ABSTRACT
Background: The intensive care unit or also known as critical care unit is a specific place where multidisciplinary care is provided to maintain the vital functions of patients at risk.
Methodology: A bibliographic review was carried out through various databases from 2017 to 2022; The search and selection of articles was carried out in indexed journals in English and Spanish. The following keywords were used: humanization, ICU, medicine, care.
Results: the implementation of good strategies has made the intensive care unit a place with a comprehensive and pleasant environment for both the patient and her relatives, which greatly helps her physical recovery.
Conclusion: humanized care from health professionals makes a big difference in all possible aspects, so much so that the patient will have better communication with the staff, better adherence to pharmacological treatment, better emotional and mental state.
Keywords: Humanization; ICU; Medicine; Care
Introduction
It should be noted in the intensive care unit individualized attention is provided to each of the patients who have a critical state, therefore, it is unique and different, where many times we concentrate so much on the treatment that we leave aside the human aspect, at present, this unit is in many changes both in the structural and organizational field, to cover all the needs of both families and patients [1]. The need to humanize intensive care arises in many areas, both for the health professional and for the patient, since we all have interpersonal relationships, and not only in this field, but in many other areas of health. In the hospital field is where the most delicate situation occurs, since vulnerability and suffering are almost inherent in the process of getting sick. The changes in health in recent years have generated numerous debates related to humanization in the care of the sick person, due to therapeutic approaches, education, and our responsibilities to all for patients equally, makes us act systematically, without taking into account that, we are attending to a human being, with a family concerned not only about their physical well-being but also about their emotional and psychological well-being [2]. Improving the relationship of professional to patients, will help us to have better communication with them in the critical environment, improving both the care, comfort and well-being of the patient, generating a fraternal alliance with the person, their relatives, and ways of life, without exceeding the ethical limits of the patient’s autonomy, but showing our humanity with the aim of improving the patient’s instance in intensive care. This article aims to show the other side of medicine in an area of high importance such as the intensive care unit (ICU), showing that health professionals not only fulfill the clinical function, but also the emotional part of the patients who are hospitalized.
Materials and Methods
A literature review was carried out, in which we searched the databases of the Journal of Medical-Surgical Specialties, Elsevier, and ScienceDirect, among others. The collection and selection of articles was carried out in journals indexed in English language from the years 2017 to 2022. As keywords, the terms were used in the databases according to the DeCS and MeSH methodology, humanization, ICU, medicine, care. In this review, 90 original and review publications related to the subject studied were identified, of which 23 articles met the specified inclusion requirements, such as articles that were in a range not less than 2017, that were fulltext articles and that reported on the humanization of intensive care: the other side of medicine. As exclusion criteria, it was taken into account that the articles did not have sufficient information and that they did not present the full text at the time of their review.
Results and Discussion
Intensive Care Unit (ICU)
The intensive care unit or also with occida as a critical care unit is a specific place where multidisciplinary care is provided which is composed of a team where there are, intensivist doctors, nurses, stretcher bearers, therapists among others, these meet functional, organizational and structural requirements so that the conditions of safety, efficiency and quality in the care of patients who are going through a moment of vulnerability in their recovery, which require specialized care, can be guaranteed [3]. Many times these patients are not stable, or need oxygen support, prone to multi-organ failure. The intensive care unit has done an impressive job since its creation, thanks to the development of the specialty and technology, greatly lowering mortality levels, and today patients admitted to these units have much more chances of recovering comprehensively [4]. However, because of how these units are structured, they tend to generate a lot of lack of attention to the fear that these patients and their families have of suffering, this is because the professionals are educated in a biomedical standard, where only the diagnosis and treatment are the main objective, which generates the technification leaving the non-pathological human needs in the background of both the patient and their families. In the intensive care unit (ICU) are those patients who require constant care and specialized care or 24 hours a day because their condition is critical. It is a sector in which specialized and educated professionals work to give due care to patients [5].
That is why it is very important to implement good strategies since, the patient is the essential element in their own recovery, implement participation in case the patient can, add participation in their own care, among other activities that can be carried out within the intensive care unit to stimulate the factors that improve their state of health and well-being. As mentioned above, the intensive care unit is a very delicate place where patients in a very critical state are cared for, due to these characteristics it is or becomes a source of stress and frustration, not only for the patient but also for the professions that develop in this area. The origin of these feelings is the frequent exposure one has to fear, pain and death, not knowing what will happen and the constant concern for the future [6]. When we talk about humanization we do not refer to an ideology, but to an alliance with the patient and his way of life, we look for aspects in quality and ethical commitment, respecting the autonomy of the patient in all areas, to achieve the objective of humanizing the intensive care unit we must implement values such as respect, understanding learning that each person is unique and respond differently when a life crisis occurs [7]. Therefore, it is very important to barar both care, ethical, cultural, communicative areas, to create an environment of human warmth, seeking improvements in the well-being of patients. For all this, it is necessary to integrate the human sciences into the training of health professionals.
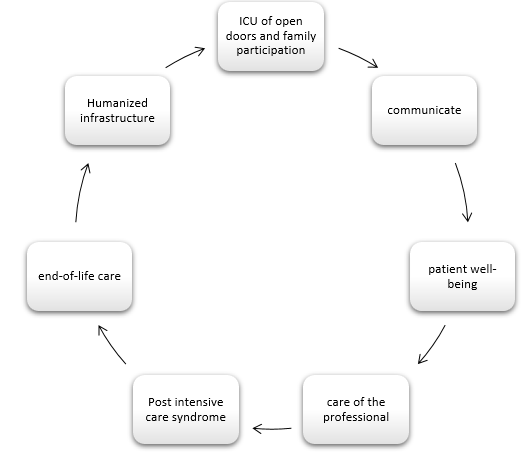
Open-Door ICU
Like everything, this unit is not free of changes, so in 2014 a HUCI project was launched, with innovative strategies, such as opendoor ICUs and participation of family members in patient care [8]. In the medical literature, many cases have been found in which the benefits of the ICU have been demonstrated at open doors, where greater satisfaction of the patient and family members is indicated regardless of their pathology, as well as of the health personnel (Figure 1). The objective of the open-door ICU is to reduce or eliminate in its entirety all the limitations imposed in three dimensions: temporal, contact, and relationship [9]. It is important to keep in mind that when it comes to a functional family, it acts as the same unit, in which, if any is affected, the rest of the family will also feel affected, which is why the health-disease process of any of the members of the family must be taken care of together with the patient [10]. This implementation of the family is very beneficial for the recovery of the patient, and for the health personnel this alliance is very positive, but at the same time it supposes a greater workload which could have an impact on the care of the patient.
Positive Effects on Patients
The advantages that have been developed thanks to the humanization of the intensive care unit are described in several aspects, such as physiological, mental, and emotional, thus reducing stress and giving greater satisfaction to patients and family members [11]. With the presence of the family member, pain management can be better distinguished and optimized, reducing the presence of complications during their stay in the intensive care unit, anxiety symptoms are also minimized, as well as the presence of delusions. Recently, other emotional and cognitive problems have been specified together, whether chronic or acute, such as depression and the development of post-intensive care syndrome, in nurses who remained unaccompanied [12]. The patient decides whether or not he wants company, since being in a critical state can generate the loss of identity and autonomy, this results in feelings of loneliness and not wanting any close person to see him in that state, generating physiological, mental and emotional alterations, given by isolation, the environment where he is and the care received by health professionals, which tends to be very limited, without assertive communication, but with a technical language forgetting the human part of that patient [13].
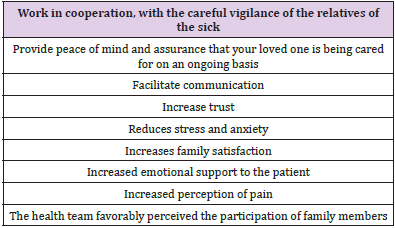
Positive Effects on the Family
Currently, ICU visits have been somewhat restricted with the belief that companions are a threat to patients as they increase the possibility of infections and increased stress. But the total opposite of this has been shown in the intensive care unit at open doors, in the Table 1 below we will show the advantages that this produces.
Positive Effect on the Health Team
An improvement of human relations within the hospital especially within the intensive care unit show great benefits such as the recognition of good work, the good interaction of the intensivist team with the patient and family members, this ensures that nursing care can be provided in a comprehensive, continuous, and safe way, thus achieving well-being and confidence [14]. On the other hand, this has a positive effect for intensive care staff by modifying the model of care through improved communication, greater patient care, greater approach, and support to the family, and favors multidisciplinary work [15].
ICU before and During the Pandemic
As we well know, during the time of 2019 and 2020, a global pandemic was triggered by the SARS-CoV-2 coronavirus, this disease produces as the most serious presentation an acute respiratory stress syndrome, with low oxygenation, which in most cases required hospitalization in Intensive Care, since it requires mechanical ventilation and specialized care [16]. This is and was an emergency at regional level, where both human and input resources generated a problem where a health plan had to be structured. The beds of Intensive Care Units were resources to face the pandemic, which required many dynamic modifications in daily work, where all the capacity, quality and skill had to be available, making a significant increase in daily work in the different sectors of the health system especially in the intensive care unit. Given the situation brought by the pandemic, new protocols had to be complied with where each patient had to be at an established distance in order to protect the integral of each one and avoid getting infected, these changes added greater isolation for those who were hospitalized in the intensive care unit, less communication between health personnel workers and patients, generated an almost total restriction to the visits of the patients’ friends, this generated a negative impact on the emotional and mental health of ICU patients, seeking to prevent or avoid the greatest amount of contagious [17].
Discussion
An article by C. de la Fuente-Martos at el, which is called “Implementation of a humanization project in an Intensive Care Unit” is a humanization project in the Intensive Care Unit (ICU) of the Infanta Margarita Hospital, the project, with a duration of 1 year “12 months for 12 commitments”, which aims to engage all ICU professionals, both medical, nursing and auxiliary staff, with exceptional involvement and commitment to patients, where for a year they carried out outreach and humanization activities within the intensive care unit [18]. Great results were obtained, and they say that the experience was very rewarding. Where they realized the way of life of the patients and their families that made them more aware of the feelings, needs and shortcomings than those that these families have experienced, during such an intense experience. Ensure to continue with these activities in the future [19]. Another article, by Danilo Moreno entitled “Open door ICU as a strategy for the humanization of care. Bibliographic review” describes the reality of what happens within the ICU, all the stress and anxiety that inpatients generate, but with the implementation of the opendoor ICU strategy, it contributes to the humanization of care in these units, since it allows family-patient interaction and health team providing mutual benefits in the care process [20].
Although a study was conducted that reported the dissatisfaction of health workers to open intensive care doors where the following results were obtained: it was found that 87.5% thought that the open visit would be of little benefit to ICU staff and that it puts patients who have a critical condition at risk, while 71.9% of the professional team in the intensive care unit consider that the open visit may have a beneficial or very beneficial effect on the patient, 62.5% considered the effect on the family as potentially beneficial or very beneficial. In short, no significant negative aspects were found related to the continuous accompaniment of family members to the patient in critical care, on the contrary, it helps the recovery faster and in more pleasant ways for the patient [21]. A strength of the current study is the methodology implemented, with respect to literature search, and steps in the selection of relevant articles, quality assessment and data extraction. However, this study has several limitations, which should be taken into account before reaching a conclusion, within these are the little evidence of clinical studies that demonstrate the humanization of intensive care: the other side of medicine.
Conclusion
How we can observe thanks to the information collected the humanization of the intensive care unit is possible, and can be done in many ways, all to help the early recovery of the critical patient. The most used strategy and with many benefits is the open doors of ICU, but, as well as these, there are much as that will help us to have a less systematized communication with patients and their families, the objective is to demonstrate that the medical staff is not only to diagnose or plan an adequate treatment plan, but also to accompany our patient in all existing areas, outside and inside medicine [22]. It has been proven that humanized care by health professionals makes a great difference in all possible aspects, so much so that the patient will have better communication with the staff, better adherence to pharmacological treatment, better emotional and mental state, both the patient and the family, and the person in the intensive care unit, they will have better results and will generate an integral environment for all ICU patients [23].
References
- Correa DAM (2021) The bidirectional sense of humanization, a perspective from physiotherapy.
- Quispe L, Raysa J (2021) The bidirectional sense of humanization, a perspective from physiotherapy.
- Duque-Ortiz C, Arias-Valencia MM (2021) Nurse-family relationship in the intensive care unit. Towards an empathetic understanding. Journal of Health Sciences 19(1): 124-143.
- González-Gil MT, Alcolea-Cosín MT, Pérez-García S, Luna-Castaño P, Torrent-Vela S, et al. (2021) The children's visit to the pediatric intensive care unit from the experience of the nurses. Intensive Nursing 32(3): 133-144.
- Alarcón MM, Sancho JM, Carbonell AP, Guirao VN, Latour MA, et al. (2022) Result of the implementation of a quality management system based on ISO 9001: 2015 in a surgical intensive care unit. Spanish Journal of Anesthesiology and Resuscitation.
- Zaragüeta Martín U (2020) Humanization in ICU: Integration of the family.
- Ayerdi Belza I (2021) Influence of music in an intensive care unit.
- Aguilar B, Faridey M (2021) Therapeutic nursing communication perceived by the family member of the patient hospitalized in the pediatric intensive care unit of a national hospital in Lima.
- Pérez-San Román MA, Cante-Hernández D, Huichin-Pool MA, Fuentes-Fernández E (2020) Critical unit adults with open doors: Nursing experiences in a public hospital in Quintana Roo. Salud Quintana Roo 11(38): 17-21.
- Martínez Zubieta R (2021) Humanization in the Intensive Care Unit. Critical Medicine (Mexican College of Critical Medicine) 35(3): 144-147.
- Zubieta RM. Humanization in the Intensive Care Unit.
- Regaira-Martinez E, Garcia-Vivar C (2021) The process of informing family members in intensive care units: a narrative review. Intensive Nursing 32(1): 18-36.
- Castro Perdomo PE, Durán Marín AL, Hernández García JS (2020) Strategies for the improvement of humanized care standards for patients in intensive care units due to Covid-19.
- Saad Y. Intensive care units before and after COVID-19. From narrative medicine to humanized care, 93.
- Duque-Ortiz C, Arias-Valencia MM (2020) Nurse-family relationship. Beyond the opening of doors and schedules. Intensive Nursing 31(4): 192-202.
- Castro L, Luz D (2020) Educational program on the knowledge and attitudes of humanized care of nursing professionals in the Intensive Care Unit of a pediatric hospital Lima.
- Rivera de Castillo BM (2020) Humanized nursing care and patient satisfaction in the maternal intensive care unit. Bethlehem Hospital.
- Álvarez Díaz R (2021) Demystifying the vision of the intensive care unit: perception and reality in patients and citizens.
- Cedeño JA (2021) Humaniza-te: For Care in times of pandemic.
- Huaynate Canorio RB (2020) Nursing care for patients at the end of life in an Intensive Care Unit.
- Álvarez Maita RA (2020) Perception of the family member about assertive communication and emotional support provided by the Nursing professional in the Intensive Care Unit of a pediatric hospital in Lima.
- Macías Ventureira R (2020) Needs of families and humanizing strategies in intensive care units.
- Ochoa KT, López CM, Guzmán-Romero SY, Ruíz, DPG, Zambrano SMH (2020) Coping strategies in relatives of critically ill patients. Journal repertoire of Medicine and Surgery, p.1-8.

 Research Article
Research Article