ABSTRACT
Objectives: Multifocality is one of the prominent characteristics of papillary thyroid cancer (PTC), however the management strategy for multifocal PTC remains controversial. Moreover, evaluation of impact of multifocality in a quantitative way rather than a qualitative way still needs to be elucidated.
Patients and Methods: Medical records of 1034 patients with PTC who underwent total or hemi-thyroidectomy were reviewed at the authors’ institution between April 2013 to September 2013. The laterality, number and size of each tumor foci, number of levels Ⅵ lymph nodes metastasis (LNM) and other potential risk factors were recorded. Results: Male gender, tumor size larger than 1cm, multifocality, diffuse calcification were risk factors for level Ⅵ LNM by univariant and multivariable analysis. Moreover, level Ⅵ LNM rate is increased proportionally with the increasing number of foci. The LNM rate is 102/474 (21.5%), 46/135 (34.1%), 14/35 (40%), and 4/7 (57.1%) for unilateral PTMC patients with 1 to 4 foci, and 15/30 (50%), 15/24 (62.5%), 7/10 (70%), 5/6 (83.3%), 2/2 (100%) for bilateral PTC patients with 2 to 6 foci. Interestingly, we found that the LNM rate for multifocal PTMCs (6mm≤largest diameter≤10mm) is comparable to unilateral unifocal PTCs (largest diameter >1cm, 52/122, 42.6%, vs. 21/58, 36.2%; P=0.413). Conclusion: Our study suggests that multifocality as a sign of a higher propensity for lymph node metastasis. Multifocal PTMC with 6mm≤largest diameter≤10mm should be treated with caution considering the possible high lymph node metastasis rate.Keywords: Papillary Thyroid Microcarcinoma; Multifocality; Lymph Node Metastasis
Introduction
The incidence of papillary thyroid carcinoma (PTC) has
increased in a dramatic pattern in recent years [1,2]. PTC often
presents with multifocal tumors, i.e., presence of two or more
non-contiguous tumor foci either unilaterally or bilaterally, which
is one of the most prominent characteristics of PTC. It is well
established that multifocality represents a higher propensity for
a more advanced staging, and multifocality per se is a qualitative
parameter to assess the risk for LNM. However, it is not easy to
quantify its effects on pathological outcome and clinical features. The prevalence of the multifocal PTC ranged from 32% to 39% in
large series of PTC [3-5]. In clinics, multifocality is often empirically
treated as a high-risk factor for aggressiveness of PTC and reported
to be associated with extensive LNM [4], higher recurrence rate
[5], and more aggressive biological behavior [6,7], compared
with unifocal PTC. However, inconsistent and even contradictory
findings also exist [4,8,9]. It is well accepted that active surveillance
should be recommended to patient with microcarcinoma at low
risk. However, a clinical dilemma is how do physicians handle with
multifocal microcarcinoma which all the foci are less than 1cm
in diameter. In other words, whether multifocality could be used
as a quantified parameter rather than a qualitative parameter
need to be addressed. Moreover, although prophylactic central
compartment neck dissection is not routinely recommended
according to ATA guidelines, insidious LNM do exist and be the
cause for the recurrence of PTC. Thus, is it safe to recommend not
receiving central compartment neck dissection for all patients with
multifocal papillary thyroid microcarcinoma?
In this study, we retrospectively analyzed 1034 patients with
papillary thyroid carcinoma to evaluate the how the multifocality
affects the central compartment LNM and try to quantify the
multifocality to further predict the possible insidious central
compartment LNM.
Material and Methods
Patients
Patients diagnosed with papillary thyroid cancer (classic type) between April 2013 to September 2013 in Tianjin Medical University Cancer Institute and Hospital were recruited. Medical records, ultrasonographic and histopathological reports were reviewed. Patients with histological variant (follicular, tall cell, trabecular or others) or patients whose tumor is in the isthmus were not included. Sex, age, tumor size, bilateral disease, tumor foci number, and cervical LNM were determined in each patient. Ethics approval was obtained from The Institutional Review Board of Tianjin Medical University Cancer Institute and Hospital (approval: BC2021023), and the requirements for patient approval and informed consent were waived because of the retrospective nature of the study.
Data Collection/ Definition of Parameter
Bilateral disease was defined as the presence of PTC foci in the right and left lobes of the thyroid gland. The size of the largest focus of PTC was used for analysis. Multifocal disease was defined as the presence of two or more foci of PTC.
Determination of Number of Tumor Foci and Tumor Size
To define the number tumor foci and tumor diameter of each tumor, ultrasonographic and histopathological reports were reviewed by two independent researchers. The number of tumor foci is determined according to the histopathological reports. As for each tumor’s largest diameter, we refer to the ultrasonographic reports for each tumor and record its ultrasonographic diameter. The largest diameter is recorded if three-dimensional data is given by the ultrasonographers.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows v21 (IBM Corp., Armonk, NY). Univariate analysis was performed using Chi-squared test or Fisher’s exact tests for categorical variables, Student’s t-tests for normally distributed data, and Mann–Whitney U-tests for continuous variables that were not normally distributed. Cox regression analyses was used for univariate and multivariate analysis. All p-values represented were two-sided and considered statistically significant when p<0.05.
Results
Clinical and Pathological Features
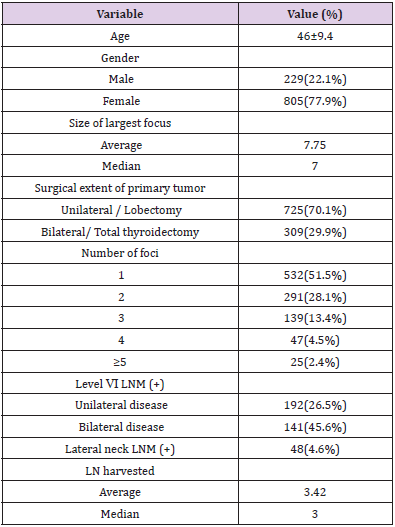
A total of 1034 patients were diagnosed as PTC or PTMC in our department during April 2013 to September 2013. The mean age was 46 years (range, 18-76), of which 229 (22.1%) were male and 805 were female (77.9%). The median tumor size was 7mm (range, 1-45). Multifocal cancer lesions were found in 502 patients (48.5%), in which the number of patients with 2 to 4 foci were 291(28.1%), 139(13.4%), and 47(4.5%), respectively, with 25(2.4%) patients with ≥5 foci. Of all the multifocal PTMCs, 273 (57.2%) were bilateral and 177 (42.8%) were unilateral. The level Ⅵ LNM rate for unilateral and bilateral cancer patients were 26.5% and 45.6%, respectively. The clinical and pathological features of these patients were summarized in Table 1.
Factors Associated with Central Compartment LNM
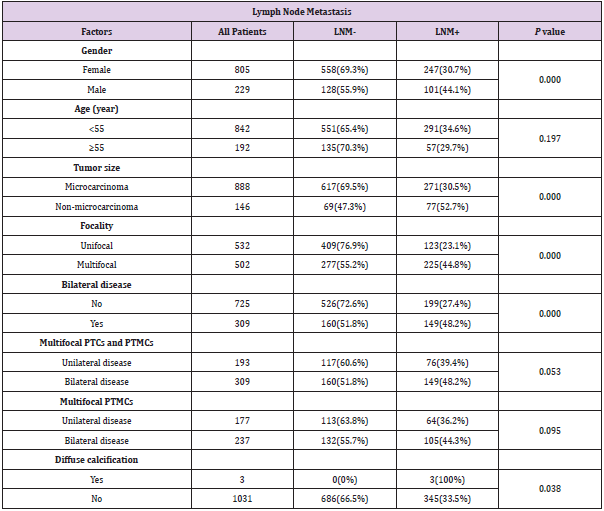
Univariate analysis was done to assess the risk factors of central
compartment LNM. As for all the patients included, male gender,
tumor size larger than 1cm, multifocality, bilateral disease, diffuse
calcification were risk factors for central compartment LNM Table 2.
Interestingly, when multifocal diseases were considered (including
both multifocal PTCs and multifocal PTMCs), bilateral disease was
no longer a risk factor (P=0.053, P=0.095, respectively). We then
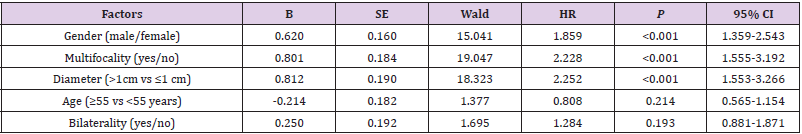
calculated the independent risk factor for LNM by multivariate
analysis, we found that male gender, multifocality, diameter
larger than 1cm, diffuse calcification on ultrasonography are all
independent risk factors for LNM. However, age and bilaterality are
not independent risk factors for LNM Table 3.
Central compartment LNM rate is associated with multifocality
irrespective of unilateral or bilateral disease.
In PTCs that larger than 1cm in diameter, the LNM rate of unifocal PTC is 36.2% (21/58), whereas the LNM rate of multifocal PTC is much higher at 63.6% (56/88, P=0.001). We then analyzed the effect of bilaterality on central compartment LNM. Of note, the LNM rate of unilateral multifocal PTC is 75% (12/16), which is comparable to the LNM of bilateral multifocal PTC 61.1% (44/72, P=0.296). Similar results were observed in PTMC patients. The LNM rate of unifocal PTMC is 21.5% (102/474), whereas the LNM of multifocal PTMC is 40.8% (169/414), in which LNM of unilateral multifocal PTMC is 36.2% (64/177), which is comparable to the LNM rate of bilateral multifocal PTMC 44.3% (105/237, P=0.095), as summarized in Table 2.
Table 2: Factors predictive of lymph node metastasis in the univariable analysis.
Abbreviations: PTMC, papillary thyroid microcarcinoma; PTC, papillary thyroid carcinoma; LNM, lymph node metastasis.
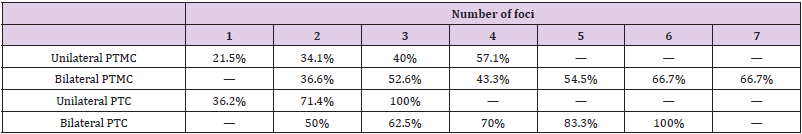
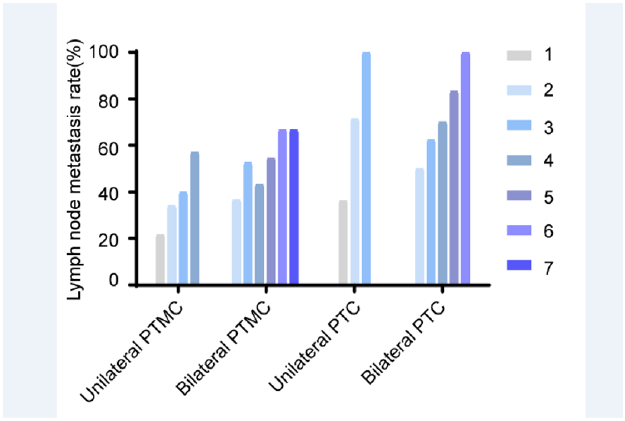
Number of Foci Increases the LNM Rate
The above results showed that multifocality is a risk factor for increased LNM rate irrespective of unilateral or bilateral disease. This finding suggests that multifocality might be interpreted in the setting of one “thyroid lobe”, rather than “one thyroid gland”. Thus, the effect of the number of PTC foci on central compartment LNM was further examined. As shown in Table 4, for all the unilateral PTMC, 102 of 474 (21.5%) patients with unifocal PTMC had level VI lymph node metastases. Whereas 46/135 (34.1%) patients with two foci of PTMC were found to have positive lymph nodes. The proportion of patients with positive level VI nodes increased in the group with three foci, where 14/35 (40%) patients were found to be positive. In patients with 4 foci, 4/7 (57.1%) were found to have positive lymph nodes in level VI. Interestingly, a gradual increase in LNM proportion is observed, with respect to foci number, as displayed in Figure 1. In bilateral PTMC patients, 41 of 112 (36.6%) patients with two foci bilateral PTMC had level VI lymph node metastases. Whereas patients with 3 to 7 foci of bilateral PTMC were found to have positive LNM were 41/78 (52.6%), 13/30 (43.3%), 6/11 (54.5%), 2/3(66.7%), 2/3(66.7%), respectively.
Table 4: Lymph node metastasis rate at various number of foci.
Abbreviations: PTMC, papillary thyroid microcarcinoma; PTC, papillary thyroid carcinoma
Figure 1: Central lymph node metastasis rate is increased with respect to increased foci number. For all unilateral or bilateral PTMCs and PTCs, the LNM rate is increased in accord with the increased foci number.
A similar result was also observed in PTC patients with largest diameter larger than 10mm. As for unilateral PTC patients with largest diameter larger than 10mm, the LNM proportion is 21/58 (36.2%), 10/14 (71.4%) and 2/2 (100%) for unilateral PTC patients with 1 to 3 foci. For bilateral PTC patients with largest diameter larger than 10mm, the LNM proportion is 15/30 (50%), 15/24 (62.5%), 7/10 (70%), 5/6 (83.3%), 2/2 (100%) for bilateral PTC patients with 2 to 6 foci Table 4.
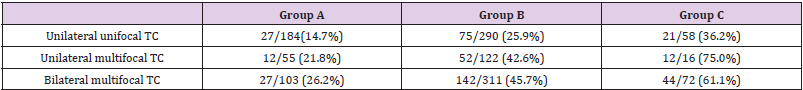
LNM Rate for Multifocal PTMC Is Comparable to Unifocal PTC When Ptmcs Largest Diameter is Between 6-10 mm
To further assess the effect of multifocality on LNM, patients were stratified according to the largest diameter. Patients were divided into three groups: A. largest diameter is ≤5mm; B. 6mm≤largest diameter≤10mm; C. largest diameter >10mm. As shown in Table 5, in group A, the LNM proportion in unilateral unifocal PTMC, unilateral multifocal PTMC and bilateral multifocal is 27/184 (14.7%), 12/55 (21.8%) and 27/103 (26.2%). In group B, the LNM proportion in unilateral unifocal PTMC, unilateral multifocal PTMC and bilateral multifocal is 75/290 (25.9%), 52/122 (42.6%) and 142/311 (45.7%). In group C, the LNM proportion in unilateral unifocal PTC, unilateral multifocal PTC and bilateral multifocal PTC is 21/58 (36.2%), 12/16 (75.0%) and 44/72 (61.1%). For unilateral PTMCs and PTCs, the LNM proportion in patients from group A, B and C were 12/55 (21.8%), 52/122 (42.6%) and 12/16 (75%). For both unilateral and bilateral PTMCs and PTCs, the LNM proportion in patients from group A, B and C were 27/103 (26.2%), 142/311 (45.7%) and 56/88 (63.6%). Interestingly, when we compare the risk of LNM for multifocal PTMCs, we found that the LNM rate for multifocal PTMCs in group B (6mm≤largest diameter≤10mm) is comparable to unilateral unifocal PTCs whose largest diameter is greater than 1cm (52/122, 42.6%, vs. 21/58, 36.2%; P=0.413), indicating that multifocal PTMCs might have the same propensity to LNM with unifocal PTC which largest diameter is greater than 1cm.
Table 5: Lymph node metastasis rate according to largest tumor diameter.
Group A: PTMC’s largest diameter is ≤5mm; Group B: 6mm≤largest diameter≤10mm; Group C: largest diameter >10mm.
Abbreviations: TC: thyroid cancer
Discussion
Previously, multifocality has been implicated as a qualitative
parameter to assess the risk for central compartment LNM.
However, few studies have shown how the number of foci affect the
LNM. In this study, the risk factors for lymph node metastasis were
studied, then the effect of multifocality was further investigated
between the number of PTC foci and LNM to central compartment.
Multifocality is a common clinical characteristic of PTC and has
been reported in 18–87% of patients with PTC [10] and was seen
in 48.5% of patients in the present study. Our results show that the
risk of level VI lymph metastasis increases proportionally with the
number of tumor foci, both in PTMCs and PTCs which diameter is
larger than 1cm. When the number of foci reaches 3 or more, the
level VI LNM rate exceeds 50% or higher (52.6% and 62.5% for
bilateral PTMC and bilateral PTC). And even 100% in the presence
of 6 foci. Ayham et al reported a similar result in the presence of
3 or more foci, except that no appreciable difference in level VI
lymph node metastasis in patients with one and two foci [11].
These findings identify multifocality in PTC as an indicator of tumor
aggressiveness, manifesting in a higher propensity for locoregional
metastasis.
Both univariate and multivariate analysis identified male
gender, tumor size larger than 1cm, multifocality, diffuse
calcification as significant predictors of level VI lymph node metastasis in the study population. These findings are consistent
with previously published studies identifying risk factors for level
VI metastasis in PTC [12-14]. Of note, our data indicated a rare
phenomenon diffuse calcification as significant predictors of level
VI lymph node metastasis. Diffuse calcification has been implicated
with thyroid malignancy [15,16]. In our study, the LNM rate for
the PTC with diffuse calcification is 3/3 (100%), although the
case number is small, it still strongly indicates that PTC patients
with diffuse calcification under ultrasonography has a higher
propensity for locoregional metastasis. Another interesting finding
is that, when we compare the LNM rate between multiple PTMCs
(6mm≤largest diameter≤10mm) and unifocal PTC which diameter
is larger than 1cm, there is no significant difference between these
two groups. This finding indicates that multifocal PTMCs with
6mm≤largest diameter≤10mm has the same propensity for LNM
in central compartment, compared with unifocal PTC with largest
diameter ≥10mm. Other studies have shown concordant result that
multifocal PTMC with relative bigger foci is at higher risk of LNM
although it might not be clinically evident. Zhao et al. has proposed
the concept of aggregate diameter (AD) to better assess the tumor
burden [17,18]. Abbas et al. also pointed out that the sum up of
the diameter of each tumor foci >10 mm confers a similar risk of
aggressive histopathological behavior with unifocal PTC greater
than 10 mm [19].
In conclusion, this study provides evidence that multifocal PTCs
are at higher risk of LNM, which tendency might increase in the
presence of over 4 foci when compared with unifocal and bifocal
disease. In addition, multifocal PTMCs with largest foci between
6mm to 10mm might have the same tendency to PTC which
diameter is >10 mm. Thus, multifocal thyroid PTMCs should not
be managed as conventional PTMCs at low risk, thereby prompting
more aggressive treatments.
Acknowledgments
This work was partially supported by grants from National Natural Science Foundation of China (Grant Nos. 81872169), Tianjin key research and development program science and technology support key projects (Grant No. 17YFZCSY00690), Tianjin Municipal Science and technology project (Grant No. 19JCYBJC27400) and Beijing-Tianjin-Hebei Basic Research Cooperation Project (Grant No. 20JCZXJC00120).
Disclosure
The author reports no conflicts of interest in this work.
References
- Haugen BR, Alexander EK, Bible KC, Gerard M Doherty 4, Susan J Mandel, et al. (2016) 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid: official journal of the American Thyroid Association 26(1): 1-133.
- Gao M, Ge M, Ji Q, Ruochuan Cheng, Hankui Lu, et al. (2016) Chinese expert consensus and guidelines for the diagnosis and treatment of papillary thyroid microcarcinoma. Cancer Biol Med 14(3): 203-211.
- Shi X, Liu R, Basolo F, Riccardo Giannini, Xiaopei Shen, et al. (2016) Differential Clinicopathological Risk and Prognosis of Major Papillary Thyroid Cancer Variants. The Journal of clinical endocrinology and metabolism 101(1): 264-274.
- Kim HJ, Sohn SY, Jang HW, Kim SW, Chung JH, et al. (2013) Multifocality, but not bilaterality, is a predictor of disease recurrence/persistence of papillary thyroid carcinoma. World J Surg 37(2): 376-384.
- Kim KJ, Kim SM, Lee YS, Chung WY, Chang HS, et al. (2015) Prognostic significance of tumor multifocality in papillary thyroid carcinoma and its relationship with primary tumor size: a retrospective study of 2,309 consecutive patients. Annals of surgical oncology 22(1): 125-131.
- Zhang W, Jiao D, Liu B, Sun S (2016) Analysis of Risk Factors Contributing to Recurrence of Papillary Thyroid Carcinoma in Chinese Patients Who Underwent Total Thyroidectomy. Medical science monitor: international medical journal of experimental and clinical research 22: 1274-1279.
- Grogan RH, Kaplan SP, Cao H, Roy E Weiss, Leslie J Degroot, et al. (2013) A study of recurrence and death from papillary thyroid cancer with 27 years of median follow-up. Surgery 154(6): 1436-1446; discussion 1446-1437.
- Leboulleux S, Rubino C, Baudin E, Bernard Caillou, Dana M Hartl, et al. (2005) Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. The Journal of clinical endocrinology and metabolism 90(10): 5723-5729.
- Neuhold N, Schultheis A, Hermann M, Krotla G, Koperek O, et al. (2011) Incidental papillary microcarcinoma of the thyroid--further evidence of a very low malignant potential: a retrospective clinicopathological study with up to 30 years of follow-up. Annals of surgical oncology 18(12): 3430-3436.
- Katoh R, Sasaki J, Kurihara H, Suzuki K, Iida Y, et al. (1992) Multiple thyroid involvement (intraglandular metastasis) in papillary thyroid carcinoma. A clinicopathologic study of 105 consecutive patients. Cancer 70(6): 1585-1590.
- Al Afif A, Williams BA, Rigby MH, Martin J Bullock, S Mark Taylor, et al. (2015) Multifocal Papillary Thyroid Cancer Increases the Risk of Central Lymph Node Metastasis. Thyroid: official journal of the American Thyroid Association 25(9): 1008-1012.
- Bian X, Chen H, Ye X, Tang PJ (2010) Role of level VI lymph nodes metastasis in cervical metastasis of patients with papillary thyroid cancer. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 45(8): 664-668.
- Yang Y, Chen C, Chen Z, Jiachun Jiang, Yizuo Chen, et al. (2014) Prediction of central compartment lymph node metastasis in papillary thyroid microcarcinoma. Clin Endocrinol 81(2): 282-288.
- Kim K, Kim E, Yoon J, Han K, Moon H, et al. (2013) Preoperative prediction of central lymph node metastasis in thyroid papillary microcarcinoma using clinicopathologic and sonographic features. World J Surg 37(2): 385-391.
- Ning CP, Ji QL, Fang SB, Wang HQ, Zhong YM, et al. (2018) Distribution patterns of microcalcifications in suspected thyroid carcinoma: a classification method helpful for diagnosis. European radiology 28(6): 2612-2619.
- Ha EJ, Baek JH, Lee JH (2017) Diffuse Microcalcifications of Only the Thyroid Gland Seen on Ultrasound: Clinical Implication and Diagnostic Approach. Annals of surgical oncology 24(Suppl 3): 641.
- Wang P, Wang Y, Miao C, Xing Yu, Haichao Yan, et al. (2017) Defining a New Tumor Dimension in Staging of Papillary Thyroid Carcinoma. Annals of surgical oncology 24(6): 1551-1556.
- Zhao Q, Ming J, Liu C, Lan Shi, Xia Xu, et al. (2013) Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Annals of surgical oncology 20(3): 746-752.
- Tam AA, Özdemir D, Çuhacı N, Hüsniye Başer, Cevdet Aydın, et al. (2016) Association of multifocality, tumor number, and total tumor diameter with clinicopathological features in papillary thyroid cancer. Endocrine 53(3): 774-783.

 Research Article
Research Article