Abstract
Objective: Urinary tract infection (UTI) in children is a serious condition that should be treated promptly and properly to prevent further complications. The most common causative agent of UTI is Escherichia coli (E.coli). However, studies regarding the E.coli resistance patterns have not been comprehensive, and further research is required. This study aims to investigate the resistance profile of E.coli in pediatric cases of UTI.
Method: In this cross-sectional study, the positive cultures for E.coli in patients admitted in the Dr. Sheikh Children Hospital of Mashhad, Iran in Feb 2020 to Feb 2021 were assessed. The demographic factors including age and sex were excluded. Urinalysis was conducted to assess the number of bacteria (categorized as mild, moderate, and many) and the WBC count (categorized as > 5, > 10, and > 15). Furthermore, the antibiogram was consulted to assess the sensitivity and resistance to different antibiotics. Data were analyzed using SPSS software.
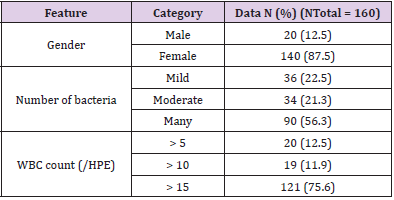
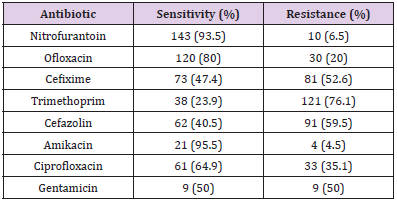
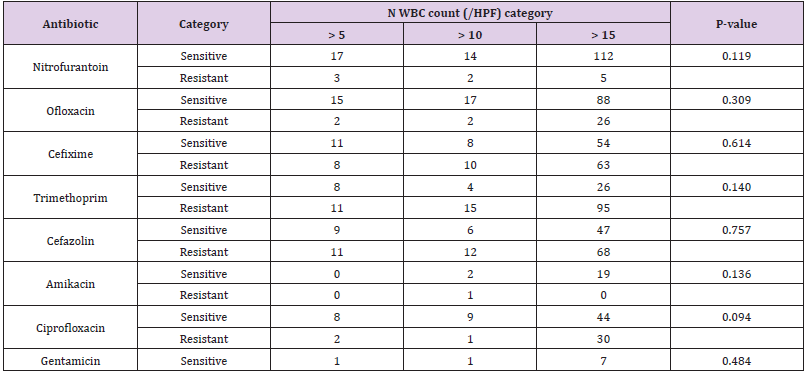
Results: In 160 children, 20 males and 140 females with the mean age of 24.00 ± 26.06 months, urinalysis showed that 22.5% were in the mild bacteriuria category, 21.3% in moderate bacteriuria, and 56.3% in the many bacteriuria category. For WBC count in urine, 12.5% had more than 5 WBC, 11.9% had more than 10 WBC, and 75.6% more than 15 WBC. Regarding resistance, 4.5% of the patients were resistant to amikacin, 6.5% to nitrofurantoin, 20% to ofloxacin, 35.1% to ciprofloxacin, 50% to gentamycin, 52.6% to cefixime, 59.5% to cefazolin, and 76.1% to trimethoprim. The mean age and also the frequency of sex showed no significant difference between different severities of bacteriuria and WBC count in urine analysis (P > 0.05). Besides, the age and sex distribution, and the number of bacteria and WBC count in urinalysis had no significant difference between the susceptible and resistant cases (P > 0.05).
Conclusion: The highest E.coli resistance was to trimethoprim, cefazolin, cefixime, gentamycin, and ciprofloxacin. The lowest resistance was to amikacin and nitrofurantoin. There was no significant difference regarding the age and gender and also different severities of pyuria and bacteriuria between the susceptible and resistant cases.
Keywords: E. Coli; Resistance; Antibiogram; Children; Urinary Tract Infection
Introduction
Urinary tract infection (UTI) is a common serious bacterial infection and one of the most common causes of febrile illness in children [1,2]. About 8% of girls and 2% of boys under the age of seven experience at least one episode of UTI, and recurrence occurs in 12% to 30% of them within a year [3]. UTI cases in children are often under-diagnosed due to the atypical clinical manifestations and various methods of collecting urine samples, especially in infants and young children [3], and it is estimated that about 50% of UTI occurrences in children are missed [4]. Early diagnosis and accurate treatment of the disease are essential to prevent longterm complications such as renal scarring, hypertension, and chronic renal failure [5]. Therefore, empirical antibiotics are often prescribed even before the results of the culture are obtained. On the other hand, antibiotic resistance is a growing universal problem that affects the ability to determine appropriate first-line methods for common urinary tract infections [6]. Escherichia coli (E. coli) is the most common bacterial pathogen responsible for urinary tract infections in children and accounts for more than 80 percent of cases [7]. An empiric therapy for affected children includes antimicrobial agents that provide coverage for that particular bacterium [1,8]. However, increased resistance to E. coli has led to fewer empirical antibiotic choices in recent years [1]. Understanding antibiotic resistance patterns helps to effectively select empiric antibiotics and reduce treatment failure. Ineffective empirical antibiotics may lead to increased morbidity, costs, long-term antibiotic treatment, and recurrence of the disease [9]. However, there are limited data on the antibiotic resistance patterns of children’s UTIs. The present study was conducted to determine the E. coli antibiotic resistance patterns in children with urinary tract infections.
Method
This cross-sectional study was performed on positive urinary cultures in children with urinary tract infections admitted in the Dr. Sheikh Hospital of Mashhad in 2020-2021. All positive urinary cultures in which E-coli was grown as the only pathogen and the colony count had more than 50,000 and had active urinary sediment were examined. Children with nephrology and urology pathologies, such as Foley catheter and nephrostomy, and who had a history of prolonged hospitalization, prolonged antibiotic consumption, or prophylaxis for UTI were excluded from the study. Demographic information such as age by month and sex were extracted. The urine analysis in these patients calculated the number of bacteria (categorized as mild, moderate, and many) as well as the WBC count (categorized as more than 5, more than 10, or more than 15). Also, the antibiogram was examined, and the antibiotic resistance and susceptibility of the organism were recorded. Finally, the data were statistically analyzed in SPSS software version 20.0.
Results
A total of 160 children were included in the study, of which 20 (12.5%) were boys and 140 (87.5%) were girls. The mean age of patients was 26.06 ± 24.00 months. Table 1 shows the number of bacteria and WBC count categories in children’s urine analysis. Most children had many bacteria and more than 15 WBC in their urine tests. The frequency of susceptibility and resistance to various antibiotics in children’s antibiogram is presented in Table 2. It was observed that the most resistant antibiotic was trimethoprim, reported in 76.1% of patients. We also compared the age and sex between the cases sensitive and resistant to various antibiotics. The age of children resistant to ofloxacin (P = 0.445), cefixime (P = 0.498), cefazolin (P = 0.523), amikacin (P = 0.770), and ciprofloxacin (P = 0.171) was less than the patients sensitive to these antibiotics. However, none of the differences was statistically significant. Comparing the sex of patients, the differences were not statistically significant either for any of the antibiotics. Comparing the age between the categories of WBC count and bacteria in urine analysis, the results showed that the age difference between different WBC categories (P = 0.437) and different bacterial severities (P = 0.170) was not significant. Likewise, the sex distribution between WBC categories (P = 0.459) and different bacterial groups (P = 0.245) did not have any significant difference. Besides, as shown in Table 3, comparing the WBC count in urine analysis among the sensitive and resistant cases to various antibiotics, none of them was statistically significant.
Table 1: The frequency of patients in terms of sex and the number of bacteria and WBC count in their urine analysis.
Table 2: Frequency and percentage of sensitivity and resistance to various antibiotics in the antibiogram.
Table 3: Comparison of WBC count levels in urine analysis among cases sensitive and resistant to various antibiotics.
Discussion
The objective of this study was to determine the E-coli antibiotic resistance patterns in urinary tract infection in children. Out of 160 patients studied, 120 (87.5%) were girls, and the occurrence rate of E. coli UTI was higher in girls, which is also confirmed by the study of Edlin, et al. [10] and Borsari, et al. [11]. Most cases of urinary tract infection had more than 15 WBC and “many” bacteria in urine analysis. Comparing the antibiotics’ sensitivity and resistance, no significant difference between different categories of number of bacteria and WBC count in urine analysis was seen. Similarly, in the study of Kadigi, et al. [12] and Parajuli, et al. [13] in Nepal, the sex and age differences between resistance and sensitivity were not significant. In our study, the highest resistance to antibiotics was seen for trimethoprim (76.1%), followed by cefazolin (59.5%), cefixime (52.6%), gentamicin (50%), and ciprofloxacin (35.1%). In a study by Kadigi, et al. Ecoli had the highest resistance to amoxicillin and ampicillin with 100% resistance, followed by trimethoprim (97%), gentamicin (50%), and nalidixic acid and cefotaxime with 47% [12]. Shrestha et al. also reported that the highest resistance of E. coli had been to ampicillin with 87%, followed by piperacillin with 71%, ofloxacin with 62%, and ceftriaxone with 62% resistance [14]. In the study by Edlin et al., in an outpatient pediatric urinary tract infection clinic, they found that the highest resistance was to ampicillin with 45%, trimethoprim with 24%, and cefalotin with 16% [10]. We observed that, like the study of Kadigi, et al. [12] and Shrestha, et al. [14], E. coli had the lowest resistance to nitrofurantoin and amikacin. However, in the study by Borsari, et al. [11], E. coli had the lowest resistance to nitrofurantoin, and no resistance was identified for co-amoxiclav and third-generation cephalosporins. As a result, our study showed that nitrofurantoin and amikacin are the most effective antimicrobial agents for the treatment of UTI. The main limitation of the present study was that we were limited to one pediatric treatment center and to the Iranian race only. However, our study is one of the few research works that examined the relationship of bacteriuria and pyuria intensity with antibiotic sensitivity and resistance.
Conclusion
This study may help physicians to select an appropriate empirical treatment. As most cases of urinary tract infections in children are caused by Ecoli, it is important to know its patterns of antibiotic resistance. It should be noted that the low antibiotic resistance to nitrofurantoin may make nitrofurantoin the treatment of choice for cystitis. Our study also showed that there is significant resistance to cefixime as the first-line treatment for urinary tract infections in children that should be considered when prescribing cefixime. In addition, our study found no statistically significant association between the amount and severity of pyuria and bacteriuria and antibiotic resistance, which indicates that urine analysis did not play a major role in the study of resistance, which could be an important insight in diagnosis. Which oral medications can be used to treat outpatient urinary tract infections? Further studies are required.
Acknowledgement
We would like to thank the Vice-Chancellor for Research of the Mashhad University of Medical Sciences for approving this study with the code 960759. The study protocol was fully approved by the Ethics Committee of Mashhad University of Medical Sciences (#IR. MUMS.fm.REC.1396.687).
References
- Zorc JJ, Kiddoo DA, Shaw KN (2005) Diagnosis and management of pediatric urinary tract infections. Clin microbiol rev 18(2): 417-422.
- Chua M, Ming J, Chang SJ, Dos Santos J, Mistry N, et al. (2018) A critical review of recent clinical practice guidelines for pediatric urinary tract infection. Can Urol Assoc 12(4): 112.
- Desai DJ, Gilbert B, McBride CA (2016) Paediatric urinary tract infections: Diagnosis and treatment. Aust fam physician 45(8): 558.
- Downing H, Thomas-Jones E, Gal M, Waldron CA, Sterne J, et al. (2012) The diagnosis of urinary tract infections in young children (DUTY): protocol for a diagnostic and prospective observational study to derive and validate a clinical algorithm for the diagnosis of UTI in children presenting to primary care with an acute illness. BMC infect dis 12(1): 1-15.
- Tsai JD, Lin CC, Yang SS (2016) Diagnosis of pediatric urinary tract infections. Urol Sci 27(3): 131-134.
- Mirsoleymani SR, Salimi M, Shareghi Brojeni M, Ranjbar M, Mehtarpoor M (2014) Bacterial pathogens and antimicrobial resistance patterns in pediatric urinary tract infections: a four-year surveillance study (2009–2012). Int j pediatr.
- Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ (2015) Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat rev microbiol 13(5): 269-284.
- Watson AR (2007) Management of urinary tract infection in children. BMJ (Clinical research ed) 335(7616): 356-357.
- Yen ZS, Davis MA, Chen SC, Chen WJ (2003) A cost–effectiveness analysis of treatment strategies for acute uncomplicated pyelonephritis in women. Acad emerg med 10(4): 309-314.
- Edlin RS, Shapiro DJ, Hersh AL, Copp HL (2013) Antibiotic resistance patterns of outpatient pediatric urinary tract infections. J urol 190(1): 222-227.
- Borsari AG, Bucher B, Brazzola P, Simonetti GD, Dolina M, et al. (2008) Susceptibility of Escherichia coli strains isolated from outpatient children with community-acquired urinary tract infection in southern Switzerland. Clin ther 30(11): 2090-2095.
- Kadigi D, Mosha F, Moyo S, Matee M (2020) Etiology and Antimicrobial Susceptibility Patterns of Bacterial Agents Causing Urinary Tract Infection in Children under Five years, dar es Salaam. J Biotechnol Immunol 2(1): 2.
- Parajuli NP, Maharjan P, Parajuli H, Joshi G, Paudel D, et al. (2017) High rates of multidrug resistance among uropathogenic Escherichia coli in children and analyses of ESBL producers from Nepal. Antimicrob Resist Infect Control 6(1): 9.
- Shrestha LB, Baral R, Poudel P, Khanal B (2019) Clinical, etiological and antimicrobial susceptibility profile of pediatric urinary tract infections in a tertiary care hospital of Nepal. BMC pediatr 19(1): 36.

 Research Article
Research Article