Abbreviations: GI: Glass Ionomers; ADA96: American Dental Association Standard; RMGI: Resin-Modified Glass Ionomer Cements
Introduction
The search for restorative materials that need fewer procedural steps, faster setting time and less cost is very important while dealing with children [1,2]. Glass ionomers (GI) in paediatric dentistry have been widely used for dental restoration due to their advantages as, biocompatibility, chemical adhesion to enamel [3]/ dentin and their abilities of fluoride release [4-6]. In the oral environment, GI must also withstand masticatory and parafunctional stresses [4]. These stresses vary markedly in different clinical situations. Thus, thresholds in the mechanical properties needed for success may vary considerably from case to case, with stronger GI being required where greater stresses are anticipated [7]. In the oral environment dental restorations are exposed to several conditions that cause physical and mechanical change of the restorations, such as wear and discoloration [8]. In attempts to enhance the mechanical properties of a GI, glass ionomer particles have been reacted with a polyacid to forma set glass ionomer matrix structure [9].
A generation of resin-modified glass ionomer cement was introduced in 2007. Ketac N100™, described by the manufacturers as a “nanoionomer,” is known to exhibit improved esthetics while retaining the beneficial qualities like fluoride release. Incorporation of nanotechnology enhances the physical properties like wear resistance, polishability, and esthetics [10]. The conventional GI (acid-base) and other glass ionomer e.g. Equia F®, has been introduced. The mechanism of reinforcement of this GI is based on the presence of evenly dispersed ultrafine and highly reactive glass particles and optimization (increase) of the molecular weight of the polyacrylic acid, leading to formation of a new class of restorative GI with good mechanical properties [1,11]. Conventional ionomer modified by the addition of light-cured resin monomers (hydroxyethyl methacrylate) are commonly classified as Resin-Modified Glass Ionomer Cements (RMGI) [12]. Other GI is Vitremer™ is a RMGI adding resin content has improved its mechanical, physical and optical properties [13]. Hence, this short communication double-blind aims to compare the compressive strength of four different GI (Equia F®, Ketac N100®, Ketac Molar® y Vitremer™) used as restorative material in paediatric dentistry, under the guidedlines of American Dental Association standard (ADA 96) and Standard International Norm (ISO-9917- 1:2007) [14].
Methods
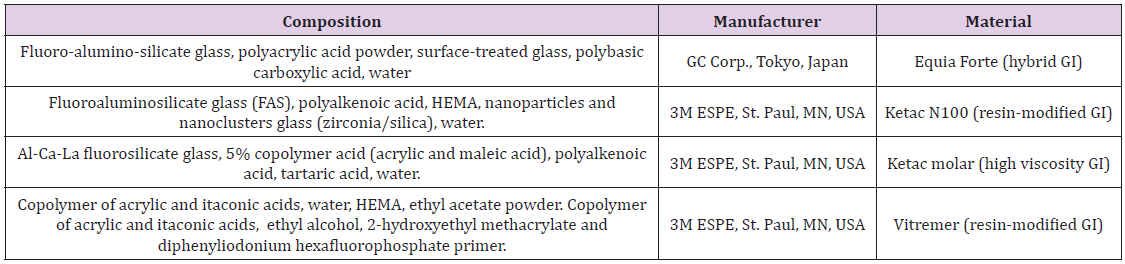
Compositions of GI evaluated and manufacturer’s data are shown are listed in Table 1. The GI were divided into four groups: Equia-F®, Ketac-N100®, Ketac-Molar® and Vitremer™ (n = 14). Specimens’ preparation was performed under controlled temperature (23±1°C / 63±1% RH). Specimens of each GI (n=14) were prepared according to the manufacturer’s instructions (in stainless steel molds) cylindrical molds (4mm-diameter, 6mm height) and transferred to a PolyScience™ oven (37±1ºC/63±1%RH) [15] for 60 minutes; all samples were prepared the same day. Specimens were individually stored in eppendorf tubes (with 2mL deonized water at 37º) in the incubator; 24h and 14 days later, 7 specimens per group were randomly withdrawn and subjected to a compressive load in the universal testing machine (INSTRON® 5567) at a crosshead speed of 1.0mm/min; the maximum load in MPa was recorded. The Shapiro-Wilk test was performed to all the groups. The description of the data was presented using means, standard deviations (SD) and median for the Ketac-Molar®. The hypothesis test was performed with a significance level of p≤0.05. U Mann-Whitney test for Ketac-Molar® and paired t-test was performed to identify differences between each group of ionomers (24h and 14 days). Kruskal Wallis for comparison among groups. Statistical analysis was performed with the GraphPad v.8 program for information processing.
Results and Discussion
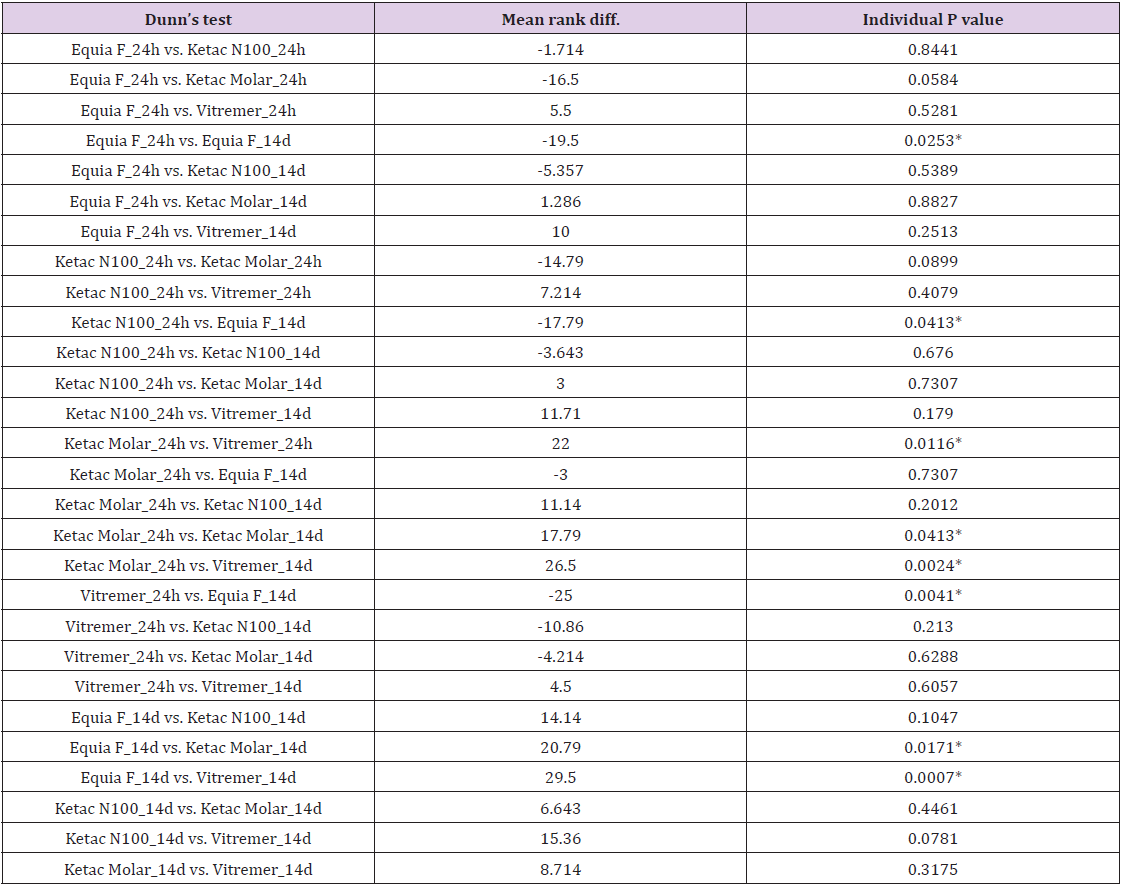
The results of the paired t were as follows: Equia-F® 24h (157±26.1) vs 14 days (197±23.8) were observed significant differences P = 0.0106; Ketac-N100® 24h (159±28.5) vs 14 days (165±12.95) P = 0.6687 and Vitremer™ 24h (147±12.3) vs 14 days (139±14.8) P = 0.1961 there were no significant difference; U Mann-Whitney between Ketac-Molar® 24h (190 median) vs 14 days (129 median) were not observed differences. A Kruskal-Wallis test (post hoc Dunn test) was performed for multiple comparisons among different GI at different matured times (24h and 14 days), as shown in Table 2. ADA 96 [16] Specification for Compressive Strength only requires evaluated the material 24 hours after mixing, in this investigation it was measured and compared at 24 hours and at 14 days.
The GI [17] at 24 hours were compared, the one that obtained the highest compressive strength was Ketac-Molar® (194MPa), however, when the GI was compared at day 14, the best was Equia-F®. The results of this study showed that GI Equia-F® [18,19] is a promising restorative material as the material of first choice in Pediatric Stomatology, with compressive strength values higher than the others GI (24 hours and 14 days). By comparing the Ketac-Molar® 24h vs 14d, significant differences were observed between the same GI, the 24h GI being better, however, in the clinic it is advisable to have greater compressive strength on over time. Different authors compare Equia-F® with different GI modified with resins in vitro, and GI Equia-F® is considered as the material of easy manipulation, and fast setting, both advantages help in managing the behavior of the pediatric patient.
Why this Paper is Important to Paediatric Dentists
a) The best GI for reconstruction restoration in temporary
restorations in paediatric patients is the Equia-F® for having
greater compressive strength, easy manipulation and shorter
setting time.
b) The four GI with the minimum value established by the
96 standard of the ADA (130MPa) and ISO-9917-1:2007 (100MPa);
all obtained a higher compressive strength after 24h and 14 days.
Author Contributions
S.E.G.M: Investigation; J.P.R.O: Supervision, Methodology C.C.B-O: Validation, Writing - Review & Editing, Funding acquisition, Conceptualization, Project administration.
Acknowledgment
This study was obtained for financial support provided via the DGAPA-PAPIIT-IA203219 and IA 200421 projects.
References
- Ali A, El Malt M, Mohamed E (2019) A Comparative Evaluation of EQUIA Forte Microleakage Versus Resin-Modified Glass Ionomer. Al-Azhar Dental Journal for Girls 6(3): 249-254.
- Cássia Mendes da Silva, Márcia Cançado, Figueiredo LC, Tathiane Larissa Lenzi (2019) Survival and Associated Risk Factors of Atraumatic Restorative Treatment Restorations in Children with Early Childhood Caries. Journal Dental Child 87(1): 12-17.
- Faustino-Silva DD, Figueiredo MC (2019) Atraumatic restorative treatment—ART in early childhood caries in babies: 4 years of randomized clinical trial. Clinical Oral Investigations 23(10): 3721-3729.
- Gurgan S, Kutuk Z, Ergin E, Oztas S, Cakir F (2015) Four-year Randomized Clinical Trial to Evaluate the Clinical Performance of a Glass Ionomer Restorative System. Operative Dentistry 40(2): 134-143.
- Bollu IP, Hari A, Thumu J, Lakshmi Deepa Velagula, Nagesh Bolla, et al. (2016) Comparative Evaluation of Microleakage Between Nano-Ionomer, Giomer and Resin Modified Glass Ionomer Cement in Class V Cavities- CLSM Study. J Clin Diagn Res 10(5): 66-70.
- Kumari PD, Khijmatgar S, Chowdhury A, Lynch E, Chowdhury CR (2019) Factors influencing fluoride release in atraumatic restorative treatment (ART) materials: A review. Journal of Oral Biology and Craniofacial Research 9(4): 315-320.
- Irie M, Maruo Y, Nishigawa G, Suzuki K, Watts DC (2008) Class I gap-formation in highly viscous glass-ionomer restorations: delayed vs immediate polishing. Oper Dent 33(2): 196-202.
- Ozkanoglu S, G Akin E (2020) Evaluation of the effect of various beverages on the color stability and microhardness of restorative materials. Nigerian Journal of Clinical Practice 23(3): 322-328.
- Moshaverinia M, Navas A, Jahedmanesh N, Alireza Moshaverinia, Sahar Ansari (2019) Comparative evaluation of the physical properties of a reinforced glass ionomer dental restorative material. J Prosthet Dent 122(2): 154-159.
- André Mallmann, Jane Clei Oliveira Ataíde, Rosa Amoedo, Paulo Vicente Rocha, Letícia Borges Jacques (2006) Compressive strength of glass ionomer cements using different specimen dimensions 21(3): 204-208.
- Diwanji A, Dhar V, Arora R, Madhusudan A, Rathore AS (2014) Comparative evaluation of microleakage of three restorative glass ionomer cements: An in vitro J Nat Sci Biol Med 5(2): 373-377.
- Balkaya H, Arslan S, Pala K (2019) A randomized, prospective clinical study evaluating effectiveness of a bulk-fill composite resin, a conventional composite resin and a reinforced glass ionomer in Class II cavities: one-year results. Journal of applied oral science: revista FOB 7(27): e20180678-e78.
- Souza JC, Silva JB, Aladim A, Rubens M Nascimento, Filipe S Silva, et al. (2016) Effect of Zirconia and Alumina Fillers on the Microstructure and Mechanical Strength of Dental Glass Ionomer Cements. Open Dent J 10: 58-68.
- Paiva L, Fidalgo TKS, da Costa LP, K Anselme, L Ploux, et al. (2018) Antibacterial properties and compressive strength of new one-step preparation silver nanoparticles in glass ionomer cements (NanoAg-GIC). J Dent 69: 102-109.
- Perdigao J, Dutra Correa M, Saraceni SH, Ciaramicoli MT, Kiyan VH (2012) Randomized clinical trial of two resin-modified glass ionomer materials: 1-year results. Oper Dent 37(6): 591-601.
- Ilie N (2018) Maturation of restorative glass ionomers with simplified application procedure. J Dent 79: 46-52.
- Diaz Caballero A, Taron Dunoyer A, Martinez Martinez A (2019) Data of resistance to the compression of restorative dental materials. Data Brief 23: 103755.
- de Oliveira BMB, Agostini IE, Baesso ML, John W Nicholson, Sharanbir K Sidhu, et al. (2019) Influence of external energy sources on the dynamic setting process of glass-ionomer cements. Dental Materials 35(3): 450-456.
- Grossi JA, Cabral RN, Ribeiro APD, Leal SC (2018) Glass hybrid restorations as an alternative for restoring hypomineralized molars in the ART model. BMC Oral Health 18(1): 65.

 Short Communication
Short Communication