Abstract
We encountered a patient with orbital floor fracture in whom bone transplantation from the left ilium was performed but left iliac fracture at the site of collection occurred 2 years after surgery. In this patient, bone-collection-related iliac bone defect had been present. In this study, we conducted mechanical analysis using the finite element method (FEM) to investigate the load on the ilium before fracture in this patient. The results showed that the risk of fracture had been high. In addition, a bone defect model was prepared based on the iliac data from healthy adults, and mechanical analysis with the FEM was also conducted to clarify the mechanism of ilium fracture on exercise loading. As a result, it was shown that the risk of ilium fracture was higher when the site of ilium collection was more posterior. Usually, anterior ilium collection has been recommended to prevent complications. Our study also supported that the risk of fracture decreases with anterior ilium collection.
Keywords: Bone Grafting; Iliac Bone; Pain; Autologous Bone Graft; Bone Harvesting; Finite Element Method; Fatigue Fracture; Iliac Crest
Abbreviations: ASIS: Anterior Superior Iliac Spine; PT: Pubic Tubercle; SJ: Sacroiliac Joint; AC: Acetabulum; IC: Iliac Crest
Introduction
For autogenous bone transplantation in the field of craniomaxillo- facial surgery, the ilium, in which the degree of freedom is relatively high, is selected as a donor in many cases. On the other hand, postoperative pain after ilium collection persists for a long period in some patients, often raising the issue of activities of daily living reduction. We encountered a patient in whom reconstructive surgery for orbital floor fracture was performed in our institution, and left iliac pain related to exercise appeared 2 years after surgery. In this patient, a bone graft had been collected from the left ilium, and computed tomography (CT) after the appearance of pain revealed fracture of the left ilium. In the present case, bone collection resulted in a bone defect, and we cannot deny that the structure was more fragile than on the unaffected side. To clarify an etiological factor for the fracture mechanism, we conducted mechanical analysis with the FEM.
Materials and Methods
We investigated the ilium of a 38-year-old female (Case 1)
with left iliac fracture after collection of a left iliac bone graft, as
well as the left ilium of a healthy 67-year-old female (Case 2). Three-dimensional (3D) models of the respective left iliac bones
were prepared from the DICOM data on CT. We conducted FEM
analysis of the ilium under mechanical loading using a personal
computer (PC) and FEM software, MECHANICAL FINDER version
11.0 (Research Center of Computational Mechanics, Inc., Tokyo).
Constraint conditions for FEM analysis were established as the
sacroiliac joint surface, pubic symphysis, and acetabular fossa. As
loading conditions for FEM analysis, vertical loads for the wing of
the ilium and acetabular fossa were established as 1,800 and 1,200
N, respectively, assuming the state of landing on exercise (Figure 1).
i. In Case 1, FEM analysis was conducted using postoperative CT
findings before fracture.
ii. In Case 2, three kinds of model, anterior, middle, and posterior
iliac bone defect models after ilium collection,
were prepared on a PC, and FEM analysis under mechanical
loading was conducted. Concerning the degree of bone destruction,
the solid numbers for compression failure (complete), compression
failure (plasticity), and tensile failure on each element were
calculated using FEM analysis and used as a parameter of the risk
of fracture.
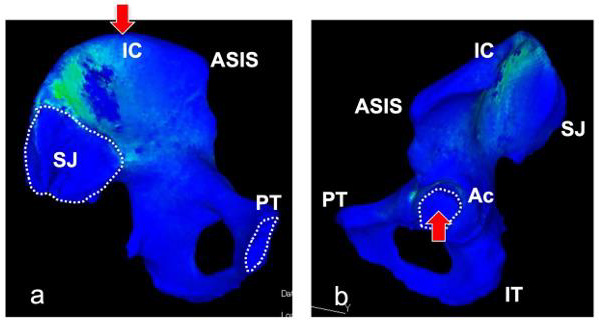
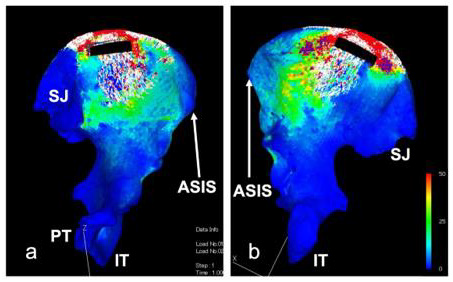
Figure 1: 3D-CT of the left ilium of a healthy adult (a: medial view, b: lateral view):
Model simulation was conducted, assuming landing on exercise.
Loading and constraint conditions in the finite element method were established as follows:
• Loading conditions (red arrow): IC, 1,800 N from the cephalic side; Ac, 1,200 N from the caudal side
• Constraint conditions (within white dotted lines): 3 points (PT, SJ (a), and Ac (b)).
Results
Case 1
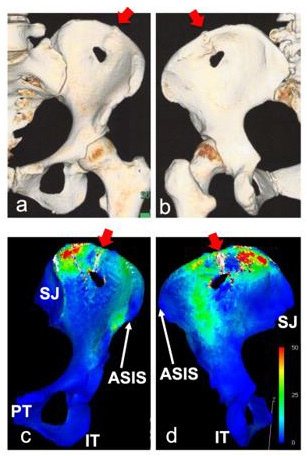
All-layer bone grafts were collected from the left ilium. CT two years after surgery revealed fracture at the iliac crest (Figures 2a & 2b). Before fracture, CT had been performed for follow-up 1 year after surgery. However, there was no fracture at that time. FEM analysis was conducted using CT findings in the absence of fracture. The results showed that compression failure (complete, red, solid number: 542), compression failure (plasticity, yellow, 221), and tensile failure (white, 339) had occurred Figures 2c & 2d, total number of destroyed solids: 1,102). Thus, iliac destruction may have been predicted 1 year after surgery.
Case 2
In the healthy ilium, posterior, middle, and anterior bone defect models were prepared, and finite element analysis was conducted for each. Anterior bone defect model (Figure 3): The total number of destroyed solids was 1,204 (compression failure (complete): red:649, compression failure (plasticity): yellow:372, and tensile failure: white:183). Middle bone defect model (Figure 4): The total number of destroyed solids was 2,185 (compression failure (complete): red:1025, compression failure (plasticity): yellow:537, and tensile failure: white:623). Posterior bone defect model (Figure 5): The total number of destroyed solids was 6,936 (compression failure (complete): red:3,445, compression failure (plasticity): yellow:564, and tensile failure: white: 2,927).
Figure 2: Bone graft were harvested from the left iliac crest in all layers. Red arrows showed fracture at the iliac crest (Figure 2-a, b, CT at 2 years postoperatively). There was no fracture on CT one year after surgery, but FEM analysis showed that stress had been dispersed in the anterior and posterior areas of the ilium on landing during exercise (Figures 2-c and 2-d, green range). In addition, FEM analysis indicated that the iliac crest to bone defect site were loaded at a degree at which bone destruction was observed (refer to bone destruction, red arrows, in Figures 2-c and 2-d).
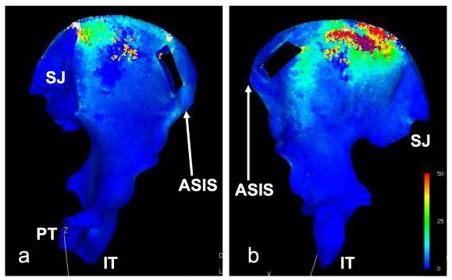
Figure 3: 3D-CT of the left ilium of a healthy adult (a: medial view, b: lateral view):
Anterior bone defect model (Figure 3): The total number of destroyed solids was 1,204 (compression failure (complete): red:649,
compression failure (plasticity): yellow:372, and tensile failure: white:183).
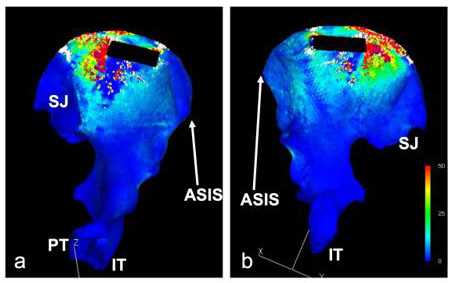
Figure 4: 3D-CT of the left ilium of a healthy adult (a: medial view, b: lateral view):
Middle bone defect model (Figure 4): The total number of destroyed solids was 2,185 (compression failure (complete): red:1,025,
compression failure (plasticity): yellow: 537, and tensile failure: white: 623).
Figure 5: 3D-CT of the left ilium of a healthy adult (a: medial view, b: lateral view): Posterior bone defect model (Figure 5): The total number of destroyed solids was 6,936 (compression failure (complete): red:3,445, compression failure (plasticity): yellow:564, and tensile failure: white:2,927).
Discussion
Iliac donor-site complications include pain, neurovascular injury, avulsion fractures of the ASIS, hematoma, infection, herniation of abdominal contents, gait disturbance, cosmetic deformity, violation of the sacroiliac joint, and ureteral injury [1]. The most common complication of posterior iliac crest bone graft harvesting is postoperative pain at the donor site [2]. Banwart et al. reported that mild complications, such as persistent pain, were noted in 39% of patients after ilium collection, and that serious complications occurred in 10% [3]. Furthermore, Goulet et al. indicated that pain at the donor site appeared 6 months after surgery in 37.9% of patients and 2 years after surgery in 18.4% [4]. We have also often encountered patients complaining of pain after ilium collection. In particular, many patients complained of pain under loading. In Case 1, there was no fracture on CT one year after surgery, but FEM analysis showed that stress had been dispersed in the anterior and posterior areas of the ilium on landing during exercise (Figures 2c & 2d, green range). In addition, FEM analysis indicated that the iliac crest to bone defect site were loaded at a degree at which bone destruction was observed (refer to bone destruction in Figures 2c & 2d). In the present case, fracture occurred 2 years after surgery. This may be correlated with iliac strain on exercise. A study reported that the incidences of donor-site pain and postoperative complications after bone transplantation with the Trapdoor-procedure were low, and that the volume of intraoperative blood loss was small [5]. In this study, we examined all-layer bone defect models, as demonstrated in Case 1.
In this study, we prepared 3 iliac bone defect models using the healthy ilium to clarify the position of ilium collection at which the risk of fracture is low. The results of FEM analysis suggested that the risk of fracture is the highest when an iliac bone defect is present in the posterior area (total number of destroyed solids: 6,936), followed by the middle and anterior areas (2,185 and 1,204, respectively). In particular, when preparing a bone defect in the posterior area, the risk of extensive bone destruction on the caudal side of the bone defect site is high in addition to fracture at the iliac crest; more serious ilium fracture was predicted (Figure 5). Based on these results, it is recommended that a bone graft should be collected from a more anterior iliac area. To reduce the risk of these complications, it is recommended that the site of collection from the anterior superior iliac crest should be established as ≥3 cm posterior to the anterior superior iliac spine [6,7]. Furthermore, a study indicated that fracture was more frequent after all-layer bone collection than after divided-layer bone collection [1]. Previous studies suggest that a bone graft should be collected from the anterior area of the ilium. However, it is described that attention must be paid. A harvest site located at least 20 to 25 mm posterior to the anterior superior iliac spine ASIS should be preferred to minimize the risk of iliac fatigue fracture [8]. And a tricortical graft from the anterior ilium should be taken at least 3 cm posterior to the ASIS [1]. Thus, bone collection from the posterior area of the ilium, which may induce complications, should be avoided, and the results of FEM analysis also support the significance of collecting a bone graft at the most anterior position while maintaining 3cm from the anterior superior iliac spine. To avoid persistent loads on the site of ilium collection or additional fracture, this study may be useful, clinically contributing to a decrease in the incidence of postoperative complications. As an issue regarding this study, FEM analysis in consideration of the muscle groups involved in the ilium may be necessary in the future, as fracture at the iliac crest after ilium collection may be associated with the strong contractility of the sartorius muscle or tensor fasciae latae muscle as a background factor [9].
Conclusion
Focusing on mechanical changes in the ilium with a bone defect after graft collection, we conducted finite element analysis regarding differences in the distribution of stress from the healthy ilium and examined factors for fracture. When collecting the ilium, anterior collection may reduce the risk of fracture due to structural mechanical reasons on the ilium.
Financial Disclosure Statement
No funding was received for this article.
The authors have no conflicts of interest directly relevant to the
content of this article.
Conflicts of Interest
The authors declare no conflict of interest.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
References
- Ebraheim NA, Elgafy H, Xu R (2001) Bone-graft harvesting from iliac and fibular donor sites: techniques and complications. J Am Acad Orthop Surg 9(3): 210-218.
- Delawi D, Dhert WJ, Castelein RM, Verbout AJ, Oner FC, et al. (2007) The incidence of donor site pain after bone graft harvesting from the posterior iliac crest may be overestimated: a study on spine fracture patients. Spine 32(17): 1865-1868.
- Banwart JC, Asher MA, Hassanein RS (1995) Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine (Phila Pa 1976) 20(9): 1055-1060.
- Goulet JA, Senunas LE, DeSilva GL, Greenfield ML (1997) Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res 339: 76-81.
- Zhu JF, Xu WX, Hu Q, Wu TQ, Liu H, et al. (2020) Iliac Bone Harvesting Techniques for Bone Reconstruction. Comparative Study Between Tricortical Bone Harvesting vs Trapdoor Technique. Ther Clin Risk Manag 16: 559-565.
- Younger EM, Chapman MW (2018) Morbidity at bone graft donor sites. J Orthop Trauma 3(3): 192-195.
- Meeder PJ, Eggers C (1994) Techniques for obtaining autogenous bone graft. Injury 25: A5-16.
- Schmitz P, Cornelius Neumann C, Neumann C, Nerlich M, Dendorfer S J, et al. (2018) Biomechanical analysis of iliac crest loading following cortico-cancellous bone harvesting. Orthop Surg Res 13(1): 108.
- Myeroff C, Archdeacon M (2011) Autogenous Bone Graft: Donor Sites and Techniques. J Bone Joint Surg Am 93(23): 2227-2236.

 Case Report
Case Report