ABSTRACT
Objectives: Pyogenic liver abscess (PLA) is an important neglected global health threat during the COVID-19 pandemic and emerged non-communicable diseases. This study aims to investigate the causality and anti-biotic resistance in patients with PLA in Vietnam.
Methods: Clinical features and treatment outcomes of 96 patients with PLA in Bach Mai Hospital from January 2015 to December 2020 were examined. The laboratory and radiological features, microbiological isolates in blood and pus cultures, antibiotics, and the interpretation of the drug sensitivity tests were performed. Demographic and clinical characteristics, treatment outcomes, and management of these patients were evaluated.
Results: All 96 cases were PLA when they were admitted to the hospital and there were 76 (79.2%) cases with positive bacterial results in pus. The common pathogen was Klebsiella pneumoniae (56.3%), followed by Escherichia coli (7.3%). The isolated Klebsiella pneumoniae strains were susceptible to most of the common antibiotics that were used at the clinic, with low rates of resistance (< 10%) except for ampicillin. The proportion of pleural effusion complications among these patients was 44.8%. Ultrasound-guided needle aspiration of PLA was performed in 36 patients (37.5%) and percutaneous abscess drainage was done in 60 patients (62.5%). There were diabetics (31.1%), followed by biliary diseases (13.5%). Antibiotic treatment and percutaneous drainage were the mainstay of management for PLA patients and successfully cured 95 of 96 participants.
Conclusion: Because all patients were admitted to the hospital with serious complications of PLA, Klebsiella pneumoniae is sensitive to the most available antibiotics, liver inflammation related to this bacteria would be concerned at the early stage for better treatment outcomes. The longer hospital stay of patients in our study might be explained by the large abscess due to the advanced stage of the disease or neglected liver infectious inflammation.
Keywords: Liver Abscess; Pyogenic Liver Abscess
Abbreviations: PLA: Pyogenic Liver Abscess; ALA: Amoebic Liver Abscess; US: Abdominal Ultrasound; CT: Computed Tomography; MRI: Magnetic Resonance Image; AST: Aspartate Aminotransferase; ALT: Alanine Transaminases
Introduction
A pyogenic liver abscess (PLA), a suppurating infection of the hepatic parenchyma is associated with high mortality [1,2]. The incidence of PLA is increasing annually but varies worldwide. In Taiwan, according to a retrospective study, the annual incidence of PLA increased gradually from 10.83 to 15.45 cases per 100,000 people from 2000 to 2011 [3]. In the United States, results from a large study indicated that the incidence of PLA was 3.59 cases per 100,000 people and the annual average percent increased 4.1% from 1994 to 2005 [2]. Data from studies in Canada and Denmark showed that the incidences rate of PLA ranged from 1.1 to 2.3 per 100.000 population [4,5]. Many studies is focusing on the prevalence, clinical characteristics, pathogenesis, and bacteriology, as well as management of PLA patients in other countries [1,6]. In Vietnam, only a few studies in the last decades showed that the prevalence of amoebic liver abscess (ALA) was high as much as 21 per 100,000 inhabitants per year [7] but there was a lack of data about the PLA due to another pathogen in Vietnam. Especially, evidence about the clinical characteristics and treatment outcomes in Vietnam has not been reported. Only one study reported the complications of the PLA case [8]. We analyzed etiology by bacteria culture, antibiotics sensitivity as well as the clinical characteristics and treatment outcomes of PLA patients admitted to the Bach Mai University hospital in Vietnam from January 2015 to December 2020.
Methods
Design of Study
A retrospective study was carried out on 96 PLA patients admitted to Bach Mai University hospital, the biggest national hospital in Northern Vietnam, between January 2015 to December 2020. The research protocol was approved by Bach Mai Ethics Committee having a code BM-2015-141 on Sep. 30, 2015.
Inclusions and Exclusions Criteria
The inclusion criteria included patients who were definitively diagnosed with PLA based on clinical findings, abdominal ultrasound (US), microbiology on blood or aspirate culture results. The exclusion criteria included patients aged under 18 years old, amoebic liver abscess, hydatid liver abscess, previous episodes of PLA.
Data Collection
The data were extracted from the medical records: ID, age; sex; main disease and contribute health events; initial symptoms; clinical manifestations; laboratory data; number, size, and location of lesions; microbiological findings by culture and their antibiotic sensitive; diagnostic and treatment methods; treatment response and mortality. We defined a cryptogenic abscess as a PLA when the obvious source of infection was not found, even though the results of imaging methods and the infection were found. Radiological findings here included abdominal ultrasound, computed tomography (CT), and magnetic resonance image (MRI). A total of 96 etiological samples isolated from the pyogenic liver abscess of the patients was retrospectively analyzed to test the drug sensitivity. The pus culture and drug sensitivity test were performed to identify the pathogens that caused the liver abscess. Pus was directly inoculated on blood agar and MAC agar. Bacteria were identified using the MALDI-TOF system (Bruker, German). The drug sensitivity of the bacteria was determined by analyzing the minimum inhibitory concentration using the M50 system (Phoenix, USA). Cultures were isolated for aerobic and anaerobic organisms using the standard diagnostic techniques.
If both blood and pus cultures were positive, bacteria were considered as the etiologic. The selection of antibiotics and the interpretation of the drug sensitivity results were based on American Clinical and Laboratory Standards Institute recommendations [9,10]. The type, duration, and drug administration of all patients who received antibiotics were recorded for each case. Antibiotics were changed based on the results of cultures. If patients still had persistent signs of sepsis after 5 days of intravenous antibiotics, ultrasound-guided percutaneous needle aspiration and drainage were performed Recovery from PLA was defined as the absence of signs and symptoms together with results of the image. Death from PLA in this study was defined as death during hospitalization and related to PLA.
Data Analysis
Data were presented as mean (range) for numerical values and frequency (percentages) for categorical variables. Statistical analysis was performed using SPSS software (version 23.0, IBM SPSS Statistics, Armonk, NY, USA).
Results
Clinical Characteristics of the Patients
A total of 96 PLA patients, 64 male, and 32 female with a mean age of 53.3±16 years. The most common clinical symptoms were fever 90(93.8%), right upper abdominal pain 92(95.8%), vomiting and nausea in 34(35.4%); Hepatomegaly was reported in 40 cases (41.7%), while right pleural effusion in 43 patients (44.8%) and jaundice in 25 cases (26%) There was a total of 30 patients (31.3%) with diabetes mellitus.
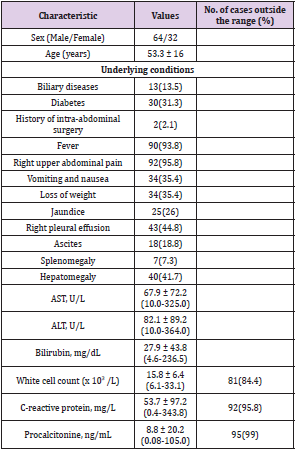
Laboratory and Radiological Features
The common laboratory abnormalities were high white blood cell count (81 cases; 84.4%), the C-reactive protein (92 cases; 95.8%). and procalcitonine (95 casses; 99%) (Table 1). Abdominal ultrasound was implemented in all cases and CT scan and/or MRI were performed in the further diagnosis were needed. The mean size of the liver abscess was 8.5 ± 2.1 cm (min-max: 3.4 – 14.8). There were 80 patients (83.3%) having one abscess when admitted to the hospital. Multiple abscesses were found in 16 cases (16.7%). The presence of gas in the abscess cavity was noted in 12.5% of cases. The abscesses in the right lobe, the left lobe, or in both lobes of the liver were found in 81 patients (84.4%), 10 patients (10.4%), and in 5 patients (5.2%), respectively.
Table 1: Clinical findings and laboratory results for patients with pyogenic liver abscess on presentation.
Note: Values are n (%) or mean ± standard deviation (SD) unless otherwise specified.
Microbiology and Pathogenesis
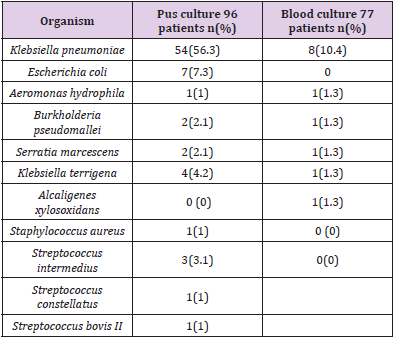
The positive results of culture from an aspirate of liver abscess were found in 76 cases (79.2%). The most common pathogen was Klebsiella pneumoniae (56.3%), followed by Escherichia coli (E.coli) (7.3%). Others bacteria were Klebsiella terrigena (4.2%), Streptococcus intermedius (3.1%), Burkholderia pseudomallei (2.1%), Serratia marcescens (2.1%). The most common underlying disease was diabetics (31.1%), followed by biliary diseases (13.5%).
Management
Patients were treated by image-guided aspiration or drainage of abscess and all patients received intravenous antibiotics before any interventional treatment. Percutaneous aspiration or drainage interventions were performed in different sizes of abscesses. Empirical antibiotic treatment was started at the onset of the clinical infection and changed upon the results of antibiotic susceptibility tests. Ultrasound-guided needle aspiration of PLA was performed in 60 patients (62.5%) and percutaneous abscess drainage was performed in 36 patients (37.5%). The removal of the percutaneous drain was based on the patient’s clinical and laboratory response. The median drainage duration was 9.5 ± 6.5 days. The average mean hospital stay was 17.4 ± 7.4 days.
Complications and Outcomes
The systemic effects of the sepsis were in three patients and only one 84 year- old female patient died from severe sepsis due to Aeromonas hydrophila after 19 days of treatment.
Results of Analysis of Pathogens
These results indicate that the most common organism identified from the liver abscess aspiration cultures was Klebsiella pneumoniae. There were 78 patients (95.1%) who used antibiotics that matched with the sensibility of the bacteria. The empirical treatment was proved to be adequate in most patients. The isolated Klebsiella pneumoniae strains were susceptible to most of the common antibiotics that were used at the clinic, with low rates of resistance (< 10%) except for ampicillin (Figure 1). There was 99% of 96 patients recovered after the treated course at the hospital.
Discussion
The most important new findings included the pathogen of Klebsiella pneumonia infection among a large proportion of people suffering from diabetes mellitus and biliary tract diseases. The proportion of pleural effusion complications was nearly half of participating patients. Most available antibiotics could be successfully used to treat the infection from Klebsiella pneumonia in combination with image-guided aspiration or drainage of the abscess. The longer hospital stay of patients in our study might be explained by the large abscess due to the advanced stage of the disease that suggested liver infectious inflammation might be neglected health treats among people having chronic health events of diabetes and biliary tract diseases. Routine screening for liver inflammation due to Klebsiella pneumonia infection and other pathogens including cancer at the early stage for further successful treatment would be recommended.
Figure 1: The drug resistance of strains of Klebsiella pneumoniae.
Note: AMP= ampicillin, CAZ= ceftazidime, CIP= ciprofloxacin, CRO= ceftriaxone, ETP= ertapenem, GEN= gentamicin, IPM= imipenem, LVX= levofloxacin, MEM= meropenem, TZP= piperacillin/tazobactam, PEP = Cefepime, SCF= Cefoprrazol+Sulbactam, COX= Cefotaxim, AMC= Amoxicillin+ A.clavulanic, CPL= Chloramphenicol.
In this study, the clinical characteristics and treatment outcomes of 96 patients with PLA were reported. The average age of PLA patients in this study was 53.3 years old, lower than the average age of patients with PLA in other studies in the literature (59.1-65 years) [6,11-14]. The common clinical abdominal findings were fever and right upper abdominal pain which were similar to the findings from previous studies [15-18]. However, the proportion of pleural effusion in this study (44.8%) was higher than in the previous study (26.1%-34.5%) [19,20]. The etiologies of PLA have shifted from intra-abdominal infections such as acute appendicitis and trauma to pathologic conditions of the biliary tract; however, up to 55% of patients with PLA have no clear risk factors and these cases are called cryptogenic [21,22]. According to literature, diabetes mellitus is known as an important risk factor of PLA, but the incidences of diabetes mellitus in KP-PLA are varied in different countries, for instance, 38.1% in China [23] and 25% in the United States [24].
Our study also realized that PLA appeared more frequently in patients with diabetes mellitus (31,3%) and biliary tract diseases (13,5%). The position of abscesses was mostly found in the right lobe of the liver and this result was similar to the result of another study [20]. The percentage of cases with the presence of gas within the abscess in our results was 12.5%. Gas-forming in PLA (GFPLA) remains one of the most dangerous complications with a high fatality rate. Klebsiella pneumoniae is the most common pathogen causing GFPLA and Gas-forming pyogenic liver abscess, which accounts for 7 to 24% of pyogenic liver abscesses [25]. The results suggested that K. pneumonia was the most common microorganism isolated from PLA patients, accounting for 54 cases (56.3%). This result is consistent with recent findings reported in other Asian countries [16,26]. Another study in Europe found that the common ones were E Coli and Enterococcus [18,27] but in our study, E. coli was the second pathogen causing PLA. In addition, Klebsiella terrigena, Streptococcus intermedius, Serratia marcescens, and Serratia marcescens were also pathogens of PLA.
It has been reported that the mortality rate of non- K. pneumoniae liver abscess was higher than that of K. pneumonia [28,29]. However, in this study, there was only one death due to Aeromonas hydrophila and this finding is similar to the result from another study showing that the mortality rate of PLA has decreased over the years [1]. Septicemia was found in 14 cases (14.6%) in our study. In a previous study in Europe, from 1992 to 2005, mortality associated with PLA was higher, 19% and the main risk factors were the development of sepsis and/or septic shock [20]. According to literature, percutaneous catheter drainage (PCD) was reported more effective than percutaneous needle aspiration (PNA), for example, a study conducted in 306 patients comparing the effectiveness of PCD and PNA in the management of liver abscess showed that PCD was more effective than PNA because of its higher success rate, reducing the time to achieve clinical relief, and supporting a 50% reduction in abscess cavity size [30]. In this study, all patients received antibiotic treatment and underwent percutaneous aspiration or drainage and ultrasound-guided catheter drainage was performed in PLA cases with abscess sizes over 5 cm in diameter.
The overall mean hospital stay was 17.4 ± 7.4 days. The longer hospital stay of patients in our study might be explained by the large abscess due to the advanced stage of the disease, the average size of the abscess among cases was 8.5 cm and the largest size was 14.8 cm. While a retrospective study of PLA focusing on Klebsiella pneumoniae in China, Yun Qian, et al. [6] showed that the average size of the abscess was 6.9 cm and the average length of stay was 18.6 ± 12.9 days. There are some limitations to our study. Firstly, the study was conducted in a hospital that might not be represented the disease in the general population. We only implemented a profile of the antibiotic resistance of K. pneumoniae, dominating pathogenic bacteria in PLA. Another limitation is the absence of hepatitis B infection and its role in developing PLA in the present study. Despite some limitations, the study has added new findings of PLD management and treatment, especially in the present study population that would be applied in Vietnam and low-medium developing countries.
The results show that fever and right upper abdominal pain were common initial clinical symptoms among PLA cases. The most common pathogen was Klebsiella pneumoniae. The antibiotic treatment and percutaneous drainage were the mainstay of management for PLA patients. This study might provide a valuable reference for clinicians in Vietnam who encounter this uncommon condition. About 20% of PLA has not detected bacteria listed in Table 2 that warrants further significant examination of this disease.
Table 2: Microbiological isolates in blood and pus cultures.
Note: * NPDR = non-proliferative diabetic retinopathy, PSV = peak systolic rate of blood flow, CRA = central artery retina, CVR = central vein retina, SPCA = short rear cylinder artery, EA = eye artery, ri = resistant index; * p <0.05; ** p <0.01 - from healthy, # p <0.05 - from the NDR IA, ^ P <0.05- from the NDRR IB; SD = Standard deviation.
Data Availability
Data are included within the manuscript.
Ethical Approval
Ethics approval of this study was given by the Research Ethics Committees of Bach Mai hospital having a code BM-2015-141 on Sep. 30, 2015.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Funding Statement
School of Medicine and Pharmacy, Vietnam National University Hanoi, Hanoi, Viet Nam, No. QGSP.2021.07.
Acknowledgment
The authors would like to thank Bach Mai Hospital for supporting this research.
References
- Rahimian J, Wilson T, Oram V, Holzman RS (2004) Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis 39(11): 1654-1659.
- Meddings L, Myers RP, Hubbard J, Shaheen AA, Laupland KB, et al. (2010) A population-based study of pyogenic liver abscesses in the United States: incidence, mortality, and temporal trends. Am J Gastroenterol 105(1): 117-124.
- Chen YC, Lin CH, Chang SN, Shi ZY (2016) Epidemiology and clinical outcome of pyogenic liver abscess: an analysis from the National Health Insurance Research Database of Taiwan, 2000-2011. J Microbiol Immunol Infect 49(5): 646-653.
- Jepsen P, Vilstrup H, Schønheyder HC, Sørensen HT (2005) A nationwide study of the incidence and 30-day mortality rate of pyogenic liver abscess in Denmark, 1977-2002. Aliment Pharmacol Ther 21(10): 1185-1188.
- Hansen PS, Schønheyder HC (1998) Pyogenic hepatic abscess. A 10-year population-based retrospective study. Apmis 106(3): 396-402.
- Qian Y, Wong CC, Lai S, Chen H, He X, et al. (2016) A retrospective study of pyogenic liver abscess focusing on Klebsiella pneumoniae as a primary pathogen in China from 1994 to 2015. Sci Rep 6: 38587.
- Blessmann J, Le Van A, Tannich E (2006) Epidemiology and Treatment of Amebiasis in Hué, Vietnam. Archives of Medical Research 37(2): 269-271.
- Pham Van T, Vu Ngoc S, Nguyen Hoang NA, Hoang Huu D, Dinh Duong TA (2020) Ruptured liver abscess presenting as pneumoperitoneum caused by Klebsiella pneumoniae: a case report. BMC Surgery 20(1): 228.
- (2013) Clinical & Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fourth Informational Supplement. Clinical and Laboratory Standard Institute, USA 33(1).
- (2015) Clinical & Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fourth Informational Supplement. Clinical and Laboratory Standard Institute, USA 35(1).
- Tan YM, Chung AYF, Chow PKH, Cheow PC, Wong WK, et al. (2005) An appraisal of surgical and percutaneous drainage for pyogenic liver abscesses larger than 5 cm. Annals of Surgery 241(3): 485-490.
- Chen SC, Yen CH, Tsao SM, Huang CC, Chen CC, et al. (2005) Comparison of pyogenic liver abscesses of biliary and cryptogenic origin. An eight-year analysis in a University Hospital. Swiss Med Wkly 135(23-24): 344-351.
- Petri A, Höhn J, Hódi Z, Wolfárd A, Balogh A (2002) Pyogenic liver abscess - 20 years' experience. Comparison of results of treatment in two periods. Langenbecks Arch Surg 387(1): 27-31.
- Pang TCY, Fung T, Samra J, Hugh TJ, Smith RC (2011) Pyogenic liver abscess: An audit of 10 years experience. World journal of gastroenterology 17(12): 1622-1630.
- Foo NP, Chen KT, Lin HJ, Guo HR (2010) Characteristics of Pyogenic Liver Abscess Patients With and Without Diabetes Mellitus. Official Journal of the American College of Gastroenterology 105(2): 328-335.
- Kong H, Yu F, Zhang W, Li X (2017) Clinical and microbiological characteristics of pyogenic liver abscess in a tertiary hospital in East China. Medicine 96(37): e8050-e8050.
- Ali AH, Smalligan RD, Ahmed M, Khasawneh FA (2013) Pyogenic liver abscess and the emergence of Klebsiella as an etiology: a retrospective study. Int J Gen Med 7: 37-42.
- Serraino C, Elia C, Bracco C, Rinaldi G, Pomero F, et al. (2018) Characteristics and management of pyogenic liver abscess: A European experience. Medicine (Baltimore) 97(19): e0628.
- Mischinger HJ, Hauser H, Rabl H, Quehenberger F, Werkgartner G, et al. (1994) Pyogenic liver abscess: Studies of therapy and analysis of risk factors. World Journal of Surgery 18(6): 852-857.
- Ruiz-Hernández JJ, León-Mazorra M, Conde-Martel A, Marchena-Gómez J, Hemmersbach-Miller M, et al. (2007) Pyogenic liver abscesses: mortality-related factors. Eur J Gastroenterol Hepatol 19(10): 853-858.
- Kuo SH, Lee YT, Li CR, Tseng CJ, Chao WN, et al. (2013) Mortality in Emergency Department Sepsis score as a prognostic indicator in patients with pyogenic liver abscess. The American Journal of Emergency Medicine 31(6): 916-921.
- Huang CJ, Pitt HA, Lipsett PA, Osterman FA Jr, Lillemoe KD, et al. (1996) Pyogenic hepatic abscess. Changing trends over 42 years. Annals of Surgery 223(5): 600-609.
- Yin D, Ji C, Zhang S, Wang J, Lu Z, et al. (2021) Clinical characteristics and management of 1572 patients with pyogenic liver abscess: A 12-year retrospective study. Liver Int 41(4): 810-818.
- Pastagia M, Arumugam V (2008) Klebsiella pneumoniae liver abscesses in a public hospital in Queens, New York. Travel Med Infect Dis 6(4): 228-233.
- Lee HL, Lee HC, Guo HR, Ko WC, Chen KW (2004) Clinical Significance and Mechanism of Gas Formation of Pyogenic Liver Abscess Due to Klebsiella pneumoniae. J Clin Microbiol 42(6): 2783-2785.
- Luo M, Yang XX, Tan B, Zhou XP, Xia HM, et al. (2016) Distribution of common pathogens in patients with pyogenic liver abscess in China: a meta-analysis. European journal of clinical microbiology & infectious diseases: official publication of the European Society of Clinical Microbiology 35(10): 1557-1565.
- Zhu X, Wang S, Jacob R, Fan Z, Zhang F, et al. (2011) A 10-year retrospective analysis of clinical profiles, laboratory characteristics, and management of pyogenic liver abscesses in a Chinese hospital. Gut Liver 5(2): 221-227.
- Yang CC, Yen CH, Ho MW, Wang JH (2004) Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. J Microbiol Immunol Infect 37(3): 176-84.
- Chen SC, Yen CH, Lai KC, Tsao SM, Cheng KS, et al. (2005) Pyogenic liver abscesses with Escherichia coli: etiology, clinical course, outcome, and prognostic factors. Wiener klinische Wochenschrift 117(23): 809-815.
- Cai YL, Xiong XZ, Lu J, Cheng Y, Yang C, et al. (2015) Percutaneous needle aspiration versus catheter drainage in the management of liver abscess: a systematic review and meta-analysis. HPB (Oxford) 17(3): 195-201.

 Research Article
Research Article