Abstract
Oral mucosal pathologies have varied presentations, and their innocuous appearance can occasionally misguide even the specialist. Various oral diseases can be detected by sampling the mucosa. The biopsy is a process of removing an altered viable tissue from a living being to determine the nature of pathology by microscopic evaluation. This approach allows for confirmation of the histopathologic features of suspicious pathologies, their grade and stage, and an appropriate treatment plan. The biopsy is a primary diagnostic test for a range of oral lesions. It is required for those oral mucosal surfaces which demonstrate significant and tenacious changes in the colour or appearance. Although an array of biopsy techniques and tools exist, the utmost intention is to pick up a representative tissue that will aid in preparing an explicit histopathology report. We present a case of a suture thread incisional biopsy (IB) technique performed on a 32-year-old patient with an oral white lesion that resulted in a successful sample for histopathology. The sample taken provided flawless sections with precise histopathological features. This report illustrates a modified IB sampling technique and its utility. The suture thread IB technique was found to have many advantages over conventional IB techniques. However, the procedure needs highly skilled clinicians to perform it. Future investigations could elaborate on the merits and demerits of this technique.
Keywords: Oral Biopsy; Diagnosis; Incisional Biopsy; Histopathology; Surgical Technique; Suture Thread Biopsy
Introduction
Biopsy of oral tissues is mandatory for the pathologies that cannot be diagnosed solely based on history and clinical oral examination (COE) [1]. In routine practice, most biopsies are from the oral mucosa. They are undertaken not only for suspected oral premalignant lesions (OPLs) but also for the diagnosis of vesiculobullous, chronic ulcerative, and desquamative lesions of the oral mucosa [2]. A biopsy is defined as “the removal of tissue from the living organism for microscopic examination and diagnosis” [3]. The word biopsy is derived from the two root Greek words, “bios” (life) and “opsis” (vision). Practically, the biopsy is a process of extracting a tissue specimen from a living being to examine it under a microscope with a diagnostic intent [4]. It is an investigative technique that is considered the gold standard for diagnosing most diseases [3,5]. Histopathological assessment of tissue gives information regarding the clinical behaviour of the disease and prognosis apart from being a gold standard for diagnosing several pathologies [6]. The biopsy report can aid the clinician in determining the course and predicting recovery, recurrences, or progression of pathology [4]. The rationale for carrying out a biopsy is as follows: to confirm a definitive diagnosis quickly so that appropriate treatment can begin, to assess the prognosis in malignant and OPLs, to ascertain whether a lesion has been entirely excised and if the histopathology report is a document with medicolegal importance [7,8].
According to the American Academy of Oral and Maxillofacial Pathology, any altered tissue removed from the oral and maxillofacial region should be subjected to histopathologic examination [9,10]. Pathologies such as a swelling, red or white patch or ulcer that does not heal within three weeks, malignancy, or any other chronic condition must be ruled out by a biopsy procedure [11]. The sample procured with oral biopsy techniques is usually small, and the chance for the artefact is higher [9]. Representative biopsy of an oral mucosal disease must encompass the full epithelial thickness with some supporting connective tissue, not only to evaluate invasion but also to provide physical support for the specimen [5,12]. A satisfactory and suitable tissue sample is critical when obtaining a biopsy [10]. A good biopsy ideally contains tissue that is indicative of the notable change in the lesion and is apt for pathologic evaluation [13]. Biopsies should be about 10 x 5 x 5 mm in size. The ideal shape of a mucosal biopsy is either elliptical or round, as either shape gives a sufficient volume of tissue [13]. Multiple biopsy specimens may be necessary if the disease is substantial or exhibits a diverse clinical picture [5]. Precise identification of oral lesions is dependent upon the biopsy quality, relevant clinical details and accurate interpretation of the report [13].
On the basis of the distinctive attributes of the specific lesion, a biopsy is labeled as direct (superficial, accessible) or indirect (deep and hardly accessible). Biopsies can also be classified based on the techniques, tools employed, timing, location of the lesion, sample processing, and intent. Depending on the working technique, biopsies can be classified as incisional biopsy (IB) or excisional biopsy (EB) [14]. The location, size, and form of the lesion dictate the decision to perform an IB or EB [15]. Most of the oral mucosal biopsies are IBs [16]. IB demands the removal of a representative wedge of the lesion in question and a portion of healthy mucosa [14,15]. IB is a reliable diagnostic approach for oral lesions [17]. Based on tools employed for biopsy, the scalpel and punch biopsy techniques are recommended for the oral cavity proper [18]. Scalpel biopsy is the frequently used mode that usually gives satisfactory samples from both incisional and excisional procedures [5]. A detailed history and COE are essential in preparing a provisional or differential diagnosis which will specify the type of biopsy to be done [2]. The sampling problem needs to be addressed for all IBs, and when required, biopsy techniques are modified to enable a more appropriate sampling. Adequate size and depth of tissue sample will better the agreement and reveal the salient diagnostic features [17]. A focused surgical procedure will reduce the tissue artefacts, which can hamper pathological diagnosis or even make the sample non-diagnostic [16]. Regardless of the method employed, the purpose is to provide a satisfactory representative specimen for the histopathologist to report, in the interim reducing patients’ perioperative distress. This paper presents a case in which effective IB was done by a suture thread biopsy technique which is an alternative or modification to the traditional scalpel biopsy or conventional IB.
Case Report
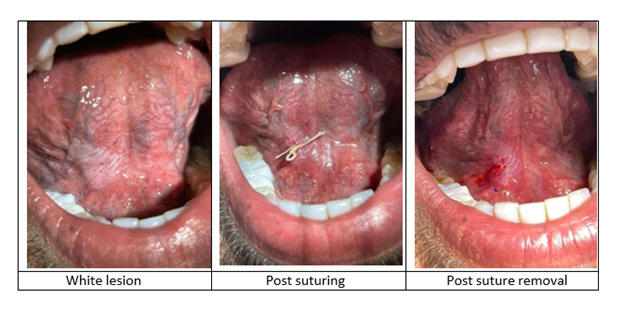
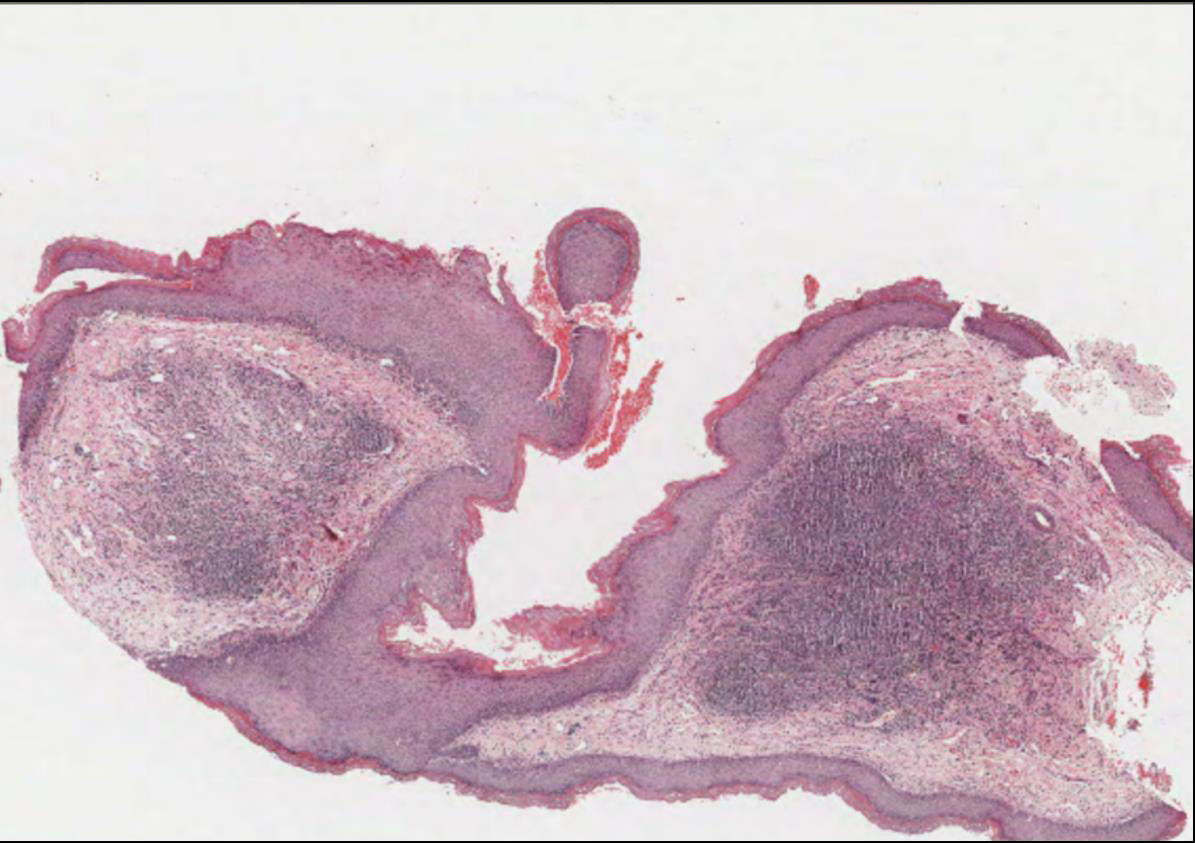
A 32-year-old male reported to the outpatient dental clinic with the chief complaint of the appearance of painless white patches under his tongue. The patient had discovered the patch 3 months before his visit. Complete oral examination showed a 2 cm × 2 cm, non- scrapable white lesion on the ventral surface of the tongue. An IB was performed to confirm the provisional diagnosis of oral leukoplakia (OL). Verbal and written informed consent were obtained before the procedure. The surgical details were discussed with the patient, as well as potential complications. Local anesthesia of mepivacaine 2% combined with epinephrine (1:100 000) was injected around the biopsy site. After this, a special technique using a suture needle and thread was inserted at a 90-degree angle along the tissue surface, followed by pulling the grasped tissue with the thread and cutting it with a size 15 scalpel blade. Hemostasis was achieved with single interrupted sutures. Postoperative healing was uneventful (Figure 1). Gross examination revealed a tiny wedge of oral mucosa with a whitish surface and yellowish base measuring approximately 4×3×2mm. Microscopic examination of the altered mucosa showed a stretch of stratified squamous epithelium and the supporting connective tissue. The epithelium showed variable thickness, mostly thin, with prominent stratum granulosum and corrugated hyperkeratosis. In addition, the epithelium showed mild dysplastic change with a focal area of moderate dysplasia. Basal cell hyperplasia, loss of polarity, increased Nuclear: Cytoplasmic ratio, hyperchromatic nuclei and pleomorphism were noted at focal areas. The dysplastic changes were confined to the lower third of the epithelium. Cytologic and architectural changes were confined to the lower third of the thickness of the epithelium. The rete ridges were inconspicuous with flat epithelial and connective tissue interface. The superficial lamina propria was infiltrated by a dense band of lymphocytes. The submucosa was composed of fatty tissue, vasculature and focal aggregates of lymphocytes. The final diagnosis was leukoplakia with mild dysplasia. The patient was put on close follow-up protocol (Figure 2).
References
- Lauren L Patton, Joel B Epstein, A Ross Kerr (2008) Adjunctive techniques for oral cancer examination and lesion diagnosis: a systematic review of the literature. J Am Dent Assoc 139(7): 896-905.
- DJ Finn, BP Rajlawat, DJ Holt, SRL Adair, K Kent, et al. (2017) Field EJBDJ: The development and implementation of a biopsy safety strategy for oral medicine. Br Dent J 223(9): 667-673.
- Bernstein ML (1978) Biopsy technique: the pathological considerations. J Am Dent Assoc 96(3): 438-443.
- Massoumeh Zargaran (2014) A review of biopsy in dentistry: Principles, techniques, and considerations. JDMT 3(2): 47-54.
- Sylvie-Louise Avon, Hagen BE Klieb (2012) Oral soft-tissue biopsy: an overview. J Can Dent Assoc 78: c75.
- Kar S, Prasant M, Saraf K, Patil K (2014) Oral biopsy: Techniques and their importance. JAJAMS 2(3).
- Ali FM, Prasant M, Patil A, Ahere V, Tahasildar S, et al. (2012) Oral biopsy in general dental practice: a review. International Journal of Medicine and Public Health 2(1): 3-6.
- S P Khoo (1995) Oral biopsy in dental practice-The pathologist's perspective. Annals of Dentistry University of Malaya 2(1).
- KL Kumaraswamy, M Vidhya, Prasanna Kumar Rao, Archana Mukunda (2012) therapeutics: Oral biopsy: oral pathologist's perspective. J Cancer Res Ther 8(2): 192.
- Molly S Rosebush, K Mark Anderson, Swati Y Rawal, Harry H Mincer, Yeshwant B Rawal (2010) The oral biopsy: indications, techniques and special considerations. J Tenn Dent Assoc90(2): 17.
- Crispian Scully, José V Bagan, Colin Hopper, Joel B Epstein (2008) Oral cancer: current and future diagnostic techniques. Am J Dent 21(4): 199-209.
- KMK Masthan, S Leena Sankari, N Aravindha Babu, Jagadish P Rajguru (2013) How to help the oral pathologist in making an accurate diagnosis. J Clin Diagn Res 7(1): 181.
- Catherine F Poh, Samson Ng, Kenneth W Berean, P Michele Williams, Miriam P Rosin, et al. (2008) Biopsy and histopathologic diagnosis of oral premalignant and malignant lesions. J Can Dent Assoc 74(3): 283-288.
- Amparo Mota-Ramírez, Francisco Javier Silvestre, Juan Manuel Simó (2007) Patología Oral y Cirugía Bucal: Oral biopsy in dental practice. Med Oral Patol Oral Cir Bucal 12(7): 504-510.
- Davari P, Fazel N (2016) Practical pearls for oral procedures. Clin Dermatol 34(4): 440- 448.
- Oliver R, Sloan P, Pemberton MN (2004) Oral biopsies: methods and applications. Br Dent J 196(6): 329-333.
- Chen S, Forman M, Sadow PM, August M (2016) The Diagnostic Accuracy of Incisional Biopsy in the Oral Cavity. J Oral Maxillofac Surg 74(5): 959-964.
- Rabie M Shanti, Takako Tanaka, David C Stanton (2020) Oral biopsy techniques. Dermatol Clin 38(4): 421-427.
- Jain N (2011) surgery o: Essentials before sending biopsy specimens: A surgeon’s prespective and pathologists concern. J Maxillofac Oral Surg 10(4): 361-364.
- Epstein JB, Guneri P, Boyacioglu H, Abt E (2012) The limitations of the clinical oral examination in detecting dysplastic oral lesions and oral squamous cell carcinoma. J Am Dent Assoc 143(12): 1332-1342.
- Shravan Renapurkar B, Glass SH, Dean Luke (2019) Guidelines for biopsy of oral mucosal lesions.
- Kush J Patel, Harsha L De Silva, Darryl C Tong, Robert M Love (2011) Surgery M: Concordance between clinical and histopathologic diagnoses of oral mucosal lesions. J Oral Maxillofac Surg 69(1): 125-133.
- Michael S Forman, Sung-Kiang Chuang, Meredith August (2015) The accuracy of clinical diagnosis of oral lesions and patient-specific risk factors that affect diagnosis. J Oral Maxillofac Surg 73(10): 1932-1937.
- Goodson M, Kumar A, Thomson P (2011) P171 Oral precancer excision is required for definitive diagnosis: incisional vs excisional biopsies in oral leukoplakia management. Oral Oncology 1(47): S128-S129.
- Jang-Jaer Lee, Hsin-Chia Hung, Shih-Jung Cheng, Chun-Pin Chiang, Bu-Yuan Liu, et al. (2007) Oral Medicine, Oral Pathology, Oral Radiology, Endodontology: Factors associated with underdiagnosis from incisional biopsy of oral leukoplakic lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104(2): 217-225.
- M Pentenero, M Carrozzo, M Pagano, D Galliano, R Broccoletti, et al. (2003) Oral mucosal dysplastic lesions and early squamous cell carcinomas: underdiagnosis from incisional biopsy. Oral Dis 9(2): 68-72.
- Meghana S, Ahmedmujib BR (2007) Surgical artefacts in oral biopsy specimens: Punch biopsy compared to conventional scalpel biopsy. Journal of Oral and Maxillofacial Pathology 11(1): 11.
- Singh D, Bastian T, Singh A, Kudva S (2014) Oral Mucosal biopsy: Comparison of surgical artifacts in incisional and punch oral mucosal biopsy 14(1): 10.
- Seoane J, Varela‐Centelles P, Ramirez J, Romero M, De La Cruz (2002) Sciences A: Artefacts produced by suture traction during incisional biopsy of oral lesions. Clin Otolaryngol Allied Sci 27(6): 549-553.

 Case Report
Case Report