ABSTRACT
We present the case of a patient with a conclusive diagnosis of incipient C3- C4 discopathy, associated with significant instability of the C2-C3 segment with hypermobility in this segment and inversion of segmental lordosis, causing facet and muscle overload, which triggers continuous biomechanical overload, with consequent severe and intractable pain complaints. This clinical case escapes the usual day-today treatment patterns of the spine surgeon, mainly because it is a reoperation of a tumor sequel, where the posterior anatomy is distorted and reveals severe adherence between the planes and medullary structures, which makes the posterior approach difficult. In addition, the patient presented frequent and excruciating pain crises without improvement with regular therapies, including not responding to treatment with corticosteroids and high-potency opioids such as morphine and methadone. The patient underwent two foraminal and facet blocks in addition to cervical rhizotomy rescue treatment with partial relief of symptomatic patients due to anesthetic application, showing that this was the trigger point of the patient’s pain complaint.
However, it was only a short-term improvement and indicated that conservative therapy would not present satisfactory results in the medium or long term. Given the above, the clinical team decided on a non-routine hybrid procedure with arthrodesis via anterior approach with a stand-alone lordotic cage in the C2-C3 segment associated with arthroplasty of the C3-C4 segment. We provided fusion between the C2-C3 vertebral bodies through this surgical intervention, solving its instability and hypermobility. By reconstructing the normal anatomy of the C3-C4 segment, we achieved the objective of improving cervical lordosis and severe pain.
Patient Information
Female patient, 32 years old, veterinarian, complaining of severe chronic neck pain associated with a frequent headache that started 17 years ago. In 2005, at 15-year-old, the patient was diagnosed with an aneurysmal bone cyst (ABC) in the cervical spine. She underwent a surgical procedure for tumor resection (excisional biopsy) conducted by another surgical team; the biopsy indicated no malignancy in the extracted tissue. After the surgery, the patient had temporary pain relief. However, the pain crises returned, which improved with analgesics and non-steroidal anti-inflammatory drugs (NSAIDs). However, the pain evolved with progressive worsening refractory, and the patient received treatment with more potent palliatives such as opioids plus rehabilitation therapy. There were no reports of pain irradiation to the upper limbs, neurological changes (sensory and motor), history of trauma, fever, and weight loss.
Diagnostic Assestment and Clinical Intervention- 2018 -2020
After frequent unsuccessful attempts to resolve her clinical condition in an emergency care service, the patient came to our medical team in 2018 for diagnostic investigation and neck pain control.
Follow-Up and Interventions - 2021
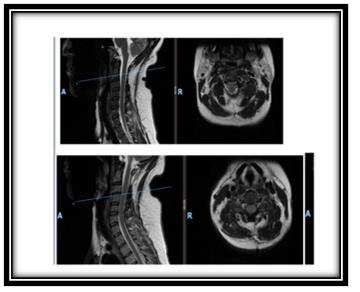
The MRI taken in June 2021 (Figure 1) indicates a normal craniocervical transition. Cervical rectification in the examination position, with minimal inversion. Preserved posterior cervical alignment. Vertebral bodies with typical height. Uncovertebral and interapophyseal joints preserved, except for the remaining C2-C3 stumps. Mild dehydration of the intervertebral discs from C2-C3 to C5-C6. Bulging of the posterior disc fibers from C3-C4 to C5-C6 that touch the anterior surface of the dural sac, without significant spinal or radicular repercussions. Small central C3-C4 protrusion, with discrete annular rupture and minimal medullary contact, without significant compressive effects. Slight thickening of ligamentum flavum at levels C5-C6, C6-C7, determining impression on the dorsal surface of the dural sac. Free intervertebral foramina. Vertebral canal with preserved dimensions.Spinal cord with normal signal strength, thickness, and position. Foci of abnormal uptake by paramagnetic contrast medium are not characterized. Symmetrical paravertebral musculature with preserved trophism
Opinion
Mild degenerative discopathies from C3-C4 to C5-C6. No focal cervical spinal cord lesions attributable to demyelination were demonstrated. Resection of the posterior arch of C2 with facet arthrosis of the remaining segment, grade I C2-C3 listhesis due to segmental instability in C2-C3. Rest of the cervical spine MRI study without significant changes. In the qualitative analysis of the images, the comparative analysis with the reference study (08/06/2020), where the patient was already under follow-up with our medical team, did not show significant changes in the lesion load or spinal cord volume.
Preoperative Assessment
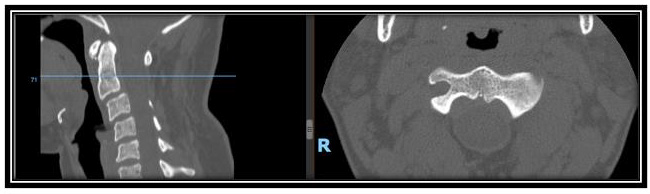
The use of X-rays, MRI, and computed tomography supports the diagnosis. Electromyography was also performed, showing no neurological lesions. The radiography (Figure 2) was performed in anterior, lateral flexion, and lateral views in extension, completing a dynamic cervical radiological study. It indicates an inversion of cervical lordosis, especially in the proximal cervical segments, partial reduction of the C2-C3 disc space with aggressive resection of the posterior arch and significant arthrosis of the remaining portion of the facet joints of this segment; mild partial reduction of the C3-C4 disc space with apparent partial resection of spinous processes and ligament structures. The dynamic images showed a C2-C3 instability, evidenced by a grade I listhesis of C2-C3 with worsening slippage in the flexion and significant segmental angular alteration of C2-C3 in extension. It also presents evident instability of the C3-C4 segment with inversion of the cervical lordosis angle in the flexion and the appearance of mild anterolisthesis with cervical hyperflexion, configuring segmental instability in the C2-C3 and C3-C4 segments.
No other disc or joint changes were observed, in addition to the absence of expansive processes examined through this technique. The computerized tomography (Figure 3) performed by high resolution volumetric technique with multiplanar and 3D surface reconstructions shows rectification with a tendency to invert the physiological curvature of the cervical spine. Slight anterior misalignment of C2-C3 classified as grade I anterolisthesis (slippage of up to 25% of the length of the vertebral body in the anteroposterior direction), degenerative disc disease of the C2- C3 segment, associated with significant resection of the posterior arch of C2, with partial resection of joint facets and segmental arthrosis in the remaining joint portions. Other uncovertebral and interface joints were preserved, except for significant degenerative arthropathy of the remaining C2-C3 stump. Bone structures with typical morphologies in the other segments. Vertebral canal and foramina with preserved calibers. Absence of expansive processes or collections that this procedure can analyze. On December, 2021 after evidence-based analysis and conversations with the patient and her relatives, the health care team decided that the most suitable solution for this patient was a hybrid stabilization, with arthrodesis of the C2-C3 segment, associated with arthroplasty of the C3-C4 segment.
Postsurgical Follow-Up and Outcomes
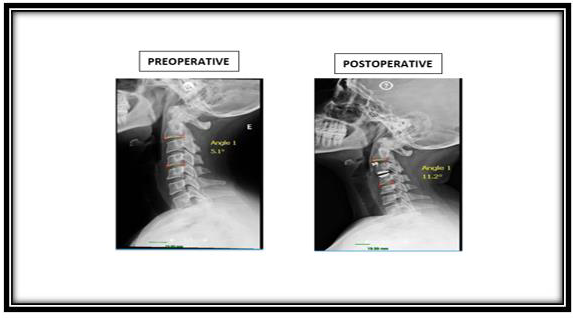
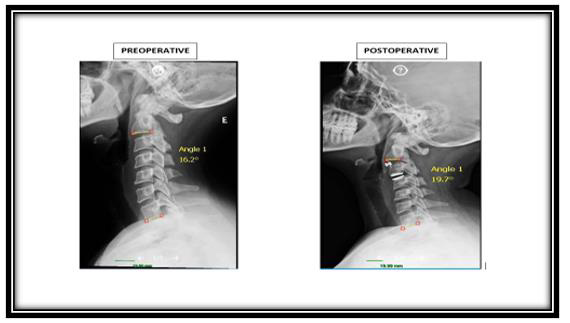
The cervical spine radiography was taken on December 2021 (Figure 4) after the surgery showed the physiological cervical curvature correction. Postoperative control by disc interposition material at C2-C3 and C3-C4 levels without material loosening or failure signs. Resection of the laminae and spinous processes from C2, and partial resection of the C3 and C4 spinous processes. The other disc spaces were preserved. Vertebral bodies with conserved alignment and heights. Marginal osteophytes on vertebral bodies. Other bone structures with normal morphology and texture. Uncovertebral and interface joints intact. Soft parts without alterations. After the surgical intervention, the C2- C3- C4 segment lordosis angle increased significantly from 5.10 to 11.20, an improvement higher than 100% (Figure 5). Post-surgery, the entire cervical spine (C2-C7) lordosis angle improved moderately from 16.20 to 19.70, as shown in Figure 6.
Discussion
When choosing the most suitable surgical procedure for a clinical case, several factors must be considered, focusing on the patient’s needs to improve their functional status. Among them are the patient’s age, the harshness of the condition assessed through imaging and the symptoms presented, level of work, daily activities, associated comorbidities, and the cervical levels affected by the disease (Kalil Debs, et al. [1]). As mentioned above, the patient had undergone complete ABC excision. The ABCs are rare and non-malignant and represent up to 15% of primary tumors of the spine and rarely affect the cervical spine ( Protas M, et al. [2,3]). There is evidence that ABC excision risks include spinal instability (Sebaaly A, et al. [4]). During several years, the patient experienced severe and frequent pain. The C3-C4 discopathy linked to the instability and hypermobility of the C2-C3 segment and inversion of segmental lordosis caused facet and muscle overload, which triggers continuous biomechanical overload.
The instability and inversion of lordosis, alteration of the sagittal cervical balance, is the leading cause of pain in the patient, who had suffered for more than ten years with the effects of this pathology. Through an anterior approach with a stand-alone lordotic cage in the C2-C3 segment, the arthrodesis allowed the fusion between the C2-C3 vertebral bodies, solving its instability and hypermobility. The fusion at this level prevents mobilization of facet joint remains from the first resection procedure, removing the pain of facet origin from the C2-C3 segment. It allows recovery of C2-C3 lordosis, considering that the cage (rigid implant with graft) placed in this disc space is more prominent in the anterior than a posterior portion, thus improving the normal cervical angulation. A third-generation arthroplasty was performed in the C3-C4 segment, consisting of an implant capable of reconstructing the typical disc anatomy, which has an annulus fibrosus and nucleus pulposus the same as the standard intervertebral disc, however with an excellent capacity for the reconstruction of the cervical lordosis.
It has a much higher height in the anterior portion of the artificial disc than its posterior region, which helps reconstruct the sagittal cervical balance without altering the normal anatomy of a cervical segment without the pathology. It is known that the intervertebral disc is the primary stabilizing method of the cervical segment, and it is essential that it presents healthy anatomical characteristics to treat segmental instability and maintain the functionality and mobility of the spinal segment. It must be mentioned that the surgical intervention in the C2-C3-C4 segment also positively impacted the cervical lordosis angle, which increased to 19.70. It is close to the standard values, oscillating between 200 and 400, (UMMC, Kim, et al. [5,6]). The surgical approach allowed reconstructing the normal anatomy of the segment, achieving the objective of improving cervical lordosis and improving the severe pain condition of the patient at present.
Final Considerations
The future and definitive consolidation of the arthrodesis in the C2-C3 segment and an angle increment of the cervical spine lordosis (C2-C7) will take place around 6 to 8 months after the surgery. This process is influenced by some factors that tend to bring lasting comfort to the patient in the clinical case presented here, among others: the adaptation of the organism to the new cervical lordotic position achieved in the postoperative period, an intense program of physical rehabilitation with muscle strengthening and comprehensive postural reeducation.
Conflicts of Interest
The authors declare no relevant conflicts of interest.
References
- Lizandra Gagliardi Kalil Debs, André Evaristo Marcondes Cesar, Luciano Miller Reis Rodrigues, Fernanda Amate Lopes, Marina Rosa Filezio (2020) The Effectiveness of The Most Used Techniques In Patients With Degenerative Cervical Disease. Coluna/Columna 19(1).
- Protas M, Jones LW, Sardi JP, Fisahn C, Iwanaga J, et al. (2017) Cervical spine aneurysmal bone cysts in the pediatric population: a systematic review of the literature. Pediatr Neurosurg 52: 219-224.
- Mankin HJ, Hornicek FJ, Ortiz-Cruz E, Villafuerte J, Gebhardt MC (2005) Aneurysmal bone cyst: a review of 150 patients. J Clin Oncol 23: 6756-762.
- Sebaaly A, Ghostine B, Kreichati G, Mallet JF, Glorion C, et al. (2015) Aneurysmal bone cyst of the cervical spine in children: a review and a focus on available treatment options. J Pediatr Orthop 35: 693–702.
- UMMC- University of Maryland Medical Center.
- Kim D, Davis DD, Menger RP (2022) Spine Sagittal Balance. In: StatPearls.

 Case Report
Case Report