ABSTRACT
During the last three weeks, cases of Human monkeypox have been diagnosed in as many as 24 non-endemic countries (Human monkeypox are usually endemic to West as well as Central African countries like the Democratic Republic of the Congo, Nigeria and others) with the diagnosed cases not having any directly detected travel history to any endemic country. This article presents a summary on this new global Human monkeypox outbreak with information that will be useful for both healthcare professionals and the general public.
Keywords: Monkeypox Outbreak; Monkeypox Virus; Human Monkeypox; Skin Lesions with Fever; Epidemiological Alert Monkeypox; MVA-BN; Imvamune or Imvanex or Jynneos Monkeypox Vaccine
Introduction
Since the second week of May 2022, a sudden outbreak of Human monkeypox cases has been observed in as many as 21 non-endemic countries [1-5]. The concerning aspect of this 2022 outbreak of Human monkeypox is that many of the diagnosed cases didn’t exhibit any direct travel history to any endemic country or region [6]. Monkeypox ICD-10 B04 [7,8] is an infection that is primarily seen in Central and West African countries that have tropical forests populated with animals which can act as hosts for this virus [3,6,9-12]. Human monkeypox refers to a virus-based zoonosis that is caused by the monkeypox virus. The monkeypox virus is a member of the Orthopoxvirus family that also includes the variola virus responsible for causing smallpox. Since it’s discovery, there have been found to be two genetically separate strains of the monkeypox virus namely the Congo Basin (Central African) strain and the West African strain. In the past, Human monkeypox infections caused by the West African strain have shown to be of low severity in comparison to the infections caused by the Congo Basin strain [1,2,11,12].
Facts known about the Ongoing Human Monkeypox Virus Infection
Human monkeypox is a viral infection which has been transmitted to human beings from animals (mainly monkeys) and the human version spreads through direct or close contact with an infected individual [4-8]. Thus, it is safe to say that human monkeypox is generally transmitted by both direct and indirect contact with the bodily fluids of an infected person like their blood, bodily fluids, their skin or mucosal lesions and their clothes or belongings that have some degree of infected bodily fluids on them [1,4,5,7,8,12]. Secondary or person-to-person spread may take place also in people who touch the infected respiratory secretions, the skin lesions or contaminated belongings of the infected individual [8,10]. In previous outbreaks, the main route of transmission was found to be close contact with infected respiratory droplets. Human monkeypox infections can also be transmitted through inoculation or via the transplacental route from mother to foetus (this is known as congenital monkeypox). Even though most of the initial cases of Human monkeypox have been diagnosed in sexual health care clinics amongst men who have sex with other men, the most probable route of infection was the close contact with skin lesions of the infected person [4,5,7-9,12].
The main symptoms of Human monkeypox infection are fever (>38.5℃), headache, joint and muscle pains with subsequent presentation of a skin rash that is generally localized to the patient’s face, palm section of the hands and the soles of their feet. Other symptoms include lymphadenopathy (this refers to the presence of swollen lymph nodes), profound myalgia (this means having severe muscle and body pains), pain in the back and presenting with asthenia (serious degree of weakness). The incubation period is usually 6 to 16 days but has been reported as ranging from 5 to 21 days [5-7]. The infected individuals remain contagious from the onset of the above mentioned symptoms till the skin lesions are completely cured [7]. A confirmed case of Human monkeypox is one in which the patient presents with symptoms and probable cause (direct contact with an infected person or a travel history to endemic regions) followed by laboratory confirmation of having the monkeypox virus (done using molecular protocols like the realtime PCR test as well as genetic sequencing where possible) [11,12].
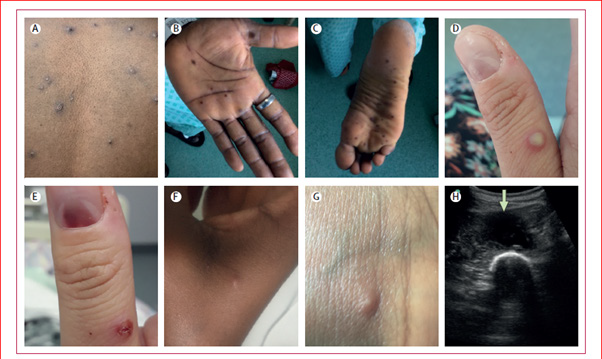
Figure 1: The appearance and progression of the different types of skin lesions in the second stage of the Human monkeypox infection (Source: 1).
The Human monkeypox infection in a patient has two clear stages. The first stage is the period of incubation and invasion (generally lasts between 5-21 days). This first stage is the one in which the patient presents with fever, serious headaches, lymphadenopathy, acute pain within the lower back as well as serious asthenia. The second stage is the skin rash period (this occurs within three days after presenting with fever) and is characterized by the different phases of rash appearance. It usually affects the face first and then spreads to the rest of the body (see Figure 1 below) [1]. The most affected areas are the face (in 96% of cases), the palms of the hands and the soles of the feet (in 75% of cases). The progression of skin rashes from maculopapular (the flat-based type of lesions) to vesicles (the fluid-filled blister type of lesions), pustules, and the formation of crusts in the end takes place within a 10-12 day period. The drying and falling of the scabs may occur or continue for almost 21 days.
Status of the Present Ongoing Human Monkeypox Outbreak on a Global Scale
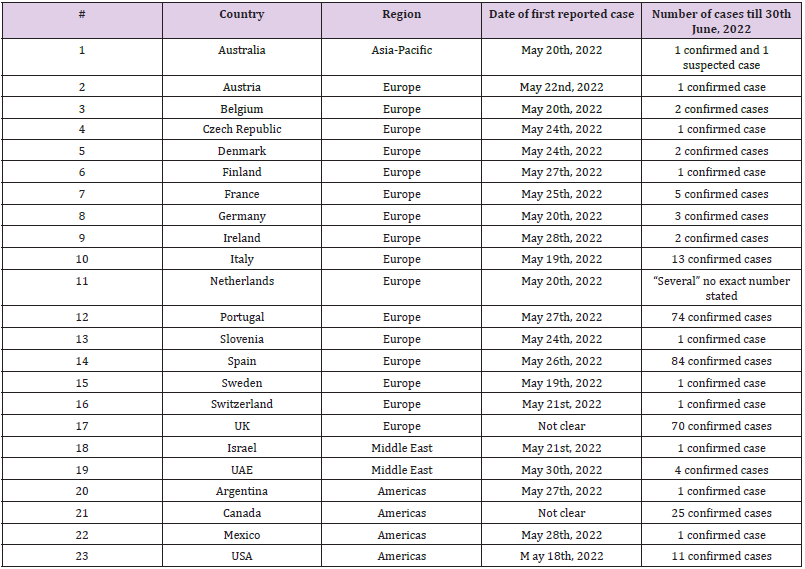
Human monkeypox which spreads via direct person-to-person contact has always been low, but the appearance of the present outbreaks in as many as 24 non-endemic nations poses a definite risk to the general public (see Table 1 below) [8,11,12].
Table 1: Status Report of the present Human monkeypox outbreak as of 30th May 2022 (Sources of data: 8, 11-15).
Potential Mitigation of Transmission, the Guidelines for Diagnosis and Existing Treatment Options
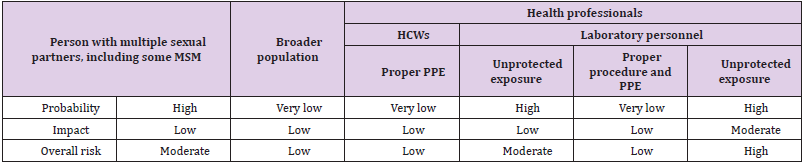
Monkeypox symptoms usually get resolved in the patient with only supporting management and treatment. Still, in the present outbreak, it is of vital importance to contain the outbreak by limiting contact with patients, contact tracing, swift information of contact status to the contacts and isolation of such contacts. The risk summary in the present 2022 Human monkeypox virus for various populations was carried out by the EDEC and is presented in Table 2 below [12]. Patients must be kept isolated till the skin rashes are totally cured and must limit or totally abstain from contact with immune-suppressed individuals (at high risk of contracting the Human monkeypox infection) persons and pets. There is also need to avoid sexual activity and close physical proximity until the skin lesions are healed. Most patients can be cared for at home with supportive care. Those who come in close contacts of Human monkeypox cases need to carry out self-monitoring for any presentation of the disease symptoms up to 21 days from the last exposure to the patient.
Table 2: Summary of risk assessment for contracting the Human monkeypox virus in various population groups as published by the EDEC [12].
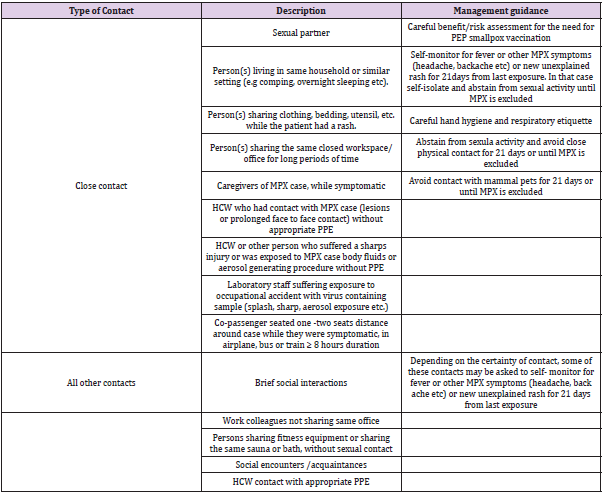
Health care staff and certain populations are more susceptible to getting infected. Health care staff needs to wear appropriate PPE (personal protection equipment) like gloves, water-resistant gown, FFP2 respirator when in touch with suspected cases or providing care to diagnosed patients. Laboratory personnel that test for the Human monkeypox virus must take mandatory precautions to mitigate occupational exposure [12]. A summary of treatment and management guidance for Human monkeypox cases has been published by the EDEC and is shown in Table 3 below. This will be useful as a reference point for health care professionals [12].
Table 3: Summary of treatment and management strategy for those in close contact with a Human monkeypox patient as published by the EDEC [12].
The strict compliance with sanitary hygiene protocols (regularly disinfecting hands after contact with the patient) by care givers and all in contact with the patients is mandatory. The surveillance, case assessment, contact tracing, follow-up, laboratory diagnosis, assessment and management of the patients should follow the WHO guidelines [10,11] or the EDEC guidelines [12] as per the country’s health care policies [5-7,11,12].
The WHO, the EDEC and USA’s CDC (The Centre for Disease Control and Prevention) are responding to this event as a high priority to avoid further spread [6-15]. The WHO has also recommended safe sex as many of the present cases on a global scale seem to have been diagnosed in men who have sex with other men. Infected people and those in contact with them have to abstain from contact with pet or domestic animals to prevent the jumping of the monkeypox virus infection in these susceptible populations [5-7,11,12]. At present, there are no validated as well as licensed treatment protocols for human monkeypox. However, two orally used medicines namely brincidofovir and tecovirimat have been given approval by the FDA (Food and Drug Administration), USA for the treatment of smallpox as emergency strategies in the event of any future bioterrorism event. None of these two medications have been assessed properly in human clinical trials for effectiveness against other members of the Orthopoxvirus family including the Human monkeypox virus. There has been some compassionate usage of tecovirimat in the Central African Republic, where Human monkeypox outbreaks are common [1].
In terms of prevention through vaccination, there are a few vaccines available for preventing smallpox which give a certain degree of protection against the Human monkeypox virus. One of the more recent vaccines that was made for smallpox namely MVABN (also called Imvamune or Imvanex or Jynneos) has been given approval in the year 2019 for usage in prevention of the spread of the Human monkeypox infection. However the drawback is that this vaccine isn’t freely accessible globally at present. The WHO is presently working towards better availability by collaborating with the makers. It is of importance to know that individuals who are in the above 40 age group were vaccinated against smallpox as it had not been eradicated and this provides them some measure of protection against the Human monkeypox virus. The issue that is worrisome at present is that these original smallpox vaccines were withdrawn from public circulation after smallpox was eradicated. As such, people in the below 40 population were most probably not given smallpox vaccination after the year 1980. In some countries, some of the highly at risk health care staff might be given a more recent smallpox vaccine [15].
Conclusion
The UN and WHO are of the opinion that the present global outbreak of Human monkeypox in non-endemic countries is still a controllable public health situation. However, there is need for every country to carry out appropriate surveillance, reporting of cases, contact tracing, adequate management as well as the compliance with the prevention, management and treatment guidelines provided by WHO [10,11,15] as well as the EDEC guidelines [12] or the CDC [13,14], depending on the country’s health care policies. The general public can consult the WHO factsheet [15] and the EDEC or CDC websites for general awareness and information on the Human monkeypox infection.
Acknowledgment
I thank Mr. Bharat Sharma for his extended support in data collection and authentication of the validity of the sources during this study.
Data Availability Statement
Data available in article.
Funding
Not applicable.
Conflict of Interest
No conflicts of interest to disclose.
References
- Adler H, Gould S, Hine P, Snell LB, Wong W, et al. (2022) Clinical features and management of human monkeypox: a retrospective observational study in the UK. The Lancet Infectious Diseases.
- Mauldin MR, McCollum AM, Nakazawa YJ, Mandra A, Whitehouse ER, et al. (2022) Exportation of monkeypox virus from the African continent. The Journal of infectious diseases 225(8): 1367-1376.
- (2022) European Centre for Disease Prevention and Control (EDEC). Epidemiological update: Monkeypox multi-country outbreak.
- (2022) Pan American Health Organization (PAHO). Monkeypox – Your questions answered.
- (2022) Pan American Health Organization (PAHO). Monkeypox.
- (2022) The World Health Organization (WHO). Multi-country monkeypox outbreak in non-endemic countries.
- (2022) Pan American Health Organization (PAHO). Epidemiological Alert Monkeypox in non-endemic countries - 20 May 2022.
- (2022) The United Nations (UN). Monkeypox outbreak can still be contained, insists UN health agency.
- Rao AK, Schulte J, Chen TH, Hughes CM, Davidson W, et al. (2022) Monkeypox in a Traveler Returning from Nigeria—Dallas, Texas, July 2021. Morbidity and Mortality Weekly Report 71(14): 509-516.
- (2022) World Health Organization (WHO). Surveillance, case investigation and contact tracing for monkeypox: interim guidance.
- (2022) World Health Organization (WHO). Laboratory testing for the monkeypox virus: interim guidance.
- (2022) European Centre for Disease Prevention and Control (EDEC). ASSESSMENT RR Monkeypox multi-country outbreak.
- (2022) Centre for disease control and prevention (CDC). U.S. Monkeypox 2022: Situation Summary.
- (2022) Centre for disease control and prevention (CDC). Monkeypox in Multiple Countries.
- (2022) The World Health Organization (WHO). Monkeypox.

 Review Article
Review Article