ABSTRACT
The diabetic foot is defined as the ulceration and destruction of the deep tissues of the foot due to the suffering of diabetes mellitus, which is a disease of great prevalence and importance today, due to its high rates in the world, therefore, it is necessary that measures be implemented as a treatment of it, that meet various conditions such as reduced wound volume, rapid healing and granulation of new tissue. In recent years, the use of negative pressure systems has been implemented, which, compared to other treatments, has yielded gratifying results, which is why in the following review article, the current literature on this technique is analyzed, to evaluate its effectiveness in this type of injury.
Keywords: Diabetic Foot; Treatment; Negative Pressure; Diabetes Mellitus
Abbreviations: IDF: International Diabetes Federation; PVD: Peripheral Vascular Disease; NPWT: Negative Pressure Therapy for Wounds; VAC: Vacuum-Assisted Closure; PDGF: Platelet-Derived Growth Factors
Introduction
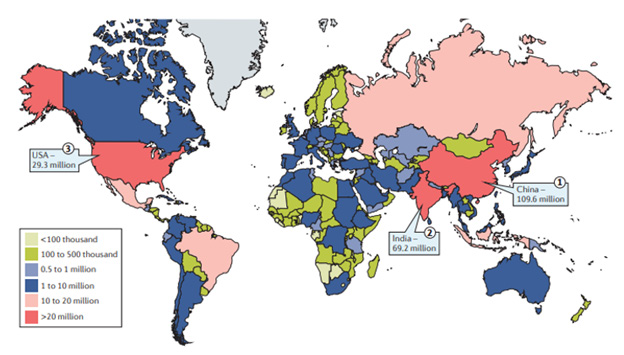
Diabetes mellitus is a group of physiological dysfunctions characterized by hyperglycemia resulting directly from insulin resistance, inadequate insulin secretion, or excessive glucagon secretion [1]. The International Diabetes Federation (IDF) estimated that 1 in 11 adults aged 20 to 79 (415 million adults) had diabetes mellitus worldwide in 2015. It is estimated that the year 2040 will see an increase to 642 million people, with the largest increases coming from regions experiencing economic transitions from low- to middle-income levels [2]. The different reasons for the growing epidemic of diabetes mellitus are multiple, including population aging, economic development, urbanization, unhealthy eating habits and sedentary lifestyles. More than 90% of cases of diabetes mellitus correspond to type 2 diabetes mellitus [3]. Between 2010 and 2030, a 20% increase in the number of adults with diabetes mellitus is estimated in developed countries and a 69% increase in developing countries [4]. Asia has become the main area with a growing epidemic of type 2 diabetes mellitus. China and India are the two main epicenters of the type 2 diabetes mellitus epidemic (Figure 1). In these countries, the epidemic of type 2 diabetes mellitus is characterized by a lower onset with bMI and a younger age than in Western populations [5]. According to data from India, China, Thailand, and Malaysia, the cost of hospitalized patients with diabetes mellitus but no complications accounted for 11 to 75% of per capita income in 2007, and hospitalized patients who had complications spent up to three times more than those without complications [6]. In 2015. U.S. It was included as the country or territory with the third highest number of patients with diabetes mellitus (Figure 1), and half of adults aged 65 years and older had prediabetes mellitus in 2008 [7]. In addition, the Middle East is another hotspot of the diabetes mellitus epidemic, with a prevalence of diabetes mellitus among adults ranging from 9.5% in Oman to 25.4% in Saudi Arabia [8]. According to the Global Burden of Disease report, diabetes mellitus was positioned as one of the main causes of years of life lost and has a great impact on Latin American countries [9].
Figure 1: Estimated total number of adults (20–79 years) living with diabetes mellitus, highlighting the top three countries or territories for number of adults with diabetes mellitus (20–79 years) in 2015. It was estimated that in 2015, 415 million adults aged 20–79 years had diabetes mellitus worldwide, and about 46.5% of them lived in three countries: China, India and the USA. The colour of the country or territory in the map relates to the total number of adults aged 20–79 years living with diabetes mellitus in the area. Tomada de: Zheng Y, Ley, SH y Hu, FB (2017) Etiología y epidemiología global de la diabetes mellitus tipo 2 y sus complicaciones. Nature Reviews Endocrinology 14(2): 88-98.
Pathogenesis and Pathophysiology of Diabetes Mellitus
Type 1 Diabetes Mellitus
Type 1 diabetes mellitus is characterized by the autoimmune destruction of insulin-producing cells in the pancreas by CD4+ and CD8+ T cells and macrophages infiltrating islets [10]. Several aspects characterize diabetes mellitus as an autoimmune disease: presence of immunocompetent and accessory cells in pancreatic islet infiltrates, association of susceptibility to diseases with class II (immunity response) genes of the main histocompatibility complex, presence of islet cell-specific autoantibodies, alterations of T-cell-mediated immunoregulation, in particular in the CD4+ T cell compartment, the involvement of monokines and TH1 cells that produce interleukins in the disease process, response to immunotherapy and frequent occurrence of autoimmune diseases specific toother organs or diseases in affected persons or their relatives [11].
Type 2 Diabetes Mellitus
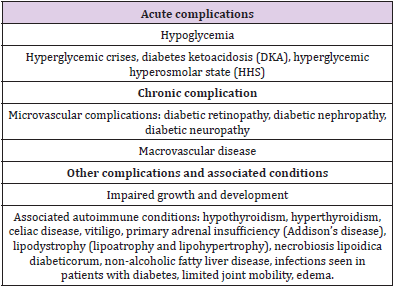
In type 2 diabetes mellitus, the mechanisms are broken, as a consequence of the two main pathological defects of type 2 diabetes mellitus being altered insulin secretion through pancreatic B-cell dysfunction and altered insulin action due to insulin resistance [12]. Diabetes mellitus can have several complications ranging from acute complications, chronic complications, and other complications with associated conditions [10] (Table 1).
Therefore, we can highlight that diabetes mellitus is described as a chronic metabolic disease that is characterized by insulin deficiency, hyperglycemia and other alterations in carbohydrate and lipid metabolism, which can cause multiple complications at the micro and macrovascular level. Diabetic foot is the infection, ulceration, and destruction of deep tissues, associated with neurological abnormalities (loss of sensitivity to pain) and peripheral vasculopathy in the lower extremities. In these cases, the foot is more vulnerable to circulatory and neurological conditions, so the slightest trauma can cause ulcers or infections. Macrovascular disease of the lower extremities is common, progresses rapidly, and presents a characteristic peritibial distribution to which fragility of the arteries of the foot is added [13]. Foot problems occur in both type 1 and type 2 diabetes and the lifetime risk of a patient developing a foot ulcer has been estimated to be 25% [14]. Ulcers are more common in men and in patients over 60 years of age. A population-based study of more than 10,000 patients conducted in the North East of England reported that 5% had foot ulceration in the past or present and that nearly 6% had one or more risk factors and the annual incidence of ulceration in these diabetic patients was 2.2% [15].
Pathogenesis of Diabetic Foot Ulcer
Diabetic foot ulcer is the consequence of a complicated interaction of several risk factors including peripheral neuropathy, peripheral vascular disease, foot deformities, arterial insufficiency, trauma, and impaired resistance to infections [16].
Neuropathy
Neuropathy is a disease that affects the nerves and causes deterioration of sensations, movement and other aspects of health, depending on the nerve affected. Peripheral neuropathy in diabetes is one of the leading causes of foot ulcers [17].
Peripheral Vascular Disease
Peripheral vascular disease (PVD) is an atherosclerotic occlusive disease of the lower extremities. Diabetes is a major risk factor for PVD [18].
Classification
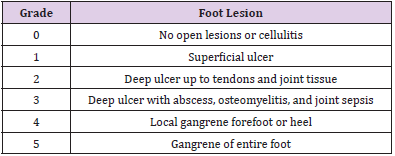
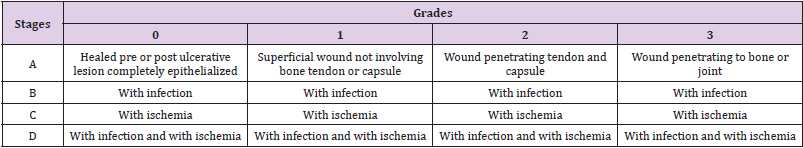
Currently, the classification of the ulcer is estimated to a wide variety that includes characteristics such as depth, size, appearance and location, etc. Evaluation should determine the etiology of the ulcer and verify whether the lesion is neuropathic, ischemic, or neuroischemic [16]. Therefore, it is important to have an appropriate classification system including these characteristics in order to project strategies for the treatment of diabetic foot injuries. One of these classifications includes the Wagner-Meggit classification (Table 2). This system includes six grades that take into account the depth of the ulcer, the presence of gangrene and the level of tissue necrosis [19]. Another outstanding classification corresponds to the classification system of the University of Texas Antonio (UTSA) evaluates diabetic foot injury according to depth, wound infection and the presence of ischemia in the lower extremities (Table 3). In this system, classification is made based on the depth of the lesion and states are classified based on the presence of ischemia, wound bio load, or a combination of both, excluding neuropathy [20].
Treatment
Preventive strategies in the form of patient education and periodic foot assessments for peripheral vascular disease and neuropathy, along with risk stratification, form the basis of diabetic foot treatment [21]. For the treatment of diabetic foot ulcer, several methods are taken into account such as glycemic control, pharmacological therapy, improvement of vascularization or an increasingly used method such as negative pressure therapy. When we talk about subatomospheric pressure, which is also known as negative pressure, it is a name used to describe a pressure lower than normal atmospheric pressure [22]. Negative pressure therapy aims to improve tissue perfusion and promote the formation of granulation tissue and often shorter treatment compared to ulcers treated with a traditional gauze dressing [23]. The basis of this technique is to progress the chronic wound from the inflammatory phase to the proliferative phase There are different mechanisms that could be responsible for the beneficial effects of treatment such as increased total blood flow, reduction of edema, stimulation of the formation of granulation tissue, stimulation of cell proliferation, elimination of soluble inhibitors of wound healing, reduction of bacterial load, approach of the edges of the wound to each other [24]. Therefore, negative pressure therapy offers optimal results when a multidisciplinary team is used in the treatment of diabetic foot wounds.
Methodology
In this review article, a detailed bibliographic search of information published since 2011 was carried out in the PubMed, Elsevier, Scielo databases, national and international libraries. We use the following descriptors: Diabetic foot, treatment, negative pressure, diabetes mellitus. The data obtained range from 2 to 15 records after the use of the keywords. The search for articles was conducted in Spanish and English, limited by year of publication, and used studies published since 2011.
Results
Melodie Blakely reports a case report of a 47-year-old woman with a history of more than five years of full-thickness diabetic foot ulcer on her left middle plantar foot. Her Diabetic Foot Ulcer (UPD) had been managed by her podiatrist throughout its course and the patient reported that the wound had been continuously open during this time. The intervention used different methods including negative pressure therapy for wounds (NPWT) in the fourth week using the Modified Vacuum-Assisted Closure (VAC) device by attaching the tube clamping pad to the distal leg with foam to prevent pressure from the tube on the plantar surface. The NPWT configuration was 125 mmHg, continuous. This was changed three times a week. Weekly debridements and discharges continued. By week five, the depth of the wound had decreased by 50%. By week seven, the wound bed was clean, shallow but with persistent coiled edges, despite debridement at each visit. At week 12, the wound measured 0.5 x 0.5 mm with 0.1 cm depth; at week 15, the wound was 100% epithelialized and the patient was able to transition to custom molded diabetic footwear [25]. Another case report given at the University Hospital of Rebro (Zagreb, Croatia) reports the case of a 43-year-old woman with an infected wound on her left foot. The patient had a history of reactive arthritis and was prescribed corticosteroid treatment when the disease was in its active phase.
He was also diagnosed with type 2 diabetes mellitus 6 months before hospitalization, so he was taking oral antidiabetic medication. Seven days before admission, the patient cut her left foot after stepping on a sharp stone. Over the course of a week after the injury, the swelling and redness progressively worsened, and a purulent discharge from the wound gradually developed. He did not consult his primary care doctor before presenting himself to the hospital. Based on clinical, radiological and laboratory findings, surgical intervention was determined to be the best method of treatment. Negative pressure wound therapy (NPWT) was applied at intermittent pressures from -60 mm Hg to -100 mm Hg. The surface of the wound remained clean throughout the time; there were no signs of purulent secretions or local redness, and the patient was afebrile. Skin grafts were used for the wound and 10 months after the initial operation, the patient is well. The wound site successfully healed with 100% graft taking [26]. Another case report of a 34-year-old male with a history of type 1 diabetes and Charcot neuroarthropathy who consults for a chronic UPD of the right plantar medial surface. There was no sign of infection. The ulcer had persisted for 6 months; Previous treatment consisted of efforts to discharge the pressure with a surgical shoe and a removable plaster boot. The wound was also treated with topical therapies, including clostridial collagenase, human platelet-derived growth factors (PDGF), and 6 applications of a human amniotic membrane allograft.
At the initial visit, the ulcer measured 3.8 cm x 3.7 cm x 3 mm. The hyperkeratotic margins of the UPD were debrided and NPWT was initiated using durable non-disposable medical equipment at -125 mm Hg continuously. All debridements were sharp debridements using a scalpel blade. A contact layer was then applied to the wound bed with the advanced collagen matrix wound that contained alginate and was designed with uniform perforations to facilitate the removal of the exudate. The NPWT sponge and secondary dressings were changed 3 times a week. The patient was instructed to use crutches and to maintain the weight of the affected foot as much as possible. The patient returned to the clinic on day 7 and then every 2 weeks for the rest of his care. After the first week, debridement was performed every 2 weeks and the collagen dressing of the wound contact layer was changed weekly with the application of NPWT. Wound healing progressed with the treatment regimen described above of biweekly debridement and weekly application of the collagen layer in contact with the wound with NPWT. By day 35, the total wound area had decreased by 91%, measuring 3.2 mm x 1.2 mm x 1 mm [27].
Discussion
In recent years, the great increase in ulcers and other complications of diabetes mellitus, mainly diabetic foot, have increased cases of morbidity and mortality in the world, causing this type of patients to suffer a progressive dependence and therefore a considerable decrease in their quality of life, which represents an increase in the need for the implementation of effective treatment techniques against this type of injury. Topical negative pressure therapy (NPT) is widely disseminated for the treatment of this type of wounds, with the basis that it favors its closure, which is why its use has increased in recent years. NPT, or subatopheric pressure therapy, is a system that uses negative pressure located topically in order to stimulate the healing of acute and chronic wounds. This therapy provides an alternative treatment in complex or difficult to resolve wounds, improving locoregional conditions and preparing the wound for definitive healing, through less complex surgical procedures. That is, NPT can be an adjuvant therapy before or after surgery, or it can even be an alternative to it in some cases. The inputs for healing with TPN are: a sponge, a tube, an adherent dressing, a vacuum pump and a reservoir. The wound surface should be covered directly with a sterile polyurethane sponge with a pore of 400 to 600 microns, which can be cut and adapted according to the shape and size of the wound. In the thickness of the sponge, a non-collapsible multifenestrated tube is placed so that it comes out of the healing parallel to the skin surface.
The sponge is covered by an adhesive dressing that must be extended at least 5 cm on the adjacent healthy skin and that wraps around the exit of the tube, in order to create an airtight system. In this way, an open wound is transformed into a closed and controlled wound. The other end of the evacuation tube is connected to a reservoir, where the exudate aspirated from the wound is deposited. In turn, the reservoir is connected to a vacuum generating pump or to the central suction system, which allows the pressure of the reservoir to be regulated. [28] which provides complete healing by stimulating granulation tissue formation, reducing wound size, microbiological control, decreasing the risk of amputation, decreasing adverse effects associated with treatment, low cost, and most importantly, great patient satisfaction. In their experimental and comparative study, Nain and others, included 2 groups of which one was applied negative pressure therapy and the other was not, in order to evaluate the degree of effectiveness of this, and it was evidenced that the group to which the therapy was applied generated granulation tissue, which led to the total healing of the injury. They concluded that NPT plays an important role in healing PD ulcers [29]. During the procedure, as part of the most important components is the dressing, which is in direct contact with the wound.
However, the literature confirms that a drawback of polyurethane foam dressings is that inside their pores can grow granulation tissue and cause discomfort to the patient at the time of their change. To avoid this situation it is recommended that the contact layer with the wound bed is the polyvinyl alcohol protection dressing and on top place the polyurethane foam. There is no study that shows that with gauze dressings granular tissue is formed in their pores, so in this case it is not necessary to use a protective layer [30]. As for the contraindications of the same, these dressings should not be placed directly on anastomotic areas, blood vessels, exposed nerves and organs, in addition if a significant hemorrhage appears, the therapy system must be interrupted as soon as possible, and an adequate control of the hemorrhage must be carried out. It can be reused only in the event that adequate hemostasis has been achieved and the patient has no risk of continuous bleeding [31] as this situation will only worsen the patient’s condition. On the other hand, a series of complications may appear such as leakage, obstruction, erosion or maceration of the periulceral skin and healthy tissue, pressure ulcer due to support on the drainage tube, pain [32], etc., however, their recurrence rates are quite low, as evidenced in the prospective study conducted by Ugurlar, in which 2 groups of chronic diabetic patients with Wagner grade 3-4 (foot wound of a single limb) were included.
The groups investigated were 10 patients with TPN application by means of a Y connector and 11 patients treated under bridge TPN [27]. The therapy was applied for a time of 40.2 (range 16-43) days in TPN with connector and in the TPN bridge 41.1 (range 23-63) wound diameters were identified in TPN connector of 6.1 (range 4.0-10.2) and TPN bridge 5.8 (range 3.7-8.7). It was found that the rates of recovery of the limb with 40% was of the connector group Y and of the 38.4% bridge group, without significant differences in the rescue of the limb, however the hospital stay and the diameter of the wounds of the groups was statistically significant (p<0.05), all patients reached a total healing without presenting any adverse event such as maceration of the adjacent tissues of the wound or necrosis [33] for which Garcia and others conclude in their retrospective observational study that the most frequent complication associated with the use of therapy is perilesional maceration and most adverse effects are considered mild and associated with external factors; these are easy to resolve and do not hinder the evolution of the lesion if properly managed [34]. In countries such as the USA, the United Kingdom and Germany, it is the treatment of first choice for lesions of vascular origin or diabetic foot, without having to become long-term lesions, both in the hospital environment and in Primary Care [35] that is, it is a method that can be used to prevent the progress of the injury, so it can be used in both acute and chronic wounds.
Providing in turn economic benefits such as lower hospitalization costs, lower treatment costs, rapid passage to a lower cost environment, greater productivity of medical and nursing equipment, reduced need for analgesics, reduced expenditure on dressings, lower use of ATB, prevention of operating room expenses, lower rehabilitation costs, lower burden on social resistance and reduction of time and costs in health care [36] among others, therefore, authors such as Calixto et al. conclude that topical negative pressure systems are an important alternative for the management of traumatic and post-surgical wounds in our environment [37], as do Perez and others, who conclude in their review of cases at the university clinic of Navarra that vacuum therapy helps to offer more complete assistance to patients, reducing their hospital stay times, optimizing hospital resources and avoiding in many cases more aggressive surgical maneuvers [38].
Conclusion
Diabetic foot is one of the most aggressive and invasive complications of diabetes mellitus, which taking into account epidemiological statistics is one of the diseases that occurs with greater recurrence worldwide, for all this, it is important to implement measures and techniques that allow the rapid resolution of this type of wounds, both acute and chronic in order to improve the quality of life of the patient, which is directly affected. The use of sub atmospheric pressure or negative pressure systems is one of the most innovative techniques used today, and taking into account the great benefits it brings, such as the complete closure of the wound, the decrease in the microbial population present in it and also the low costs it needs, this is cataloged as one of the most effective techniques for the treatment of this complication, which is reflected in the series of cases reviewed and in the current literature, however, its effectiveness as the first method of choice continues to be studied.
References
- Blair M (2016) Diabetes Mellitus Review. Urol Nurs 36(1): 27-36.
- (2015) International Diabetes Federation. IDF Diabetes Atlas (7th)., on. Diabetes Atlas.
- Zimmet PZ (2017) Diabetes and its drivers: the largest epidemic in human history?. Clin Diabetes Endocrinol 3(1).
- Shaw J, Sicree R, Zimmet P (2010) Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 87: 4-14.
- Kong A, Gang Xu, Nicola Brown, Wing-Yee So, Ronald CWM, et al. (2013) Diabetes and its comorbidities- where east meets west. Nat Rev Endocrinol 9: 537-547.
- Goldhaber-fiebert J (2010) Inpatient treatment of diabetic patients in Asia: Evidence from India, China, Thailand and Malaysia. Diabet Med 27: 101-108.
- (2011) National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation. National diabetes fact sheet: National estimates and general information on diabetes and prediabetes in the United States, 2011. Centers for Disease Control and Prevention.
- Al-rubeaan KL (2015) Epidemiology of abnormal glucose metabolism in a country facing its epidemic: SAUDI-DM study. J Diabetes 7(5): 622-632.
- Lozano R, Mohsen Naghavi, Kyle Foreman, Stephen Lim, Kenji Shibuya, et al. (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859): 2095-2128.
- Wondifraw H (2015) Classification, Pathophysiology, Diagnosis and Management of Diabetes Mellitus. Baynes J Diabetes Metab 6(5).
- Hussain AN, Vincent MT (2007) Type 1 Diabetes Mellitus.
- (2010) American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 33(1).
- Dubon M (2013) Diabetic foot. Rev Faculty Med of the UNAM 56(4).
- Singh N, Armstrong DG, Lipsky BA (2005) Preventing foot ulcers in patients with diabetes. J Am Med Assoc 293(2): 217-228.
- Abbott CA, Carrington AL, Ashe H, LC Every, J Griffiths, et al. (2002) The North-West Diabetes Foot Care Study: incidence of, and risk factors for new diabetic foot ulceration in a community-based patient cohort. Diabet Med 19: 377-384.
- Noor S, Zubair R, Ahmad J (2015) Diabetic foot ulcer--A review on pathophysiology, classification, and microbial etiology. Diabetes Metab Syndr 9(3): 192-199.
- Zochodone DW (2008) Diabetic polyneuropathy: An update. Curr Opin Neurol 21(5): 527-533.
- (2003) American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care 26: 3333-3341.
- Lipsky AB, Anthony R Berendt, H Gunner Deery, John M Embil, Warren S Joseph, et al. (2004) Diagnosis and treatment of diabetic foot infections. Clin Infect Dis 39(7): 885-910.
- Oyibo S, Jude E, Tarawneh I, Nguyen H, AJ Boulton, et al. (2001) A comparison of two diabetic foot ulcer classification systems: The Wagner and the University of Texas wound classification systems. Diabetes Care 24(1): 84-88.
- Zhang J, Su N, Thomas C (2017) Prevention and treatment of diabetic foot ulcers. J R Soc Med 110(3): 104-109.
- Sarabia M, Castanedo C (2014) What is the Pressure Topical Negative? Is it effective/efficient in wound closure complex? Topic Review. Gerokomos 25(1).
- (2006) Healthy quality ontario. Negative Pressure Wound Therapy: An evidence-based analysis. Ont Health Technol Assess 6(14): 1-38.
- Philbeck TE Jr, Whittington KT, Millsap MH, Briones RB, Wight DG, et al. (1999) The clinic and cost-effectiveness of externally applied negative pressure wound therapy in wound management in Medicare home health care patients. Ostomy Wound Manage 45: 41-50.
- Blakely M (2016) The Use of Best Practice in the Treatment of a Complex Diabetic Foot Ulcer: A Case Report. Healthcare (Basel) 4(1): 18.
- Smud-orehovec S, Marko Mance, Damir Halužan, Vilena Vrbanović-Mijatović, Davor Mijatović, et al. (2018) Defect Reconstruction of an Infected Diabetic Foot Using Split- and Full-thickness Skin Grafts with Adjuvant Negative Pressure Wound Therapy: A Case Report and Review of the Literature. Wounds 30(11): 108-115.
- Lehrman J (2020) Combining the Benefits of Collagen and Negative Pressure Wound Therapy to Heal a Chronic Diabetic Foot Ulcer: A Case Report. Wounds 32(3): 11-13.
- Lena T, Giachero V, Gaites B, Gil S Ledesma, Y Machado, et al. Treatment of diabetic foot wounds with negative pressure therapy.
- Tardáguila A (2015) Bioactive therapies applied to the treatment of complicated diabetic foot ulcers. Reduca (Nursing, Physiotherapy and Podiatry) Series of Final Degree Projects 7(1): 55-83.
- Martinez M (2015) Use of negative pressure therapy for wound healing. Final degree project. UNIVERSITAT DE LES ILLES BALEARS Curs Acadèmic 2014-2015.
- Zambrano A (2017) Benefits of vacuum-assisted negative pressure therapy (VAC) in the management of complex wounds that occur in patients of the Guayaquil National Police Teaching Hospital No. 2 from September 2016 to January 2017. Catholic University of Santiago de Guayaquil.
- Doalto Y, Diaz P (2016) Vacuum-assisted therapy. Another way to cure. Nuber Científ 3(18): 34-39.
- Roa E (2017) Negative Pressure as a Strategy for the Treatment of Chronic and Acute Wounds: Literature Review. University of Applied and Environmental Sciences U.D.C.A.
- Garcia S, Gonzalez J, Sanz I, Garcia E, Alvaro F, et al. (2017) Complications associated with negative pressure therapy in the treatment of diabetic foot ulcers: retrospective case series. Spanish journal of podiatry.
- Sarabia C, Castanedo C (2014) What is negative topical pressure? Is it effective/efficient in closing complex wounds? Topic review. Gerokomos 25(1): 44-47.
- Espinosa C, Abad E, Termens J, Gonzalez L, Arnés A, et al. (2011) Negative pressure therapy and podiatry. The Peu 31(3): 112-123.
- Calixto L, Villegas M (2013) Application of topical negative pressure systems in wounds and coverage defects in traumatized limbs. Rev Col or Tra 27(1): 48-55.
- Buendía J, Vila A, Gómez R, Qiu S, Marré D, et al. (2011) Treatment of complex wounds with negative pressure therapy. Experience in the last 6 years at the University Clinic of Navarra, Pamplona (Spain). Cir.plást. iberolatinoam 37(1): S65-S71.

 Review Article
Review Article