ABSTRACT
Background: Diastasis recti is an increase in the distance between the rectus abdominis muscles in the midline caused by weakness in the anterior abdominal wall. Patients with diastasis recti commonly present with a midline bulge with or without other symptoms. The preaponeurotic endoscopic repair is performed with a suprapubic approach and in both iliac fossae. A new preaponeurotic cavity is created with dissection of the subcutaneous cellular tissue, followed by rectification with barbed suture.
Methodology: A narrative review was carried out through various databases from January 2012 to February 2022; the search and selection of articles was carried out in journals indexed in English. The following keywords were used: Endoscopic repair; preaponeurotic; diastasis recti; physiotherapy.
Results: Diastasis recti is an increase in the distance between the rectus abdominis muscles in the midline caused by weakness in the anterior abdominal wall. Currently there are different therapeutic approaches for diastasis recti, among which we can highlight physiotherapy and surgical approach which can be open surgery, laparoscopic surgery and robot-assisted surgery. The preaponeurotic endoscopic repair allows us to resolve the parietal defect with the placement of a reinforcement supraaponeurotic prosthesis.
Conclusion: His review offers updated and detailed information on the treatment options that exist to date, as well as highlighting the importance of preaponeurotic endoscopic repair
Keywords: Endoscopic Repair; Preaponeurotic; Diastasis Recti; Physiotherapy
Introduction
Rectus diastasis is considered an unusual increase in the space between the rectus abdominis muscles in the midline, this is caused by weakness in the anterior abdominal wall. Most experts consider that there is weakness, thinning and widening of the linea alba and weakness of the abdominal muscles [1,2]. Common complaints are signs and symptoms caused by diastasis recti from patients in various fields, including plastic surgery, emergency medicine, general surgery, gynecology, obstetrics, and family medicine [3,4]. The perception of the lump or other symptoms by the patient are of great importance in diagnosis and treatment. Additionally, several studies have been conducted to identify the normal versus enlarged distance between the rectus muscles [5,6]. Patients with this condition often present with a midline bulge with or without other symptoms [7]. It is important to explain to the patient that there is no true hernia or future risk of complications. But for patients who report discomfort and/or cosmetic concerns, treatments should be offered and discussed [8]. The preaponeurotic endoscopic repair is performed with a suprapubic approach and in both iliac fossae, creating a preaponeurotic cavity with dissection of the subcutaneous cellular tissue, posteriorly, rectification is performed with barbed suture. Reinforcing the wall with polypropylene mesh [9]. Drainage is systematically left. Due to the patient’s complaints and the aesthetic problems that diastasis recti could have, it is convenient to carry out this work in order to show all the treatment options that exist to date as well as to highlight the importance of preaponeurotic endoscopic repair [10,11].
Materials and Methods
A systematic review was carried out. Implemented databases: PubMed, Scielo and ScienceDirect, among others. The selection of articles was carried out in journals indexed in English from the years 2012 to 2022. The DeCS and MeSH methodology was used to identify keywords such as: Endoscopic repair; preaponeurotic; recti diastasis; physiotherapy. We identified 58 original and review publications associated with the theme, 28 articles met the specified inclusion requirements, among which we highlight articles that were in a range not less than the year 2012, full text articles and that reported on endoscopic repair. preaponeurotic for management of diastasis recti. Articles that did not have sufficient information and that did not present the full text at the time of review were taken as exclusion criteria.
Results
Diastasis Recti
Patients with this alteration note a general feeling of instability and/or a bulge in the midline of the anterior abdominal wall, the increase in abdominal pressure worsens the symptoms reported by the patient. Stress urinary incontinence and back pain have been shown to be caused by diastasis recti [12,13]. While diagnostic and treatment options should focus on the patient’s perception of the lump or other symptoms, several studies have been conducted to look at normal versus enlarged distance between the rectus muscles. Most experts consider that a separation of more than two centimeters can be considered abnormal but keeping in mind that there may be less or more with or without bothersome symptoms [14]. Diastasis recti can be confused with a ventral hernia; however, there is no fascial defect in diastasis recti. Diastasis recti is associated with conditions in which there is increased intraabdominal pressure, including pregnancy and obesity, as well as diseases that lead to weak connective tissues [14]. Patients with diastasis recti commonly present with a midline bulge with or without other symptoms. The indication for treatment of diastasis recti is based on the patient’s perspective and complaint [15].
Treatment Options for Diastases of the Rectus Abdominis
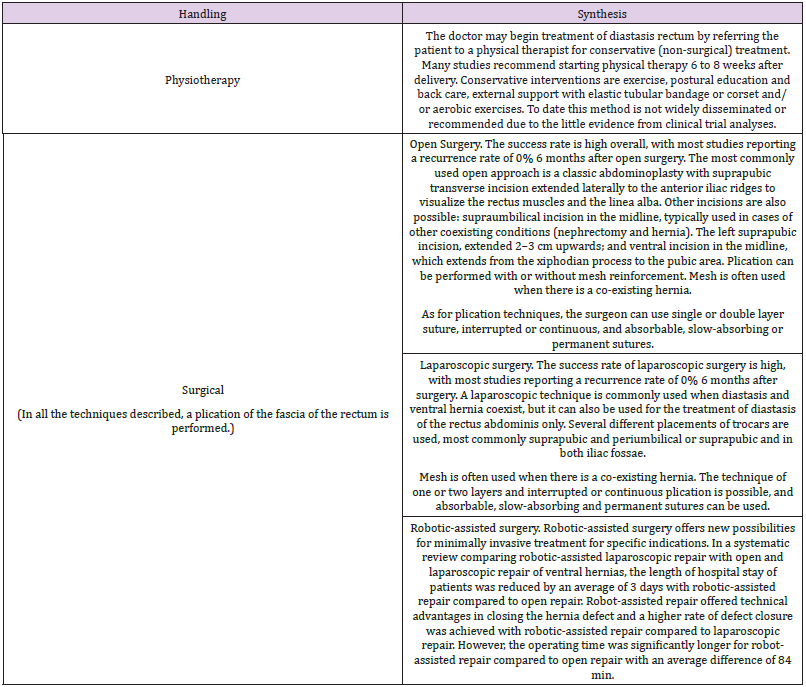
Currently there are different therapeutic approaches for diastases of the rectum, among which we can highlight those found in Table 1 [14-17]. Surgery may be considered when physical therapy fails to reduce abnormal widening of the linea alba and discomfort is severe. We suggest that surgery can be considered 6 to 12 months after delivery, as the diastasis may resolve naturally during this period [18].
Preaponeurotic Endoscopic Repair
A preaponeurotic endoscopic approach allows us to resolve the parietal defect with the placement of a reinforcement supraaponeurotic prosthesis, which will reduce recurrence, increasing plastic safety, without entering the abdominal cavity, with good aesthetic and functional results [19]. Rectus diastasis was associated with midline defects in 100%. The preaponeurotic endoscopic repair is performed with a suprapubic approach and in both iliac fossae. A new preaponeurotic cavity was created with dissection of the subcutaneous cellular tissue and then rectification was performed with barbed suture. The wall is reinforced with polypropylene mesh. Drainage is systematically left [18].
Surgical Technique
Under general anesthesia and endotracheal intubation, the patient is placed in the dorsal position with the legs apart. The surgeon is placed between the legs; the wizard is located to the right or left according to preference [19]. An incision is made in the suprapubic midline; a preaponeurotic space is created; an optical trocar is placed, the neocavity is infused with pressure between 8 and 10 mmHg, then the 5 mm working trocars are placed, they are placed in both iliac pits under direct vision, as shown in Figure 1 [18-23]. Then the dissection of the subcutaneous cell tissue up to 3 cm beyond the bilateral costal margin and laterally to the anterior axillary lines is completed. Plication of the sheath of the rectum with bearded suture is performed from the xiphoid appendix up to 5 cm subumbilical. If necessary, the release of aponeurosis from the external oblique is carried out outside the outer edge of the rectum [24]. Hemostasis control and neocavity washing are performed. Then a light mesh of acroporous polypropylene 22 cm long × 15 cm transverse is placed or placed of the appropriate size to cover the area of detachment of the external oblique if it was performed [25]. The prosthesis is fixed with trackers, straps or resorbable stitches. The navel is reinserted with internal or external sutures. Aspirational drains were placed systemically in 100% of cases, with a permanence of approximately 3 days. Removing when the remnant was less than 50 cc per day [26].
Discussion
The study carried out by Majke et al, in which they consider that the first step for proper management of diastasis recti is physical therapy. The second treatment option should be surgery, open or laparoscopic, both with high success rates. The surgical approach includes different plication techniques. Recurrence and complication are low, with improvement in lumbar pain, urinary incontinence and quality of life [27]. Another study conducted by Salvatore et al analyzed the evolution of 172 patients who underwent preaponeurotic endoscopic repair between August 2017 and December 2019. One hundred twenty-four patients were followed up for at least one year. Sixty-three patients responded to a satisfaction and quality of life survey 12 months after surgery. It was concluded that endoscopic repair is safe and effective for the treatment of diastasis recti [28]. We consider the implemented methodology to be a strength, with respect to the literature search, selection of relevant articles, quality assessment and data extraction. Therefore, we could conclude that the endoscopic approach for the repair of diastasis recti is a good alternative to surgical treatment, and thus improves the quality of life of patients.
Conclusion
Diastasis recti is an increase in the distance between the rectus abdominis muscles in the midline caused by weakness in the anterior abdominal wall. Most experts agree that there is weakness, thinning, and widening of the linea alba and associated abdominal muscle weakness. Currently there are different therapeutic approaches for diastasis recti, among which we can highlight physiotherapy, in which the doctor can start the treatment of diastasis recti by referring the patient to a physiotherapist for conservative treatment. The other approach is surgical, which can be open surgery, laparoscopic surgery, and robot-assisted surgery. The preaponeurotic endoscopic repair allows us to resolve the parietal defect with the placement of a reinforcement supraaponeurotic prosthesis, which will reduce recurrence, increasing plastic safety, without entering the abdominal cavity, with good aesthetic and functional results.
References
- Akram J, Matzen SH (2014) Rectus abdominis diastasis. J Plast Surg Hand Surg 48(3): 163-169.
- Bucaria V, Boccuzzi A (2021) Autologous Dermal Mesh in Severe Postpregnancy Recti Muscles Diastasis. Aesthetic Plast Surg 45(1): 198-211.
- Mommers EHH, Ponten JEH, Al Omar AK, de Vries Reilingh TS, Bouvy ND, et al. (2017) The general surgeon's perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc 31(12): 4934-4949.
- Qu E, Wu J, Zhang M, Wu L, Zhang T, et al. (2021) The ultrasound diagnostic criteria for diastasis recti and its correlation with pelvic floor dysfunction in early postpartum women. Quant Imaging Med Surg 11(2): 706-713.
- Cherla DV, Bernardi K, Blair KJ, Chua SS, Hasapes JP, et al. (2019) Importance of the physical exam: double-blind randomized controlled trial of radiologic interpretation of ventral hernias after selective clinical information. Hernia 23(5): 987-994.
- Mrdutt MM, Papaconstantinou HT, Robinson BD, Bird ET, Isbell CL (2019) Preoperative Frailty and Surgical Outcomes Across Diverse Surgical Subspecialties in a Large Health Care System. J Am Coll Surg 228(4): 482-490.
- Carlstedt A, Bringman S, Egberth M, Emanuelsson P, Olsson A, et al. (2021) Management of diastasis of the rectus abdominis muscles: recommendations for swedish national guidelines. Scand J Surg 110(3): 452-459.
- Laframboise FC, Schlaff RA, Baruth M (2021) Postpartum Exercise Intervention Targeting Diastasis Recti Abdominis. Int J Exerc Sci 14(3): 400-409.
- Mota P, Pascoal AG, Sancho F, Bø K (2012) Test-retest and intrarater reliability of 2-dimensional ultrasound measurements of distance between rectus abdominis in women. J Orthop Sports Phys Ther 42(11): 940-946.
- Juárez MD, Verasay G, Garcia Walter M (2017) Reparación endoscópica prefascial de la diástasis de los rectos: descripción de una nueva té Rev Hispanoam Hernia 5(2): 47-51.
- Bezama Murray J (2017) Técnica quirúrgica para reparar la diástasis de los rectos asociada a hernia umbilical. Diez años de experiencia. Rev Hispanoam Hernia 5(2): 52-56.
- Sperstad JB, Tennfjord MK, Hilde G, Ellstrom Engh M, Bo K (2016) Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med 50(17): 1092-1096.
- Carlstedt A, Petersson U, Stark B, Bringman S, Egberth M, et al. (2018) Abdominell rektusdiastas kan ge funktionella besvä Lakartidningen 115: 1-3.
- Benjamin DR, van de Water ATM, Peiris CL (2014) Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy 100(1): 1-8.
- Keshwani N, Mathur S, McLean L (2018) Relationship between interrectus distance and symptom severity in women with diastasis recti abdominis in the early postpartum period. Phys Ther 98(3): 182-190.
- Emanuelsson P, Gunnarsson U, Dahlstrand U, Strigard K, Stark B (2016) Operative correction of abdominal rectus diastasis (ARD) reduces pain and improves abdominal wall muscle strength: a randomized, prospective trial comparing retromuscular mesh repair to double-row, self-retaining sutures. Surgery 160(5): 1367-1375.
- Gluppe SL, Hilde G, Tennfjord MK, Engh ME, Bo K (2018) Effect of a postpartum training program on the prevalence of diastasis recti abdominis in postpartum primiparous women: a randomized controlled trial. Phys Ther 98(4): 260-268.
- Kamel DM, Yousif AM (2017) Neuromuscular electrical stimulation and strength recovery of postnatal diastasis recti abdominis muscles. Ann Rehabil Med 41(3): 465-474.
- Walton LM, Costa A, LaVanture D, McIlrath S, Stebbins B (2016) The effects of a 6 week dynamic core stability plank exercise program compared to a traditional supine core stability strengthening program on diastasis recti abdominis closure, pain, oswestry disability index (ODI) and pelvic floor disability index scores (PFDI). Phys Ther Rehabil 3: 1-9.
- Kim JK, Jang JY, Hong YG, Sim HB, Sun SH (2016) Deep-plane lipoabdominoplasty in East Asians. Arch Plast Surg 43(4): 352-359.
- Kohler G, Fischer I, Kaltenbock R, Schrittwieser R (2018) Minimal invasive linea alba reconstruction for the treatment of umbilical and epigastric hernias with coexisting rectus abdominis diastasis. J Laparoendosc Adv Surg Tech A 28(10): 1223-1228.
- Nardi WS, Busnelli GL, Tchercansky A, Pirchi DE, Medina PJ (2018) Diastasis recti associated with midline hernias: totally subcutaneous video-endoscopic repair. J Minim Access Surg 14(2): 161-163.
- Schwarz J, Reinpold W, Bittner R (2017) Endoscopic mini/less open sublay technique (EMILOS)-a new technique for ventral hernia repair. Langenbecks Arch Surg 402(1): 173-180.
- Gomez Menchero J, Guadalajara Jurado JF, Suarez Grau JM, Bellido Luque JA, Garcia Moreno JL, et al. (2018) Laparoscopic intracorporeal rectus aponeuroplasy (LIRA technique): a step forward in minimally invasive abdominal wall reconstruction for ventral hernia repair (LVHR). Surg Endosc 32(8): 3502-3508.
- Köhler G, Luketina RR, Emmanuel K (2015) Sutured repair of primary small umbilical and epigastric hernias: concomitant rectus diastasis is a significant risk factor for recurrence. World J Surg 39(1): 121-126.
- Henriksen NA, Jensen KK, Muysoms F (2019) Robot-assisted abdominal wall surgery: a systematic review of the literature and meta-analysis. Hernia 23(1): 17-27.
- M Lyhne, S Oberg J (2019) Rosenberg Treatment Options for Abdominal Rectus Diastasis. Front Surg 6: 65.
- S Cuccomarino, L Domenico, F Apra (2022) Preaponeurotic endoscopic repair (REPA) of diastasis recti: a single surgeon's experience. Surg Endosc 36(2): 1302-1309.

 Research Article
Research Article