SUMMARY
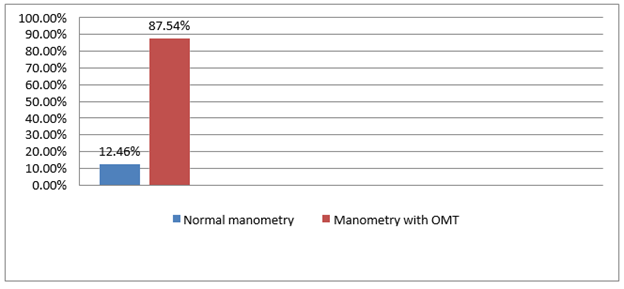
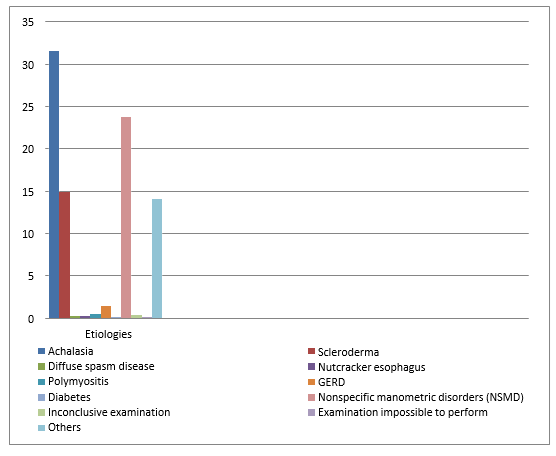
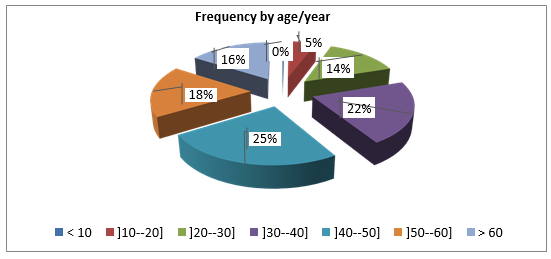
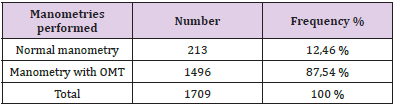
Esophageal manometry is the most appropriate diagnostic test for detecting esophageal motor disorders (OMD). This test makes it possible, in particular, to show incomplete relaxation of the lower esophageal sphincter with a median integrated relaxation pressure ≥ 15 and 100% failure of peristalsis [1]. Our retrospective descriptive study focused on 1709 manometries performed in adult subjects of both sexes, during the last ten years. The manometric data (resting pressure, relaxation percentage, amplitude of the esophageal body, frequencies of the different types of waves) were analyzed. The population concerned by our study is 1496 subjects with a OMD made up of 1123 women or 75.07 % and 373 men or 24.93 % for a total number of manometries performed during this period of 1709; the proportion of OMD in relation to the total number is 87.54%. Our results show that achalasia is the most common cause of OMD. Which affect middle-aged patients much more, between 40 and 50 years old, probably in relation to the resurgence of general diseases during this age group. It appears, in our study, that OMD are more frequent in women compared to men for sex- related considerations.
Abbreviations: OMD: Esophageal Motor Disorders; LES: Lower Esophageal Sphincter; US: Upper Sphincter
Introduction and Objectives
Esophageal manometry is currently the most sensitive method for recording motor events in the esophagus (OMT). The measurement of these events combining contractions and relaxations allows to study swallowing and to specify motor abnormalities at the level of the lower esophageal sphincter (LES), the body and, to a lesser degree, the upper sphincter (US). These motor disorders may be responsible for different symptoms, such as dysphagia and chest pain (DT), or be associated with different pathologies. It is the only method that allows the classification of motor disorders into different nosologic entities [2]. The recording of the different motor phenomena at the level of the LES and the body of the esophagus as well as the interpretation of the tracings require physiological knowledge, specific training and rigorous care in the execution. Several French [3] and Anglo-Saxon [4,5] practice guidelines have been published defining the prerequisites and conditions of the examination. Esophageal manometry is the preferred diagnostic test for the diagnosis of TMO. This test allows, in particular, to show incomplete relaxation of the lower esophageal sphincter with a median integrated relaxation pressure ≥ 15 and 100% failure of peristalsis [1]. Therefore, in this work, we want to highlight the contribution of manometry in the differential diagnosis of TMO.
Patients and Methods
Patients
This is a retrospective descriptive study of 1709 manometries performed in adult subjects of both sexes during the last ten years.
Inclusion Criteria:
1. Subjects aged 20-80 years free of clinical or manometric signs of OMT
2. Non-dysphagic subjects with a manometric trace of OMT
3. Dysphagic subjects (solid or mixed dysphagia) with normal manometric pattern
4. Dysphagic subjects (dysphagia to solids or mixed) with TMO manometric pattern.
Non-Inclusion Criteria:
1. Subjects operated for achalasia
2. Subjects operated on for hiatal hernia or other pathologies of the esogastric tract
3. Subjects presenting an obstacle or anomaly at the level of the nasal septum preventing the passage
4. the passage of the probe by nasogastric way
5. Subjects with a motor handicap who cannot stand the sitting position
6. Subjects with severe hypoglycemia who cannot tolerate 8 hours of fasting
7. Subjects with a chronic cough that hinders the examination and gives a false result manometry.
Methods
Manometric data (resting pressure, percent relaxation, body amplitude, frequencies of different wave types) were collected. The examination was performed using a perfused nasogastric tube including at least 4 catheters and which must be purged; this is the conventional esophageal manometry technique. The manometric examination of the esophagus begins with an intubation which allows the positioning of the probe in the stomach, the patient being in a sitting position). Once the 4 catheters of the probe are in the stomach, the patient is laid down to start the recording of the manometric tracing. The study of the motor phenomena of the esophageal body is based on the analysis of the different characteristics of the contractile waves during wet swallowing (swallowing of a bolus of water): duration, amplitude and propagation of the muscular contractions. Analysis of LES relaxation and esophageal peristalsis allows a positive diagnosis of esophageal motor disorder. The gradual withdrawal method consists of withdrawing the probe in steps of 0.5-1 cm; the recording must be long to have a stable resting pressure. Pressures can be expressed in different units depending on the laboratory: 1 kPa = 10 cm H2O = 7.5mm Hg (Figures 1 & 2).
Figure 3: Our results show that TMO is more common in middle-aged patients, between 40 and 50 years.
The study of the LES must include all the elements necessary to describe its functioning: length, resting pressure and relaxation as well as its duration during swallowing. The measurements should always be performed at the same time, i.e, either at the end of expiration or at mid-expiration. The range of normality varies between laboratories, it is between 12.4- and 34.5-mm Hg. Residual pressure should be <7 mm Hg, percent relaxation >90%, and relaxation time <8 seconds. The analysis of the conventional esophageal manometry reports as well as the patients’ files at the level of the functional exploration unit of the internal medicine department of the EPH Kouba allowed us to collect the data which were analyzed (Figures 3 & 4).
Statistical Analysis
The results were processed using the Statistical Package of Social Sciences (SPSS 4.0).
Result
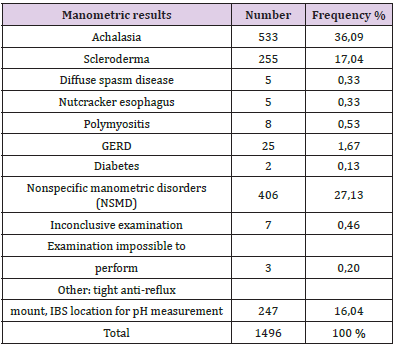
The population concerned by our study is n= 1496 TMO made up of 1123 women or 75.07% and 373 men or 24.93% for a total number of manometries performed during this period of 1709; the proportion of TMOs in relation to the total number is 87.54%, as shown in the following (Tables 1 & 2).
Table 1: Representation of manometries with OMT in relation to the total number of manometries performed.
Table 2: Representation of the different manometric results in relation to the total number of manometries performed.
Discussion
The analysis of the observations noted during our study leads us to clarify the physio pathological aspects. Achalasia has been shown to be the most common cause of OMT; indeed, since the origin of the disease is the degeneration of esophageal parietal neurons affecting NO (nitric oxide) producing inhibitory neurons, there are consequently adverse effects on the relaxation function of esophageal smooth muscle [6]. The fact that TMO affects adult patients much more is probably since this population is more vulnerable to general chronic pathologies. In addition, the predominance of women in esophageal motor disorders could be related to a set of triggering factors linked to gender. The most frequent indication for the diagnosis of achalasia was dysphagia, as described in the literature [7]; our work confirmed this relationship. The most common type of achalasia is classical achalasia because it is only at this stage that the disease is diagnosed since the vigorous form is often ignored or confused with is often unrecognized or confused with the non-specific motor disorders [8].
The most common OIS abnormality in achalasia has been loss of relaxation [9]; this relationship reflects the pathophysiologic mechanisms underlying the loss of esophageal smooth muscle phasic activity in this upper GI pathology. The most common motor disturbances in the esophageal body during achalasia were non- propagating contractions. Thus, it can be said that the most frequent and typical pattern of achalasia is characterized by an absence of relaxation of the LES with the presence of nonpropagated contractions at the level of the esophageal body. The most frequent correlation between indication and manometric tracing was dysphagia with an achalasia tracing; this suggests that dysphagia is the main symptom in achalasia and that its presence is an indication to perform esophageal manometry [10].
Conclusion
Esophageal manometry is a key functional exploration tool of the upper digestive tract. Its usefulness and high performance in the diagnosis of esophageal motor disorders are validated. Achalasia represents the most common motor disorder found by this technique. Esophageal manometry allows, on the one hand, to diagnose achalasia and offers, on the other hand, the opportunity to treat patients presenting an achalasia tracing even at a very early stage of the disease, and, on the other hand, thanks to the control tracings, to undertake the follow-up of the evolution of the patients treated medically or surgically and to establish, consequently, the prognosis of the disease.
References
- (2003) Guide for the use of endoscope washer-disinfectors.
- Frank Zerbib, Michel Dapoigny (2010) Le’s explorations fonctionnelles digestives. Edition Elsevier Masson.
- Kronecker H, Meltzer SJ, Der Schluckmemanismus, seine Erregungund seine Hemmung. Arch Ges Anat Physiol Supp 7(1883): 328- 32.
- Parkman HP, Orr WC (2009) The gastrointestinal motility laboratory. Gastro intestosc Clin N Am 19: 171-84.
- Council Directive 93/42/EEC of 14 June 1993 concerning medical devices. Official Journal N°L169 of 12/07/1993: 1-43.
- Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia. Lancet 383: 83-93.
- Chtouroul, Rejab H, Rachek R, Kallel R, Boudabous M, et al. Diagnostic and therapeutic news of achalasia. J.I. M. Sfax, N°37; Feb 21: 1-93.
- Andolfi C, Fisichella PM (2019) Meta-analysis of clinical outcome after treatment for achalasia based on manometric subtypes. Br J Surg 106(4): 332-341.
- Zebib F, Roman S (2015) Current therapeutic options for esophageal motor disorders as defined by the Chicago classification. J Clin Gastroenterol 49(6): 451-460.
- Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: Diagnosis and management of achalasia. Am J Gastroenterol 108(8): 1238-1249.

 Short Communication
Short Communication