Editorial
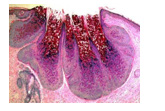
Figure 1: Molluscum contagiosum demonstrating a centric, waxy core pervaded with virions confined to superficial stratified squamous epithelial layer [1].
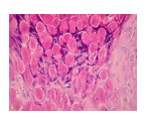
Molluscum contagiosum or ‘water warts’ emerges as an extremely contagious, cutaneous viral infection engendered by molluscum contagiosum virus of poxvirus family. Molluscum contagiosum virus is confined to superficial cutaneous layers wherein centroidal, waxy core is permeated by the virus [1,2]. Onset of lesions occurs in around seven weeks following viral exposure. Mean duration of an outbreak of lesions appears at 6 months to five years wherein immunosuppressed individuals demonstrate a prolonged duration [1,2]. Molluscum contagiosum virus disseminates through direct or sexual contact, with contact sports, contact with infected fomites, autoinoculation with scratching or picking the lesions or sharing of contaminated objects as towels. Self-inoculation within diverse region of the body is common in children and widespread, clustered lesions may be discerned [1,2]. Factors contributing towards emergence of molluscum contagiosum are atopic dermatitis, immunodeficiency or crowded living area with inadequate sanitation. Re-infection following a singular infection may ensue [1,2]. Appropriate discernment of the condition is contingent to classical appearance of lesions subject to confirmation by cogent histological examination [1,2]. Commonly discerned within the face, neck, axilla, torso, extremities, abdominal region or genital region, no area of disease emergence is exempt. The condition is frequently discerned in children between one-year to10 years. Typically, lesions in adults appear within the genital region [1,2]. Commonly, irritated, pruritic, non-painful, singular or clustered, miniature, elevated, pink nodules are observed. Molluscum contagiosum exemplifies flesh colored, dome shaped, pearly lesions with a centric punctum and magnitude varying from one millimeter to 5 millimeters. Upon microscopy, molluscum contagiosum characteristically demonstrates molluscum bodies or Henderson-Petersen bodies confined to superficial epidermal layer, superimposing upon the stratum Basale Figures 1 & 2. Cells imbued with abundant, enlarged, granular, eosinophilic cytoplasmic inclusion bodies or accumulated virions with eccentric, peripherally displaced, miniature, compressed nuclei are delineated [1,2].
Circumvention of disease may be obtained with appropriate hygiene and restricted sharing of personal items [3,4]. Spontaneous resolution of lesions in the absence of scarring may occur within a year. Thus, a wait and watch policy may be beneficially adopted. Picking or scratching of lesions may augment viral dissemination, induce bacterial infection, engender scarring or contribute to occurrence of eczema circumscribing the lesions [3,4]. Although treatment is unnecessary, lesions can be exterminated for cosmetic concerns or preventing disease dissemination [3,4]. Eradication of lesions can be accomplished with scraping intrinsic segment of the lesion, a maneuver which may induce scarring [3,4]. Oral agents such as cantharidin or cimetidine within the Paediatric population appear efficacious in expunging molluscum contagiosum. Topical podophyllotoxin or tretinoin can engender disease resolution [3,4]. Mild instances can be treated with salicylic acid which decimates duration of infection [3,4]. Imiquimod is an immunotherapy which can be suitably adopted to treat lesions of molluscum [3,4]. Surgical procedures as cryosurgery employing liquid nitrogen to freeze the lesions or lesion curettage appear optimal. Laser therapy with pulsed dye laser can be advantageously adopted to exterminate lesions of molluscum contagiosum [3,4]. Majority of lesions of molluscum contagiosum resolve spontaneously within nine months to two years. With perpetual cutaneous evolution, possible transmission of infection to family members or associated individuals may ensue. However, following competent eradication spontaneous reoccurrence is unperceived [3,4].
Figure 2: Molluscum contagiosum delineating abundant, eosinophilic, intra-cytoplasmic viral inclusion bodies with an eccentric, miniature nucleus and circumscribing stratified squamous epithelial layer [2].
References
- Müller CSL, Laue M, Kim Kremer, Stephanie Becker, Thomas Vogt, et al. (2018) Molluscum-contagiosum-Virus in einer Epidermalzyste. J Dtsch Dermatol Ges 16(9): 1144-1146.
- Clebak KT, Malone MA (2018) Skin Infections. Prim Care 45(3): 433-454.
- Peterson AR, Nash E (2019) Infectious Disease in Contact Sports. Sports Health 11(1): 47-58.
- Rosner M, Zloto O (2018) Periocular molluscum contagiosum: six different clinical presentations. Acta Ophthalmol 96(5): e600-e605.

 Editorial
Editorial