ABSTRACT
Background: Intradural pressure increases in patients with intracerebral (ICH) and subdural (SDH) hemorrhage. This should be treated immediately to prevent secondary brain injury due to ischemia. Hyperosmolar fluids can be used to manage intradural pressure. Hypertonic sodium lactate (Totilac®) contains lactate which is considered to provide energy supplementation for ischemic brain. The combination of hyperosmolar properties with lactate in Totilac® is expected to have a better effect on reducing intradural pressure.
Objective: to compare the intradural pressure after Mannitol® and Totilac® administration for patient who underwent craniotomy of hematomal evacuation.
Methods: The study subjects were allocated into two groups using permuted block techniques randomization. Group M received mannitol®, whereas group T had Totilac®. Intradural pressure measurement was performed by the surgeon through puncture using needle no.23 connected to an invasive monitor device when the duramater was still intact. The intradural pressure was measured when opening the cranium as a baseline, 5th, 10th and 15th minutes after hypertonic solution administered.
Results: Twenty-four patients underwent hematomal evacuation craniotomy of ICH and SDH at the emergency surgery room. There were significant decreases of intradural pressure at the 5th, 10th, and 15th minute after hypertonic solution administered in each group compared to baseline when the cranium was opened. The change from baseline in intradural pressure between groups at 5th, 10th, 15th minute after hypertonic solution administered were similar.
Conclusion: There was no additional benefit in intracranial pressure control after administration of Totilac® compared to Mannitol administration for patients undergoing craniotomy of hematomal evacuation.
Keyword: Mannitol; Totilac; Intradural Pressure; Hematomal Evacuation; Craniotomy; Anaesthesia
Background
Hemmorhage cerebral injury requires management to control the increase in intracranial pressure (ICP), including the surgical strategy and administration of hyperosmolar solution [1]. The hyperosmolar solution that has been widely used is mannitol 20% (Mannitol®). Mannitol® increase diuresis directly in the loop of Henle. Hypertonic sodium lactate (Totilac®), a relatively new hyperosmolar solution, can be used as an alternative in the management of increased ICP [2]. Besides having an higher osmotic reflection coefficient (σ), [3] the lactate content can theoretically be an energy source for ischemic brain cells [4]. Totilac® has the potential to increase diuresis indirectly by increasing intravascular volume [5]. From these properties, totilac® with the basic component of hypertonic saline, is considered superior in maintaining intravascular volume compared to mannitol®. Therefore, we want to compare the intradural pressure profile after administration of Totilac® and Mannitol® in patients undergoing hematomal evacuation craniotomy.
Methods
The study was conducted at a tertiary care hospital during April-July 2018. The study was approved by the Medical and Health Research Ethics Committee of FKKMK UGM and Dr. Sardjito Hospital. Informed consents were acquired from all subjects before participating in this study. The patients included for the study aged 18-65 years and who underwent emergency hematomal evacuation craniotomy for indications of intracerebral hematoma (ICH) or subdural hematoma (SDH). The exclusion criteria were unresolved shock, ongoing massive bleeding, allergic to lactate, impaired renal function, hyponatremia [Na+] <130 meq / L, hypernatremia [Na+]> 150 meq / L, history of uncontrolled diabetes mellitus, history of uncontrolled hypertension. The study subjects were allocated into two groups using permuted block techniques randomization. Group M received mannitol®, whereas group T had Totilac®. The allocated group information was given in a sealed envelope when the patient arrived at the surgery room. In operating room, Anaesthesia was induced with 2.5 mg of midazolam, fentanyl 2 mcg/kg, propofol 2 mg/kg, lidocaine 1.5 mg/kg, and rocuronium 0.6-1 mg/kg for tracheal intubation.
Anaesthesia was maintained with sevoflurane 2% with delivery gas of FiO2 50%. The depth of anesthesia was monitored by maintaining bispectral index value between 40-60. Controlled ventilation was set with a tidal volume of 6-8 ml/kg, PEEP 3-5, a minute volume of 80-120 ml/kgBW/ minute and a maximum peak inspiratory pressure of 30 mmHg. Maintenance fluid was given according to the needs of patients with a composition of 0.9% NaCl:RL = 3: 1. Blood lost was replaced with colloids with the same volume. Blood component was given if the bleeding exceeded maximum allowable blood lost. Another crystalloid was given to replace the urine output with 2/3 of the volume of it. Baseplate of invasive monitor were placed at the level of the tragus, following changes in the position of the patient. Invasive monitors were prepared with CVP mode on a scale of 0-30 and being zeroed every time a subject changes position. Intradural pressure measurement was performed by the surgeon through puncture using needle no.23 when the duramater was still intact.
The needle was placed in the subdural space parallel to the duramater then was connected to an invasive monitor device. The intradural pressure, hemodynamic and other parameters are measured when opening the cranium as a baseline, 5th, 10th and 15th minutes after hypertonic solution administered by rezeroing before recording the value. Analyses were done on all subjects who had received treatment according to the protocol. Data were expressed in terms of numbers and percentages, mean and standard deviations. The data between the two groups were analyzed for differences using independent t‑tests or paired t-test for numerical data and Chi square tests for categorical data. Data were analysed using SPSS 24 software computer program.
Results
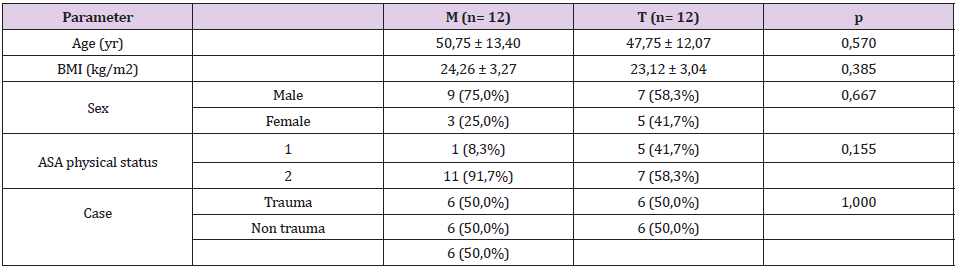
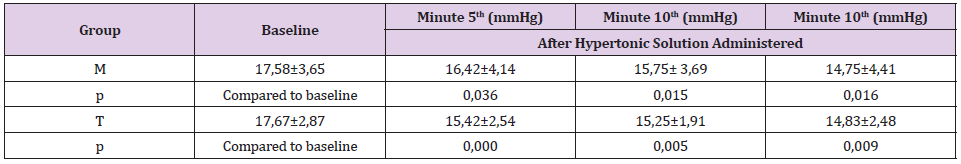
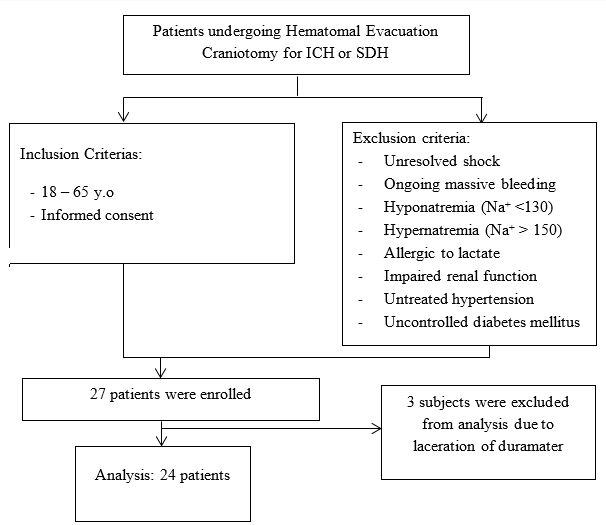
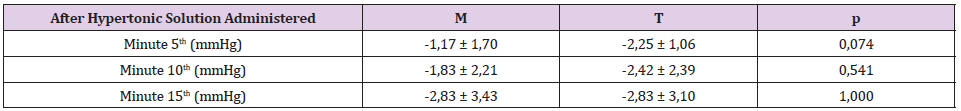
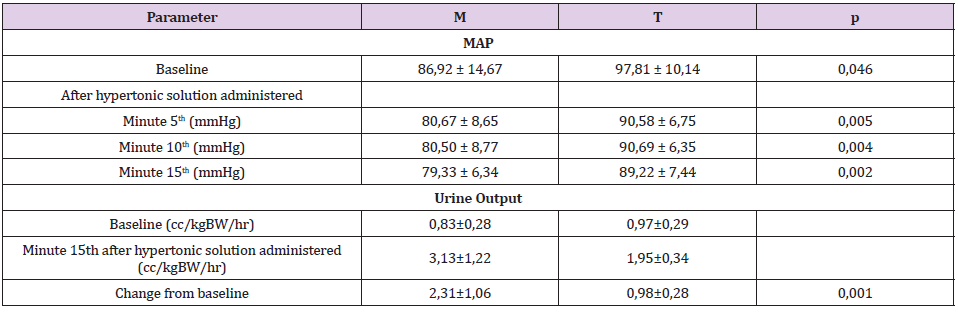
A total of 27 patients were assessed for eligibility for this study. Randomization was performed on 27 patients. As shown in Figure 1, 3 subjects were excluded from analysis because of unable to follow the study procedure due to laceration of duramater during craniotomy. One-third of subjects are women as shown in Table 1. The average age of the subjects in group M was 50.75 + 13.4 years and in the T group it was 47.75 + 12.07, which was not difference significantly. There was no difference in the ratio of BMI and physical status based on ASA physical status (p= 0.667 and 0.155, consecutively). The distribution of trauma and non-trauma cases was also balanced in both groups. The level of brain relaxation was assessed in this study by measuring intradural pressure. Table 2 shows significant decreases of intradural pressure in the 5th, 10th and 15th minute after hypertonic solution administered in each group compared to baseline when the cranium was opened. Table 3 shows the change from baseline in intradural pressure between groups at 5th, 10th, 15th minute after hypertonic solution administered were similar. The difference in MAP between groups was found to be significant at all periods of measurement, as shown in Table 4. Group M has higher change from baseline of urine production at the end of observation compared to group T, as shown in Table 4.
Discussion
In this study, there was a significant decrease in intradural pressure in each group. It is well known that Mannitol® and hypertonic sodium lactate solutions with its hyperosmolar properties are part of ICP control management. The most significant decrease in group M occurred in the 10th minute after the cranium was opened, whereas the T group experienced the highest difference in the 5th minute after the cranium opened. This shows a different peak onset difference in each solution, although it is stated that Mannitol® peak onset and hypertonic sodium lactate solution are almost correspondent (15-20 minutes) [5]. Properties of hypertonic sodium lactate solutions that draw fluids from interstitial to intravascular be superior in controlling cerebral edem because its reflection coefficient is greater than Mannitol [5]. A study by Hisam, et al. showed hypertonic sodium lactate had a significantly better brain relaxation effect than Mannitol® assessed from a comparison of brain relaxation assessed subjective when an open cranium with BRS in COT [6].
Sokhal, et al. found that there was a significant difference in the decrease of intradural pressure in both groups with tumor removal craniotomy, but brain relaxation assessed by operators with the BRS method in the study did not differ significantly between the two groups. In this study, the difference in intradural pressure was not linearly related to brain relaxation that occurred, because the determinant component of ICT was not only from brain relaxation, where large tumor mass and intravascular volume also played a role in determining intradural pressure [7]. Previous studies conducted by Sharma, et al. the number of samples of 31 subjects who underwent aneurysm repair surgery also showed a meaningless difference in the decrease in intracranial pressure between groups M and T [8] this result is due to the aneurysm surgery itself the incidence of extravasation of fluid is not promising. Wirawijaya, et al. revealed no significant differences in brain relaxation in patients with craniotomy surgery to remove tumors that received 3% NaCl, Mannitol, and hypertonic sodium lactate [9].
In addition, nutritional support in the form of exogenous lactate that can be a source of energy in injured cells also decreases the progression of intersective edema resulting from cell death [2,10]. The study conducted by A Daniel (2014) states that lactate supplementation is an important component in brain metabolism that is experiencing injury, especially in the penumbra region that has the potential to experience cellular death [11]. Hamzah, et al. showed that ATP biomarkers in experimental animal models that experienced ICH experienced a significant increase in the administration of hypertonic sodium lactate solution compared to Mannitol® and NaCl 3%. The study also suggested that the comparison of the area of necrosis in the animal brain was significantly different, whereas in the hypertonic sodium lactate group it was much smaller than in the Mannitol® group, with p = 0,000.10 but they did not mention the correlation between the two findings.
The effect of diuretic Totilac® solution on the results of the study was significantly lower than Mannitol®. Previous research also showed similar results [6-9]. This was due to the Mannitol® properties acting in the loop Henle which resulted in increased urine production. In contrast to hypertonic sodium lactate, the diuretic effect is a result of increased intravascular volume, so that increased urine production is not a direct influence on the organ of urine formation. Based on this, hypertonic sodium lactate is a better choice in patients with intravascular volume disorders, because the diuretic effect of hypertonic sodium lactate will not appear in conditions of hypovolemia or dehydration [5]. The results of the insignificant decrease of intradural pressure in this study can be caused by the duration of the onset of the incident until the intervention was performed. In addition, the possibility of still active bleeding also affects intradural pressure. Even though brain relaxation has been achieved, the addition of volume in the third space can also increase intradural pressure. We could not manage this parameter and analyze it because we could not evaluate hematoma enhancement during surgery.
For the next research, it is necessary to do a comparative test of quantitative assessment methods using invasive monitors with BRS. A comparative study of the size of the needles used also needs to be done, so that it can avoid the possibility of blockages and clinging during the measurement period while not causing premature trauma to the dura mater. The use of invasive monitor equipment in this study is still relatively new even though it has been proven to determine the magnitude of pressure on other body locations. The use of needle number 23 can still allow for blockages and slacking during the measurement period.
Conclusion
Totilac® administration had similar intradural pressure profile effect compared to Mannitol® in hematomal evacuation craniotomy case.
References
- Peter S Amenta, Jacques J Morcos (2017) Nonlesional Spontaneous Intracerebral Hemorrhage. [book auth.] H. Richard Winn. Youmans and Winn Neurological Surgery (7th). Philadelphia: Elsevier.
- Carole Ichai, Guy Armando, Jean Christophe Orban, Frederic Berthier, Laurent Rami, et al. (2009) Sodium Lactate Versus Mannitol® in the Treatment of Intracranial Hypertensive Episodes in Severe Traumatic Brain-injured Patients. Care Med 35.
- Samir H Haddad, Yaseen M Arabi (2012) Critical Care Management of Severe Traumatic Brain Injury in Adults. BioMed Central.
- Pierre Bouzat, Nathalie Sala, Tamarah Suys, Jean Baptise Zerlauth, Pedro Marques Vidal, et al. (2014) Cerebral Metabolic Effect of Exogenous Lactate Supplementation on the Injured Human Brain., Berlin : Intensive Care Med 40: 412-421.
- Wendy C Ziai, Thomas JK Toung, Anish Bhardwaj (2017) Hypertonic Saline: First-line Therapy for Cerebral Edema? J Neurol Sci 261.
- Muhammad Yusuf Hisam, Sudadi, Sri Rahardjo (2015) Perbandingan Pemberian Mannitol® 20% Dosis 0,5 g/kgBB dengan Natrium Laktat Hipertonik Dosis 1,5 ml/kgBB Terhadap Efek Relaksasi Otak pada Pasien Cedera Otak Traumatik yang Dilakukan Kraniotomi. Jurnal Komplikasi Anestesi.
- Navdeep Sokhal, Girija Prasad Rath, Arvind Chaturvedi, Manmohan Singh, Hari Hara Dash (2017) Comparison of 20% mannitol® and 3% hypertonic saline on intracranial pressure and systemic hemodynamics.Journal of Clinical Neuroscience.
- Shalini Sharma, Vinod K Grover, Preethy J Mathew (2015) Mannitol® versus Hypertonic Saline for Intra-operative Brain Relaxation during Aneurysm Surgery. Journal of Neuroanesthesiology and Critical Care 2: 23-27.
- Dear Mohtar Wirawijaya, Ruli Herman Sitanggang, Tatang Bisri (2018) Perbandingan Mannitol® 20%, NaCl 3%, dan Natrium Laktat Hipertonik Terhadap Osmolaritas dan Brain Relaxation Score Pasien Tumor Otak yang Menjalani Kraniotomi Pengangkatan Tumor. Jurnal Neuroanestesi Indonesia, p. 1-10.
- Hamzah, Nancy Margarita Rehatta, Tatang Bisri, Siti Chasnak Saleh, Arie Utariani (2019) Lactic Acid's Role in Sodium hypertonic Lactic Solution As Neuroprotector Measured from the Level of ATM, MCT-1, and Necrosis Area In Intracerebral Hematoma Rats Model. Critical Care and Shock.
- A Dienel Gerald (2014) Lactate shuttling and lactate use as fuel after traumatic brain. Journal of Cerebral Blood Flow & Metabolism, pp. 1736-1748.

 Research Article
Research Article