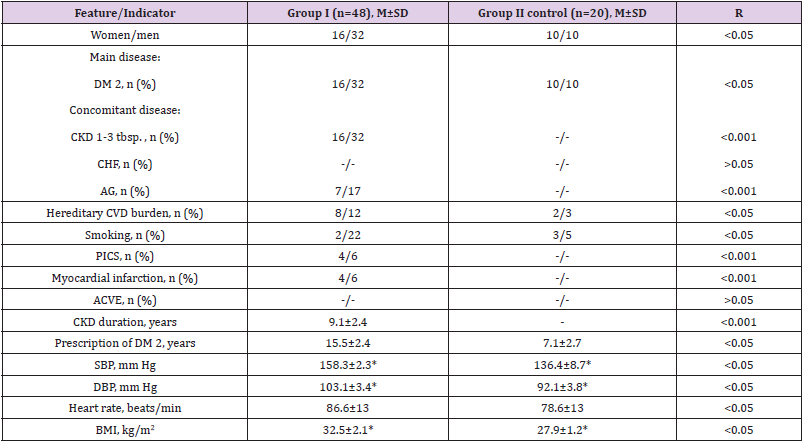
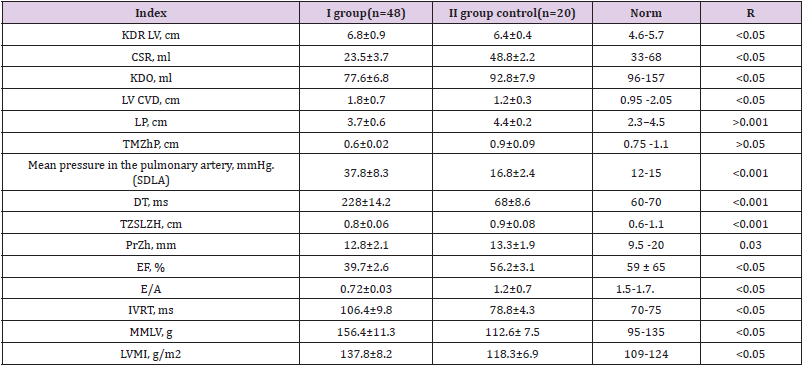
Table 1 shows the distribution of examined patients by sex and age. As can be seen from Table 1, patients in the age group from 60 to 74 years old both among men and women predominated - 23/11 cases, respectively. As can be seen from Table 2, the significance of differences in comparison with the control relative to SBP, DBP, BMI in the studied patients was established (p<0.05). At the same time, 20 (42%) patients out of 48 in the main group had a history of myocardial infarction. In the same group, bad habits (smoking) were more common, the duration of DM 2 prevailed (v<0.05) in comparison with the control group. The next stage of our work was the analysis of Echo-ECG data from our patients (Table 3). As can be seen from Table 3, there is a significant difference in the parameters of the central hemodynamics of the main group compared with the control group: LV EDR, ESV, EDV, LV ESR(p<0.05),mean pressure in the pulmonary artery, the time of slowing the blood flow of early diastolic filling, TZSLV (p<0.001), EF, the ratio of the peak velocities of E and A waves, the time of isovolumic relaxation of the LV, LVMI, LVMI (p<0.05). Thus, in the group of patients with DM 2 with CKD stages 1-3 without CHF, we detected Echo-ECG changes in the type of LV systolic dysfunction of 1-2 degrees with a tendency to increase the mean pressure in the pulmonary artery. It should be noted that LV systolic dysfunction is characterized by an asymptomatic course, as noted in our patients. The patient may note both the presence of characteristic symptoms, and their complete absence. In the latter case, they speak of asymptomatic dysfunction.
Table 2: Clinical and anamnestic characteristics of patients included in the study.
Note: AH: Arterial Hypertension; DBP: Diastolic Blood Pressure; SBP: Systolic Blood Pressure; p: Reliability Criterion
Table 3: Indicators of structural and functional parameters of the heart in patients included in the study (M ± m).
Note: *Differences are significant, p < 0.05. :EDR: End Diastolic Size, ESR: End Systolic Size, LA: Pulmonary Artery, LV: Left Ventricle, LA: Left Atrium, n/a: Unsignificant Difference Between The Compared Parameters, RV: Right Ventricle, SBP: Systolic Blood Pressure, TZSLV: Thickness Posterior Wall of the Left Ventricle, VTRV: Thickness of the Interventricular Septum, EF: Ejection Fraction, CHF: Chronic Heart Failure, HR: Heart Rate, DT: Early Diastolic Filling Blood Flow Deceleration Time, IVRT: LV Isovolumic Relaxation Time, E/A: Peak Ratio Wave Velocities E and A., EDV - End Diastolic Volume, ESV - End Systolic Volume, LVMM - LV Myocardial Mass, LVMI - LVMI Index
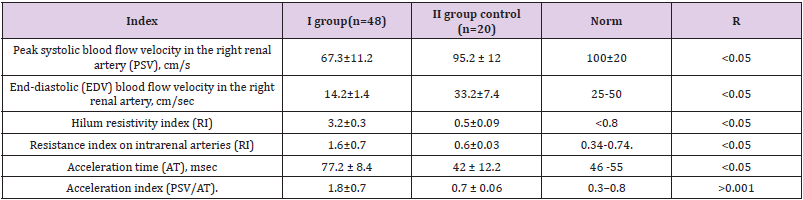
Our patients of the main group had changes in Dopplerography of the kidneys, shown in Table 4. As can be seen from Table 4, the indicators of the main group significantly differed from the control group (p<0.05). In this group, a decrease in peak systolic and end-diastolic blood flow velocity in the right renal artery, an increase in RI in the renal hilum and intrarenal arteries were found. It is known that most common cause of heart failure (HF) is systolic dysfunction of LV. Any pathological process, which affects LV systolic function or leads to an increase in its mass, can also change LV diastolic function. In every third patient with symptoms of congestive heart failure, myocardial contractility is not impaired, and the cause of the development of cardiac symptoms lies in the violation of the LV blood filling, i.e., its diastolic dysfunction. Changes in LV diastolic filling appear in most heart diseases earlier than impaired systolic function LV. All the above data indicate the need for timely diagnosis of CRS in patients with DM 2, the development of measures to prevent their development and the organization of long-term monitoring of patients with a high risk of developing this complication of diabetes.
Conclusion
1) In the group of patients with DM 2 and CKD stages 1-3 without CHF, we detected Echo-ECG changes according to the type of LV diastolic dysfunction of 1-2 degrees with a tendency to increase the mean pressure in the pulmonary artery.
2) RI can be used as an independent marker for predicting the outcomes of CKD in DM.
References
- McCullough PA, Kellum JA, Haase M, Christian Müller, Kevin Damman, et al. (2013) Pathophysiology of the cardiorenal syndromes: executive summary from the eleventh consensus conference of the Acute Dialysis Quality Initiative (ADQI). Contrib Nephrol 182: 82-98.
- Singh P, Ricksten SE, Bragadottir G, Bengt Redfors, Lina Nordquist (2013) Renal oxygenation and haemodynamics in acute kidney injury and chronic kidney disease. Clin Exp Pharm and Physiology 40(2): 138-147.
- Sinkeler SJ, Damman K, van Veldhuisen DJ, Hans Hillege, Gerjan Navis (2012) A re-appraisal of volume status and renal function impairment in chronic heart failure: combined effects of pre-renal failure and venous congestion on renal function. Heart Failure Rev 17(2): 263-270.
- Tumlin JA, Costanzo MR, Chawla LS, Charles A Herzog, John A Kellum, et al. (2013) Cardiorenal syndrome type 4: insights on clinical presentation and pathophysiology from the eleventh consensus conference of the Acute Dialysis Quality Initiative (ADQI). Contrib Nephrol 182: 158-173.
- Scholbach T, Scholbach J (2009) Can we measure renal tissue perfusion by ultrasound? J Med Ultrasound 17(1): 9-16.
- Lubas A, Kade G, Niemczyk S (2013) Renal resistive index as a marker of vascular damage in cardiovascular diseases. Int Urol Nephrol 46(2): 395-402.
- Marta Sarkozy, Zsuzsanna ZA Kovacs, Monika G Kovacs, Renata Gaspar, Gergő Szűcs, et al. (2018) Mechanisms and Modulation of Oxidative/Nitrative Stress in Type 4 Cardio-Renal Syndrome and Renal Sarcopenia. Physiol 9: 1648.
- Arkadiusz Lubas, Robert Ryczek, Grzegorz Kade, Stanislaw Niemczyk (2015) Renal Perfusion Index Reflects Cardiac Systolic Function in Chronic Cardio-Renal Syndrome. Med Sci Monit 21: 1089-1096.

 Research Article
Research Article