ABSTRACT
Hepatic epithelioid hemangioendothelioma (HEHE) is a rare vascular endothelial cancer of the liver that is often misidentified as a metastatic tumor if it is multifocal in the liver or if the patient has another concurrent primary malignancy. We present the case of a patient with buccal cancer and some hypoechoic nodules, as identified through ultrasonography. 18F-labeled fluoro-2-deoxyglucose (FDG) positron emission tomography revealed nodules with increased FDG uptake in the patient’s liver. After liver core biopsy, HEHE was diagnosed. Ultimately, hepatectomy was performed to treat the HEHE. No recurrence was observed on the patient’s computed tomography images at a 3-month follow-up.
Keywords: Hepatic Epithelioid Hemangioendothelioma; Positron Emission Tomography; Metastasis
Abbreviations: HEHE: Hepatic Epithelioid Hemangioendothelioma; PET: Positron Emission Tomography; CT: Computerized Tomography; 18F-FDG: 18F-Labeled Fluoro- 2-Deoxyglucose; VEGF: Vascular Endothelial Growth Factor
Introduction
Hepatic Epithelioid Hemangioendothelioma (HEHE) is a rare malignant type of vascular tumor composed of epithelioid and histiocytoid endothelial cells in a myxohyaline or fibrous stroma. It is often misidentified as a metastatic tumor if it is multifocal in the liver or if the patient has another concurrent primary malignancy. HEHE cells can be classified into three histological types: epithelioid, dendritic, and intermediate cells. Most patients with HEHE are asymptomatic and receive their diagnoses incidentally. Liver core biopsy is the standard method for diagnosing HEHE. the typical imaging features of HEHE include enhancement on arterial-phase CT scans and low signals on venous-phase and delayed-phase CT scans. In addition, 18F-labeled fluoro-2-deoxyglucose (18F-FDG) positron emission tomography (PET) usually reveals increased 18F-FDG uptake. Hepatectomy and liver transplantation are firstline treatments for HEHE. If a patient cannot receive surgery, then antiangiogenic drugs, radiotherapy, chemotherapy, radiofrequency ablation, or transcatheter arterial chemoembolization may be considered. The prognosis of HEHE is generally more favorable than that of other malignant liver tumors. Herein, we present the case of a patient with buccal cancer and HEHE. The patient underwent segmental hepatectomy and had no recurrence at a 3-month follow-up.
Case Report
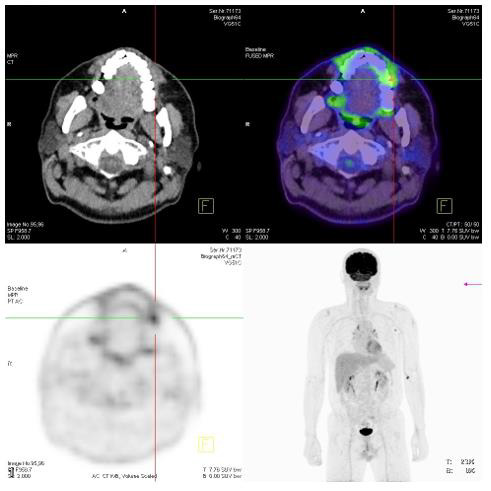
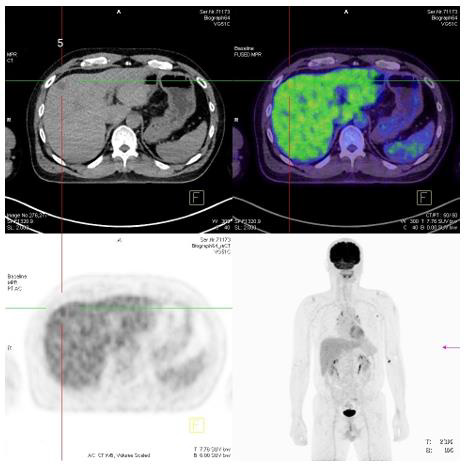
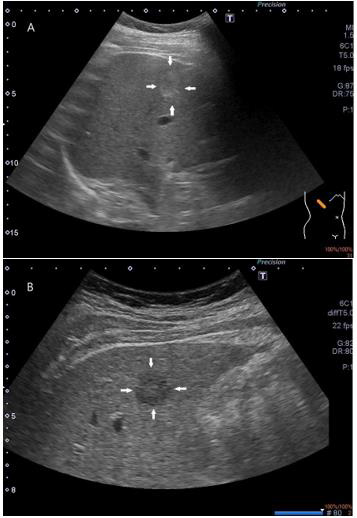
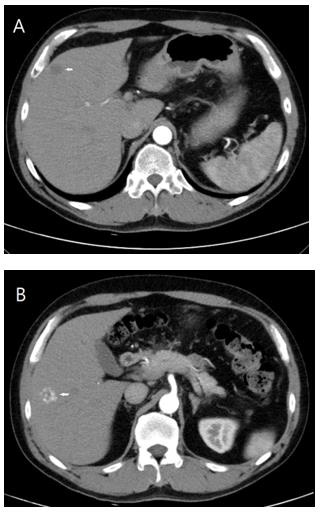
A 50-year-old male with chronic hepatitis C reported having engaged in habitual smoking and betel nut chewing for over 20 years. He complained of odynophagia and tenderness over his left buccal area for 2 months. He visited a physician for help. An ulcerative lesion was discovered over his left buccal area. A biopsy of the lesion was performed, and pathology revealed squamous cell carcinoma. PET was therefore arranged for cancer staging. The PET revealed a hypermetabolic lesion of approximately 0.55 cm without definite evidence of nodal or distant metastasis (Figure 1). The patient’s stage was tentatively denoted as T1N0M0. However, some hypermetabolic nodules (of up to 2 cm) in the right hepatic lobe were also observed (Figure 2). Malignant tumors or metastasis was suspected. The patient’s tumor markers, including αFP, CEA, and CA19-9, were within the normal limits. The patient was transferred to the gastrointestinal clinic for further management. The patient’s liver tumors were further investigated through abdominal sonography; some of the lesions were hyperechoic (Figure 3a), and others were hypoechoic (Figure 3b). The patient also underwent CT. Some nodules were observed in the patient’s liver; two were heterogeneous tumors (1.2 and 1.9 cm) with delayed-phase enhancement in the S4b and S5 segments (Figure 4a), and the others were identified as hemangiomas (Figure 4b). Liver biopsy was arranged for the S4b and S5 tumors. The final pathology revealed epithelioid hemangioendothelioma. Segmental hepatectomy was arranged after the patient had recovered from buccal cancer surgery. The surgical specimens were sent to a pathologist, and the diagnosis of epithelioid hemangioendothelioma was finalized. A CT scan was performed 3 months later and revealed no recurrence of the liver tumors (Figure 5).
Figure 1: A small increased FDG uptake (SUV:6.7, 0.55 cm) in left anterior buccal region, and compatible with malignant tumoral uptake. SUV: standard uptake value.
Figure 2: Some hypodense nodules (about 2 cm) in right hepatic lobe, with FDG uptake similar to or slightly higher than normal hepatic parenchyma.
Figure 3: A. A hyperechoic lesion (up to 1.6cm) in the right lobe of liver (white arrow).
B. A hypoechoic lesion about 1.5cm is also found in the right lobe of liver (white arrow).
Figure 4:
A. A heterogeneous tumors with delay enhancement is found in the right lobe.
B. A hyper-vascular lesion is noted in the right lobe, and hemangioma is diagnosed.
Figure 5:
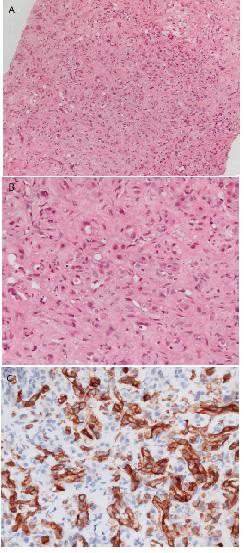
a. In 100x power field, it shows proliferation of epithelioid tumor cells with round hyperchromatic and pleomorphic nuclei, small nucleoli and moderate amount of eosinophilic cytoplasm, in myxohyaline stroma.
b. In 400x power field, some tumor cells contain intracytoplasmic vacuoles, with entrapped red blood cells. Occasional abnormal mitotic figures are seen.
c. In Immunohistochemical staining, it’s positive to CD34.
Discussion
Background
HEHE is a rare malignant type of vascular tumor composed of epithelioid and histiocytoid endothelial cells in a myxohyaline or fibrous stroma. Its incidence is 1 to 2 cases per 1 million people [1]. HEHE can originate in soft tissue, bone, the head or neck, or the liver or other organs. HEHE is slightly more common among patients aged 30 to 40 years than among other age groups and is more common among women than among men [2]. The etiology of HEHE remains unknown; however, some studies have reported that oral contraceptive use, alcohol consumption, liver trauma, sarcoidosis, Crohn disease, vinyl chloride or asbestos exposure, and hepatitis B and C are associated with HEHE [1-4]. Studies have reported that 25% to 40% of patients with HEHE are asymptomatic upon diagnosis. Among patients with symptoms, right upper quadrant pain is the most common symptom. Other symptoms include ascites, weight loss, anorexia, weakness and fatigue, nausea, and vomiting. Alkaline phosphatase, aspartate aminotransferase, and alanine transaminase may be elevated in some patients [3,5-7].
Imaging
HEHE lesions are hypoechoic in ultrasonography. In contrastenhanced ultrasound images, HEHE lesions exhibit enhancement in the arterial phase and low signals in the venous and delayed phases [8]. On CT scans, single or multifocal nodular peripheral lesions with early ring enhancement followed by late appearance of central core enhancement are common features used to diagnose HEHE [2]. Low and high signals appear on T1 and T2 magnetic resonance images, respectively [9]. A common feature of HEHE on T2 images is a target sign with a high-signal core, low-signal ring, and weak secondary high-signal halo. 18F-FDG PET is a powerful tool for detecting metastasis in patients with HEHE [10]. Most HEHE cells exhibit only slightly elevated FDG uptake; this differs from cholangiocarcinoma cells, which exhibit greatly elevated FDG uptake [10].
Histology
HEHE appears as nests and cords of epithelioid endothelial cells spread throughout a myxohyaline stroma. HEHE cells can be classified into three types: epithelioid cells (which are rich in eosinophilic cytoplasm and contain atypical nuclei), dendritic cells (which contain cytoplasmic processes), and intermediate cells (which have characteristics between those of epithelioid cells and dendritic cells). These cells are typically embedded in mucus hyaluronate or hardened matrix. In addition, signet ring–like cytoplasmic vacuoles may appear in epithelioid and dendritic HEHE cells [11]. Immunohistochemical staining of HEHE cells is typically positive for the endothelial markers CD31, CD34, CD12, vimentin, and factor VIII antigen [12]. One study determined that 99%, 94%, and 86% of HEHE cells are positive for factor VIII antigen, CD34, and CD31, respectively [12].
Molecular Characterization
CAMTA1 is a calmodulin-binding transcriptional activator, and WWTR1 is a transcriptional coactivator [13]. Up to 90% of HEHE tumors exhibit WWTR1–CAMTA1 fusion resulting from t(1; 3) (p36; q25) translocations [14]. Therefore, HEHE presents with a rearrangement/deletion of WWTR1–CAMTA1 or YAP1–TFE3 fusion and is characterized by well-formed vasoformative tumors with abundant eosinophilic cytoplasm, atypical cytogenetics, pseudoalveoli, and partly solid-state growth patterns [15]. Only one case of TFE3 rearrangement in HEHE has been reported [16]. Researchers have suggested that testing for TFE3 rearrangement through immunostaining may be useful in the differential diagnosis of HEHE. Other markers such as ERG and AE1/AE3 are expressed in HEHE cells but are also expressed in other tumor cells and are therefore not useful for differential diagnosis [17,18].
Diagnosis
Although specific image findings can be used to diagnose HEHE, liver core biopsies with immunohistochemical staining still play a key role [19]. HEHE is commonly diagnosed on the basis of microscopic features, specifically numerous proliferating dendritic or epithelioid cells with eosinophilic cytoplasm that test positive for CD31, CD34, or factor VIII antigen.
Treatment
HEHE is a rare cancer for which no standard treatment strategy currently exists. Antiangiogenic drugs, radiotherapy, chemotherapy, hepatectomy, liver transplantation, radiofrequency ablation, transcatheter arterial chemoembolization, and observation (watchful waiting) are commonly applied in the treatment of HEHE [20,21]. Surgical resection may be the optimal treatment for single or small HEHE tumors. Because of the vascular origin of HEHE, vascular endothelial growth factor inhibitors such as sorafenib, pazopanib, and bevacizumab are crucial in the treatment of HEHE [22]. For patients with extrahepatic lesions, adjuvant chemotherapy may be an effective alternative approach to disease control [23].
Prognosis
The prognosis of HEHE has a good prognosis compared with that of other malignant liver tumors, and 50% of patients with HEHE survive more than 5 years after diagnosis without treatment. Tumor metastasis has no effect on the 5-year survival rate of HEHE [24]. Hepatectomy and liver transplantation improve patients’ chances of survival; the 1-year and 3-year disease-free survival rates of patients with HEHE who undergo such procedures are 100% and 75%, respectively [25]. The prognosis of HEHE among patients with tumors more than 10 cm in diameter and older adult patients is poor [26]. In one study, researchers developed a HEHE risk stratification strategy based on clinicopathological features; high mitotic activity (>3 mitoses/50 high-power fields) and a tumor size >3 cm were associated with poor prognosis [12]. In addition, 18F-FDG PET is a useful tool for disease follow-up; one study reported that FDG uptake levels provide key information about the progression of HEHE. The prognosis of HEHE among patients with high FDG uptake is usually poor [27].
Conclusion
HEHE is a low-grade to moderate-grade malignant tumor. The 5-year survival rate of patients with HEHE is higher than those of patients with other malignant liver tumors. HEHE can be distinguished from other liver tumors through immunohistochemical staining. Surgical resection remains the first-line treatment for HEHE. If a patient with HEHE is unable or unwilling to undergo surgery, then antiangiogenic drugs, radiotherapy, chemotherapy, radiofrequency ablation, or transcatheter arterial chemoembolization may be considered.
Conflict of Interest
The authors declare that they have no conflicts of interest.
References
- Elleuch N, Dahmani W, Ben SA, Jaziri H, Aya H, et al. (2018) Hepatic epithelioid hemangioendothelioma: A misdiagnosed rare liver tumor. Presse Med 47(2): 182-185.
- Giardino A, Miller FH, Kalb B, Ramalho M, Martin DR, et al. (2016) Hepatic epithelioid hemangioendothelioma: a report from three university centers. Radiol Bras 49(5): 288-294.
- Makhlouf HR, KG Ishak, ZD Goodman (1999) Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer 85(3): 562-582.
- Remiszewski P, Szczerba E, Kalinowski P, Gierej B, Dudek K, et al. (2014) Epithelioid hemangioendothelioma of the liver as a rare indication for liver transplantation. World J Gastroenterol 20(32): 11333-11339.
- Mehrabi A, Kashfi A, Fonouni H, Schemmer P, Schmied BM, et al. (2006) Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer 107(9): 2108-2121.
- Studer LL, DM Selby (2018) Hepatic Epithelioid Hemangioendothelioma. Arch Pathol Lab Med 142(2): 263-267.
- Torres LR, Timbo LS, Freitas Ribeiro CMD, Galvao Filho MM, Yuji Verrastro CG, et al. (2014) Multifocal and metastatic hepatic hemangioendothelioma: case report and literature review. Radiol Bras 47(3): 194-196.
- Afrit M, Nasri M, Labidi S, Mejri N, benna HE, et al. (2017) Aggressive primary hepatic epithelioid hemangioendothelioma: a case report and literature review. Cancer Biol Med 14(2): 187-190.
- Gan LU, Chang R, Jin H, Yang LI (2016) Typical CT and MRI signs of hepatic epithelioid hemangioendothelioma. Oncol Lett 11(3): 1699-1706.
- Kim YJ, Yun M, Lee WJ, Kim KS, Lee JD (2003) Usefulness of 18F-FDG PET in intrahepatic cholangiocarcinoma. Eur J Nucl Med Mol Imaging 30(11): 1467-1472.
- Illueca C, Machado I, Garcia A, Covisa A, Morales J, et al. (2011) Uncommon vascular tumor of the ovary. Primary ovarian epithelioid hemangioendothelioma or vascular sarcomatous transformation in ovarian germ cell tumor? Arch Gynecol Obstet 284(6): 1589-1591.
- Deyrup AT, Tighiouart M, Montag AG, Weiss SW (2008) Epithelioid hemangioendothelioma of soft tissue: a proposal for risk stratification based on 49 cases. Am J Surg Pathol 32(6): 924-927.
- Flucke U, JC Vogels R, Aubain Somerhausen NDS, Creytens DH, Riedl RG, et al. (2014) Epithelioid Hemangioendothelioma: clinicopathologic, immunhistochemical, and molecular genetic analysis of 39 cases. Diagn Pathol 9: 131.
- Mendlick MR, Nelson M, Pickering D, Johansson SL, Seemayer TA, et al. (2001) Translocation t(1;3)(p36.3;q25) is a nonrandom aberration in epithelioid hemangioendothelioma. Am J Surg Pathol 25(5): 684-687.
- Antonescu CR, Loarer FL, Mosquera JM, Sboner A, Zhang L, et al. (2013) Novel YAP1-TFE3 fusion defines a distinct subset of epithelioid hemangioendothelioma. Genes Chromosomes Cancer 52(8): 775-784.
- Kuo FY, Huang HY, Chen CL, Eng HL, Huang CC (2017) TFE3-rearranged hepatic epithelioid hemangioendothelioma-a case report with immunohistochemical and molecular study. Apmis 125(9): 849-853.
- Amer S, M Nabil, M Negm (2022) Expression of Podoplanin in Hepatocellular Carcinoma in a Sample of Egyptian Population – Immunohistopathological Study. Open Access Macedonian Journal of Medical Sciences 10(A): 366-375.
- Fujii T, Zen Y, Sato Y, Sasaki M, Enomae M, et al. (2008) Podoplanin is a useful diagnostic marker for epithelioid hemangioendothelioma of the liver. Mod Pathol 21(2): 125-130.
- Miller WJ, Dodd GD, Federle MP, Baron RL (1992) Epithelioid hemangioendothelioma of the liver: imaging findings with pathologic correlation. AJR Am J Roentgenol 159(1): 53-57.
- Cardinal J, Vera MED, Marsh JW, Steel JL, Geller DA, et al. (2009) Treatment of hepatic epithelioid hemangioendothelioma: a single-institution experience with 25 cases. Arch Surg 144(11): 1035-1039.
- Weitz J, Klimstra DS, Cymes K, Jarnagin WR, Angelica MD, et al. (2007) Management of primary liver sarcomas. Cancer 109(7): 1391-1396.
- Bally O, Tassy L, Richioud B, Decouvelaere AV, Blay JY, et al. (2015) Eight years tumor control with pazopanib for a metastatic resistant epithelioid hemangioendothelioma. Clin Sarcoma Res 5: 12.
- Tan Y, Yang X, Dong C, Xiao Z, Zhang H, et al. (2018) Diffuse hepatic epithelioid hemangioendothelioma with multiple splenic metastasis and delayed multifocal bone metastasis after liver transplantation on FDG PET/CT images: A case report. Medicine (Baltimore) 97(22): e10728.
- Llueca A, Piquer D, Maazouzi Y, Medina C, Serra A, et al. (2018) Hepatic epithelioid hemangioendothelioma: A great mimicker. Int J Surg Case Rep 53: 25-28.
- Baek SH, JH Yoon (2013) Computed Tomography and Magnetic Resonance Imaging Findings of a Malignant Hepatic Epithelioid Hemangioendothelioma: A Rare Case of Solitary Small Nodular Form. J Investig Med High Impact Case Rep 1(3): 2324709613504549.
- Treska V, Daum O, Svajdler M, Liska V, Ferda J, et al. (2017) Hepatic Epithelioid Hemangioendothelioma - a Rare Tumor and Diagnostic Dilemma. In Vivo 31(4): 763-767.
- Dong A, Dong H, Wang Y, Gong J, Lu J, et al. (2013) MRI and FDG PET/CT findings of hepatic epithelioid hemangioendothelioma. Clin Nucl Med 38(2): e66-e73.

 Case Report
Case Report