Introduction
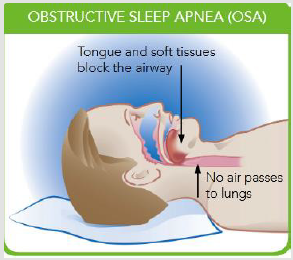
Obstructive sleep apnea, or OSA, is a condition that disrupts breathing during sleep. OSA occurs when the tongue and other soft tissues relax during sleep and obstruct the airway [1] (Figure 1). During sleep, upper airway muscles tend to relax, in healthy subjects, muscle tone is high enough to prevent the upper airway from collapse during sleep but in OSA patients upper airway is not capable to maintain the patency and leads to a partial or complete collapse of the upper airway. The oxygen level in the blood decreases and the brain senses a problem due to sudden reduction (hypopnea) or complete cessation (apnea) of airflow that persists at least for 10 sec. The severity of OSA is measured by apnea/hypopnea index (AHI), which is calculated by apneas and hypopneas per hour of sleep. Sleep studies (Polysomnography) are recommended for the diagnosis of OSA. The AHI score depicts the severity of OSA: Mild (5 ≤ AHI < 15/h), moderate (15 ≤ AHI < 30/h), and severe (AHI ≥ 30/h) sleep [2]. The OSA is more common in males (14%) as compared to females (5%) [3]. Common symptoms of OSA include snoring, daytime sleepiness, irritability, or difficulty with focus or concentration. If left untreated, OSA can lead to secondary health issues such as:
a. Heart attack
b. High blood pressure
c. Stroke
d. Heart failure
e. Irregular heartbeats
f. Weight gain
To reduce the morbidity of OSA, successful treatment of OSA is important. Multiple treatment options are available. Electrical neurostimulation therapy is an emerging treatment option for OSA. In this therapy hypoglossal nerve is stimulated by an electric current that protrudes the tongue and opens the upper airway.
The purpose of this article is to describe the mechanism of electrical neurostimulation therapy for OSA patients.
Current Treatment Options
Current treatment options for OSA range from lifestyle changes to external device-based treatments, such as continuous positive airway pressure (CPAP), to surgery [2] Lifestyle changes such as losing weight, exercising regularly, or consuming less alcohol before sleep may help improve sleep. If lifestyle changes alone do not resolve OSA, CPAP is typically prescribed. CPAP is the most common treatment for OSA. CPAP is an effective treatment that uses a mask to deliver air pressure and keep the airway open. While CPAP is often successful, some people are unable to tolerate this therapy. Oral appliances may be prescribed as an alternative to CPAP. Oral appliances keep the airway open by holding the jaw forward during sleep. Surgical options may be considered by some people who are unable to use or adhere to CPAP or oral appliances. Traditional sleep apnea surgery is intended to make the airway larger by removing or altering facial or airway anatomy. These anatomy altering surgeries can be painful and involve lengthy recovery time.
Electrical Neurostimulation Therapy
Three different systems are available for this nerve stimulation therapy; the working mechanism of each system is different [4]-
1. Hypoglossal Nerve Stimulation (HGNS) system (Apnex Medical, Inc., St. Paul, Minnesota)
2. Aura6000 Targeted Hypoglossal Neurostimulation (THN) system (ImThera Medical, Inc., San Diego, California))
3. Inspire Upper Airway Stimulation (UAS) device (Inspire Medical Systems, Inc., Maple Grove, Minnesota).
Inspire UAS system device is the only system that has approval from Food and Drug Administration (FDA).
Principle of Stimulation Therapy
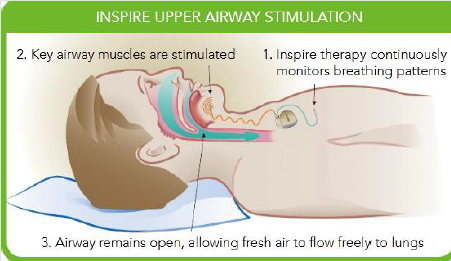
Neurostimulation therapy reduced the activity of dilators muscles of the upper airway during sleep and also stimulates the hypoglossal nerve. Stimulation of the hypoglossal nerve activates the genioglossus muscle which leads to protrusion of the tongue during sleep and prevents the tongue fall back into the pharynx [5].
Patient Selection
Eligibility for the implantation
a. Have been diagnosed with moderate to severe obstructive sleep apnea
b. Have either failed or not tolerated CPAP treatment
c. Have a body-mass index, or BMI, of 32 or less
d. Do not have any other active implantable devices, such as
a pacemaker
e. Do not have certain diseases or conditions that may disqualify them as candidates
Inspire Stimulation Device
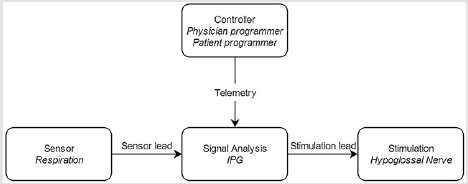
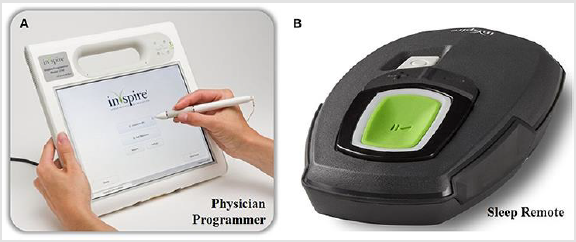
This is a small device that consists of three implantable and two external components, interconnected via either leads or telemetry (Figure 2). Pulse generator, Stimulation, and Sensing leads need to be implanted in the patient’s body (Figure 3). The stimulation electrode was placed on the hypoglossal nerve to recruit tongueprotrusion function and the sensing lead was placed between the internal and external intercostal muscles to detect ventilatory effort [6]. Sensing signals are transferred to a Pulse generator, which filtered and amplified the signals. Physician’s programmers and patient’s programmers are the external components of the Inspire system (Figure 4). These programmers are used to control the pulse generator. A physician’s programmer is a tablet used by a surgeon to control the stimulation and adjustments in the amplitude of signals. The patient’s programmer is used by a patient to switch on and off the device. This system generates the electrical signals, these signals excite the hypoglossal nerve. The depolarization of the nerve produces the action potential in the genioglossus muscle, resulting in protrusion of the tongue [7].
Conclusion
Electrical neurostimulation therapy is an innovative and novel therapy for moderate to severe obstructive sleep apnea. Patient selection can optimize both the efficacy and the workflow of this therapy for selected patients.
References
- Redline S, Kapur VK, Sanders MH, Quan SF, Gottlieb DJ, et al. (2000) Effects of varying approaches for identifying respiratory disturbances on sleep apnea assessment. Am J Respir Crit Care Med 161: 369-74.
- Young T, Peppard P, Gottlieb D (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Resp Crit Care Med 165(9): 1217-39.
- Young T, Evans L, Finn L, M Palta (1997) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 20(9): 705-706.
- Eisele DW, Smith PL, Alam DS, Schwartz AR (1997) Direct hypoglossal nerve stimulation in obstructive sleep apnea. Arch Otolaryngol Head Neck Surg 123(1): 57-61.
- Schwartz AR, Thut DC, Russ B, M Seelagy, X Yuan, et al. (1993) Effect of electrical stimulation of the hypoglossal nerve on airflow mechanics in the isolated upper airway. Am Rev Respir Dis 147(5): 1144-1150.
- Schwartz AR, Eisele DW, Hari A, Testerman R, Erickson D, et al. (1996) Electrical stimulation of the lingual musculature in obstructive sleep apnea. J Appl Physiol 81(2): 643-652.
- Strollo P J Jr, Soose R J, Maurer J T, De Vries N, Cornelius J, et al. (2014) Upper-airway stimulation for obstructive sleep apnea. N Engl J Med 370: 139-149.

 Review Article
Review Article