Introducing the Clinical Case
The Idiopatic Basal Ganglia Calcification (IBGC), or Fahr’s disease, is a rare disease with less than 200 reported cases. It presents an autosomal dominant inheritance pattern and is clinically characterized by the psychiatric disorders, neurological disorders and abnormal movements triad. This clinical case’s purpose is to highlight the importance of communication and multidisciplinary therapeutic choices between psychiatrist and neurologist. A 56-year-old man presents with a panel of acute atypical psychosis that combines delirious ideas of persecution, of intuitive and interpretative mechanism, systematized in networks, with complete adherence to the delirium and anxiodepressive repercussions in a context of auditory hallucinations. This psychiatric panel is associated at different moments in the disease with paraesthesia, haloaesthesia, balance and walking issues combined with an unstable gait, dysarthria, vertigo, postural tremors and static disorders and extrapyramidal syndrome with major akinesia. Clinical and paraclinical exams make a diagnosis of IBGC with mutation of the SLCA20A2 gene Figure 1. Treatment by QUETIAPINE (800mg/day) enables the complete abrasion of the psychotic symptomatology and the combination of benzodiazepines and ALIMEMAZINE reduces anxiety and sleep disorders. Combining QUETIAPINE with benzodiazepines is necessary, initially, to control anxious displays caused by the diagnostic announcement and the knowledge of associated neurologic disorders. LEVODOPA proves to be ineffective, and ROTIGOTINE causes chorea after 6 weeks of treatment, which doesn’t allow finding a fitting treatment that limits abnormal movements and correlated anxiety. Multidisciplinary support combining ergotherapy, physiotherapy, speech therapy and physical exercise in a therapeutic group is initiated when the treatment begins.
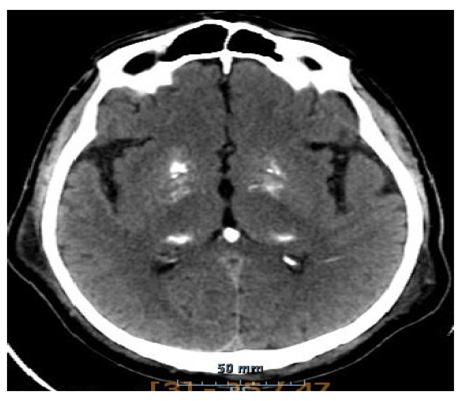
Figure 1: Cerebral scanner without injection in axial section in parenchymatous window. Spontaneous hyperdensity of the internal pallidus globus, the thalamus and the pineal gland corresponding to the calcifications.
Therapeutic Discussion
Fernandez et al have demonstrated that the use of QUETIAPINE in patients suffering from Parkinson’s disease or dementia with Lewy bodies enabled a partial or even complete abrasion of the psychotic symptoms, and with only small dosages (50mg/day). It has also been demonstrated that the continuing use of QUETIAPINE in the long run was compromised in numerous patients because of the deterioration or the outbreak of motor disorders [1]. As our patient was stabilized on 800mg/day of QUETIAPINE and because of motor disorders (especially extrapyramidal syndrome) and their anxio-depressive repercussions, we saw fit to look for an alternative. CLOZAPINE has had a marketing authorization since 2001 for the treatment of psychotic disorders in Parkinson’s disease. The evaluation file has demonstrated that a disappearance of psychotic symptoms happens in 40% of patients, without aggravating the motor symptoms [2]. It has also been established that the necessary dosage of CLOZAPINE is largely inferior to the usual posology for schizophrenia (up to 800 mg/day). Indeed, the average dosage is under 125mg/day and barely ever goes over 250 mg, without increasing the extrapyramidal symptoms in more than 90% of the cases [3]. Given these indications, the treatment by QUETIAPINE was stopped and switched to CLOZAPINE, whose lowest efficient dosage was 62.5mg/day for our patient.
During the patient’s treatment, some neurologic signs appeared (gait disorders, sedation, dizziness) that were linked to Fahr’s disease but could also be related to or potentiated by the benzodiazepines (LORMETAZEPAM/ZOPICLONE) or “hidden” neuroleptics (ALIMEMAZINE) [4]. However, CLOZAPINE produces a sedative effect because of its H1 antagonist, anticholinergic and alpha-1 adrenergic antagonist action. CLOZAPINE, much like HYDROXYZINE, has an H1 antagonist component with anxiolytic features [4]. Therefore, it has been decided to ban the use of benzodiazepines and “hidden” neuroleptics and to use higher dosage of CLOZAPINE associated with HYDROXYZINE in the lowest efficient dosage. The major benefits of a treatment by physiotherapy, speech therapy, physical exercise and also psychotherapy on motor symptoms in Parkinson’s disease have been established in numerous studies [5]. Motor disorders being a strong source of anxiety in our patient, an ergotherapeutic, psychotherapeutic and re-educational treatment enabled a significant improvement on the psychological side. Moreover, we were able to observe an improvement in the memory disorders, especially through the measurement of the MMS (18/30 initially; 25/30 2 years later), and also a stabilization of the motor disorders measured by the SARA and UPDRS III score (initially, SARA: 12.5/40, UPDRS: 32/108; 2 years later, SARA: 8/40, UPDRS: 14/108). We can ascribe these results to the multidisciplinary treatment.
Conclusion
The neuropsychiatric and therapeutic choices and reflexion were capital for this patient. They enabled stabilization and even an improvement of psychiatric symptoms and even of some neurologic symptoms. Considering neurologic signs as elements of the diagnostic but also as factors of aggravation in psychiatric disorders (anxio-depressive) was therefore important. The integrated multidisciplinary treatment was thus the key to the positive clinical evolution of our patient.
References
- Fernandez H, Martha E Trieschmann, Monica A Burke, Joseph H Friedman (2002) Quetiapine for psychosis in Parkinson’s disease versus dementia with Lewy bodies. The Journal of Clinic Psychiatry 63(6): 513-515.
- Prescrire redaction (2001) Clozapine/LEPONEX: En derniers recours en cas de psychose chez les patients parkinsoniens. Revue Prescrire (8): 294-315.
- Riedman J H, Lannon M C (1989) Clozapine in the treatment of psychosis in Parkinson’s disease. Neurology 39(9): 1219-1221.
- Stahl SM (2015) Psychopharmacologie essentielle: bases neuroscientifiques et applications pratiques (4th )., Lavoisier Médecine France.
- Prescrire Rédaction (2011) Traitement de la maladie de Parkinson. D’abord une monothérapie par Lévodopa ou agoniste dompaminergique. Revue Prescrire 31(329): 200-205.

 Case Report
Case Report