Abstract
Background: Advances in the management of patients with diabetes mellitus (DM)
in recent years do not reduce the risk of chronic kidney disease (CKD), but provide
a delay in its development. Violation of carbohydrate metabolism and the associated
violation of lipid metabolism is a factor in the progression and development of diabetic
nephropathy(DN).
Materials and Methods: The prospective study included 80 patients with type 2
diabetes with DN. The duration of diabetes mellitus was on average 9.7 ± 0.9 years. To
study the effect of iSGLT-2 on carbohydrate metabolism, lipid profile in type 2 diabetes
mellitus.
Results: By the 3rd month of treatment, there was a significant decrease in HbA1c
in the 1st and 2nd groups of patients. The decrease in HbA1c in the 1st group occurred
by 9.2% (P <0.05), in the 2nd group by 8.8% (P> 0.05), which is almost 2% lower.
The study of the lipid spectrum in the observed patients showed that when using
hypoglycemic therapy (metformin + iSGLT-2) after 3 and 6 months of therapy, a decrease
in the level of triglycerides by 9.8 and 14.1%, respectively, in total cholesterol by 15.4
and 9 , 8%, respectively, LDL-C - by 11.0 and 12.4%, respectively, and an increase in
cholesterol in HDL-C - by 32.0 and 41.8%, respectively (p <0.05).
Conclusion: Thus, in patients with type 2 diabetes with CKD G3a, the combination
of metformin and iSGLT-2a had a positive effect on the main indicators of carbohydrate
and lipid metabolism. This combination was more effective in improving lipid
metabolism in type 2 diabetes patients with CKD G3a compared with type 2 diabetes
patients with CKD G3b.
Abbreviations: DM: Diabetes Mellitus; CKD: Chronic Kidney Disease; DN: Diabetic Nephropathy; WHO: World Health Organization
Introduction
Diabetes mellitus (DM) is a global medical and social problem of
our time, which is faced by medical science and healthcare in almost
all countries of the world. The World Health Organization (WHO)
for the first time recognized this disease as a new non-infectious
epidemic of the 21st century, since in recent years the growth rate
of patients has become alarming [1]. The current constant increase
in the number of patients with type 2 diabetes unambiguously
affects the incidence of microvascular complications, including
diabetic nephropathy (DN). DN increases morbidity, disability and
mortality in type 2 diabetes patients. DN in parallel with diabetes
is a risk factor for the onset and progression of cardiovascular
diseases and one of the main factors of end-stage renal failure [2,3].
Type 2 diabetes increases the risk of chronic kidney disease (CKD) 2.6 times, and the risk of death due to kidney pathology - 3 times.
According to statistics, CKD develops in about 15% of individuals in
the general population and in every second patient with diabetes
mellitus (DM). In Uzbekistan, 118026 patients with CKD were
registered, in 2020 the number of patients with CKD was 23773 with
CKD, of which 5146 are on hemodialysis, about 40% are patients
with diabetes [2]. The leading role in the development of CKD in
patients with diabetes is played by permanent hyperglycemia.
Advances in the treatment of patients with diabetes mellitus
(DM) in recent years do not reduce the risk of chronic kidney
disease (CKD), but provide a delay in its development. Obesity
and the associated lipid metabolism disorder is a factor in the
progression of any kidney disease, including DN. Along with damage
to the mesangial and paramesangial regions of the glomerulus,
lipids filtered into the primary urine can also cause damage to the
cells of the renal tubules [3-5]. It has been shown that the lipid
profile shift characteristic of T2DM is chronologically ahead of the
development of carbohydrate metabolism disorders and confirms
the fact that lipotoxicity pathogenically precedes glucose toxicity
[6,7]. The most pronounced anti-lipolytic effect is possessed by
representatives of the gliflozin classes (iSGLT-2). Meanwhile, the
action of hypoglycemic drugs should also be considered from the
point of view of renoprotection and correction of cardiovascular
insufficiency [7].
Purpose of the Study
To study the effect of iSGLT-2 on the parameters of carbohydrate metabolism, lipid spectrum in patients with diabetic nephropathy.
Material and Research Methods
The prospective study included 80 patients with type 2 diabetes with DN. The duration of diabetes mellitus was on average 9.7 ± 0.9 years. To study the effect of iSGLT-2 on carbohydrate metabolism, lipid profile in type 2 diabetes mellitus, 2 groups were identified. Group 1 40 patients with type 2 diabetes with CKD G3a diabetic nephropathy, average GFR 56 ± 0.9 ml / min 72 m2, patients’ age was 56.8 ± 2.8 years, of which 18 were men and 22 women, as hypoglycemic therapy received metformin and a sodium-glucose cotransporter type 2 inhibitor (iSGLT-2) empagliflozin. Group 2 of 40 patients with diabetic nephropathy, the average age of patients was 58.3 ± 2.9 years, including 21 men and 19 women with CKD G3b, the average GFR was 40 ± 0.9 ml / min 72 m2. The studied groups of patients were comparable in terms of sex, age, duration and severity of diabetes mellitus. The patients were on a constant diet, and they were not prescribed hypolipidemic therapy. Glomerular filtration rate was determined using the CKD-EPI formula. Glycemia was determined on an automatic biochemical analyzer BS-380 “Mindray” by glucose oxidase method in venous blood on an empty stomach using HUMAN Glucose reagents (Germany). HbA1c was determined on a Huma Nex A1c analyzer. The lipid spectrum of blood was determined using kits from Cypress Diagnostics (Belgium) using a Hospitex Diagnostics spectrophotometer. Total cholesterol and triglycerides in blood serum were determined by a standard enzymatic method, HDL cholesterol in the supernatant was determined after precipitation of lipoproteins of other classes with dextran sulfate. LDL cholesterol values were calculated according to the formula of W. Friedwald (1972): LDL cholesterol = total cholesterol - (TG / 2.2 + HDL cholesterol), mol / l. Control studies of the studied parameters were carried out after 3 and 6 months.
Research Results and their Discussion
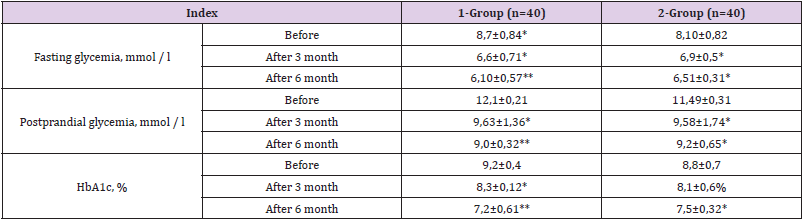
Studies have shown that the baseline indicators characterizing glycemia (fasting glycemia, postprandial glycemia and HbA1c%) in the studied groups were comparable (Table 1). By the 3rd month of treatment, there was a significant decrease in HbA1c in the 1st and 2nd groups of patients. The decrease in HbA1c in the 1st group occurred by 9.2% (P <0.05), in the 2nd group by 8.8% (P> 0.05), which is almost 2% lower. The initial indicators of fasting glycemia and postprandial glycemia in the 1st group did not significantly exceed the indicators of the 2nd group (8.7 ± 0.84 mmol /l and 8.10 ± 0.82 mmol /l, respectively; 12.1 ± 0, 21 mmol /l and 11.49 ± 0.31 mmol /l, respectively), after 3 months these indicators significantly decreased in the 1st group by 24.9% and 19.8%, respectively, in relation to the initial data, in the 2nd group, the decrease was significantly lower - 14.1% and 16.8%, respectively. In the dynamics of treatment, after 3 and 6 months, there was a pre-delivery decrease in the studied parameters of carbohydrate metabolism in both groups of patients. So, the level of postprandial glycemia within 6 months in both the 1st and 2nd groups significantly decreases in relation to the initial data, in the 1st group - by 25.6% and by 19.9% (P < 0.05). The HbA1c content after 6 months decreased by 25% in the 1st group of patients with type 2 diabetes and by 10.2% in the 2nd group (P <0.05). Episodes of hypoglycemia were not observed in both groups. By the 6th month of observation, it should be noted that the glycated hemoglobin indicators reached the target values in patients with diabetic nephropathy (Table 2).
Table 1: Dynamics of carbohydrate metabolism indicators in the treatment groups at baseline and after 3 (M ± m).
Note: * p <0.001, ** p <0.05
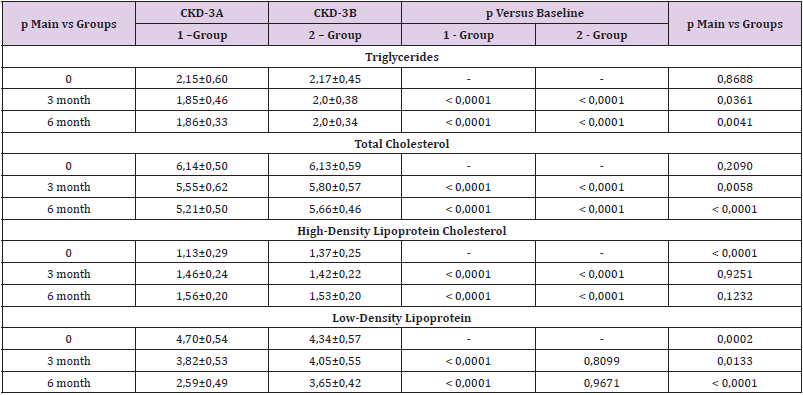
Table 2: Influence of the appointment of sodium glucose cotransporter type 2 inhibitors (iSGLT-2) on the lipid profile in DN.
The study of the lipid spectrum in the observed patients showed that when using hypoglycemic therapy (metformin + iSGLT-2) after 3 and 6 months of therapy, a decrease in the level of triglycerides by 9.8 and 14.1%, respectively, in total cholesterol by 15.4 and 9,8%, respectively, LDL-C - by 11.0 and 12.4%, respectively, and an increase in cholesterol in HDL-C - by 32.0 and 41.8%, respectively (p <0.05). At the same time, the TG level was slightly changed and remains within the normal range in all the studied groups. The data obtained indicate that TG should be determined with reference or slightly increased levels of TG and LDL in patients with type 2 diabetes in patients with DN. In the 1st group of patients, there is a decrease in TG 8,6%, and HDL 38,1% increases. In group 2, the dynamics of TG, HDL was less pronounced: TG decreased 9,2%, HDL increased 11,1%. Thus, it should be emphasized that the first group of patients with type 2 diabetes with CKD G3a achieved a more favorable lipid spectrum in general, TG and HDL parameters were close to the target values in this category of patients. In the second group, patients with type 2 diabetes with CKD G3b also showed a decrease in TG, but less pronounced, the level of HDL was achieved the target values in this category of patients. The lack of significant dynamics of LDL in both groups is possibly due to the lack of special lipid-lowering therapy.
Discussion
Advances in the management of patients with DM in recent years do not reduce the risk of CKD, but provide a delay in its development [4,5]. Along with damage to the mesangial and paramesangial regions of the glomerulus, lipids filtered into the primary urine can also damage the cells of the renal tubules. Lipoproteins deposited in the renal tissue bind negatively charged glycosaminoglycans, there by neutralizing its negative charge and increasing its permeability to proteins [7,8]. Damage to the renal tubules is associated with intense lipid reabsorption and metabolism by nephrocytes, which leads to the release of lysosomal enzymes, cytotoxic effect and subsequent sclerosis. In turn, proteinuria is one of the most studied risk factors for the progression of renal disease [7]. The strategy and therapeutic goals, including those for indicators of lipid metabolism in patients with diabetes, have been determined. In recent years, special attention in diabetology has been paid to inhibitors of the sodium-glucose cotransporter 2 (iSGLT-2). These drugs, in addition to successful glycemic control, have a positive effect on renal function in individuals with type 2 diabetes and CKD [9], they also have positive metabolic effects, but also the ability to correct hemodynamic disorders, reducing intraglomerular hypertension and systemic arterial pressure, which can potentially have a nephroprotective effect. The mechanism of the effect of iSGLT-2 on lipid metabolism is not fully understood, according to the data, a potential mechanism of action of SGLT2 inhibitors may be an increase in the metabolism of LDL, but this fact has been shown in rats [9,10]. So, the main mechanism for reducing the fat content in the liver under the action of iSGLT2 inhibitors is a decrease in de novo lipid synthesis by reducing the level of glycemia and insulin and an increase in beta-oxidation of fatty acids.
Conclusion
Thus, in patients with type 2 diabetes with CKD G3, the combination of metformin and iSGLT-2 a had a positive effect on the main indicators of carbohydrate and lipid metabolism. This combination was more effective in improving lipid metabolism in type 2 diabetes patients with CKD G3a compared with type 2 diabetes patients with CKD G3b.
References
- Dedov II, Shestakova MV, Vikulova OK (2017) Epidemiology of diabetes mellitus in Russian Federation: clinical and statistical report according to the federal diabetes registry. Diabetes mellitus 20(1): 13-41.
- Alieva AV, Ismailov SI, Rahimova GN (2018) Epidemiology of diabetes and prediabetes in Uzbekistan: Screening results. Health Sci J 12(6): 609-614.
- Sowers KM, Javad Habibi, Melvin R Hayden (2017) Diabetic nephropathy and tubulointerstitial fibrosis in cardiometabolic syndrome and type 2 diabetes mellitus. J Cardiometab Syndr 2(2): 143-148.
- Miguel Ángel Salinero Fort, Francisco Javier San Andrés Rebollo, Carmen de Burgos Lunar, Juan Carlos Abánades Herranz, Enrique Carrillo de Santa Pau, et al. (2016) Cardiovascular and all-cause mortality in patients with type 2 diabetes mellitus in the madiabetes cohort study: association with chronic kidney disease. Diabetes Complications 30(2): 227-236.
- Volker Vallon, Scott C Thomson (2012) Renal function in diabetic disease models: the tubular system in the pathophysiology of the diabetic kidney. Annu Rev Physiol 74: 351-375.
- Li Z, Hongyang Liu, Zhangjing Niu, Wen Zhong, Miaomiao Xue, et al. (2018) Temporal Proteomic Analysis of Pancreatic β-Cells in Response to Lipotoxicity and Glucolipotoxicity. Molecular and cellular proteomics 17(11): 2119-2131.
- Wang D, Luo Y, Wang X, David J Orlicky, Komuraiah Myakala, et al. (2018) The sodium-glucose cotransporter 2 inhibitor dapagliflozin prevents renal and liver disease in western diet induced obesity mice. Int J Mol Sci 19(1): 137.
- Yu T, Sungelo MJ, Goldberg IJ, Wang H, Eckel RH (2017) Streptozotocin-Treated High Fat Fed Mice: A New Type 2 Diabetes Model Used to Study Canagliflozin-Induced Alterations in Lipids and Lipoproteins. J Horm Metab Res 49(05): 400-406.
- Vallon V, Thomson SC (2017) Targeting renal glucose reabsorption to treat hyperglycemia: the pleiotropic effects of SGLT2 inhibition. Diabetologia 60(2): 215-225.
- Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ (2016) Sodium glucose cotransporter 2 inhibitors in the treatment of diabetes mellitus: cardio-vascular and kidney effects, potential mechanisms, and clinical applications. Circulation 134(10): 752-772.

 Review Article
Review Article