Abstract
Solitary Reticulohistiocytoma is a rare condition that belongs to a group of diseases associated with the exacerbated immune response of macrophages/monocytes. In this article, we present a rare reticulohistiocytoma case in a Brazilian female patient. The patient had a lesion in the left anterior cervical region with rapid growth. The final diagnosis was made by biopsy, including immunohistochemistry. The definite treatment for the solitary reticulohistiocytoma consists of total resection of the lesion without the need for adjuvant therapies.
Keywords: Non-Langerhans Cell Histiocytosis; Immunohistochemistry; Dermatology; Dermatopathology
Abbreviations:<
RH: Reticulohistiocytosis; SRH: Solitary Reticulohistiocytoma; NLCH: Non-Langerhans Cell Histiocytosis
Introduction
The histiocytosis are a group of diseases associated with the exacerbated immune response of macrophages/monocytes. There is still no consensus regarding their morphological classifications and clinical presentations [1,2]. The most common and studied histiocytosis are Langerhans cell histiocytosis and hemophagocytic lymphohistiocytosis. The others are collectively called Non- Langerhans Cell Histiocytosis (NLCH) or rare histiocytosis [3]. Among the NLCH, Reticulohistiocytosis (RH) can present in a multicentric, diffuse cutaneous, or solitary pattern [4,5]. Solitary Reticulohistiocytoma (SRH) presents as a solitary papule or nodule with a reddish or yellowish hue. It affects mainly the skin and mucous membranes, being first described by Zak in 1950 [5-7]. SHR is a rare condition, and its prevalence has not yet been established [8]. With this in mind, we present below a rare case of SRH in a female patient from southern Brazil.
Case Report
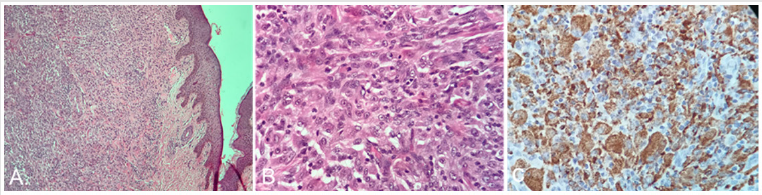
female patient, 34 years old, sought medical assistance due to an asymptomatic lesion in the left anterior cervical region, with rapid growth and spontaneous onset six months ago. The patient reported an attempt to remove the lesion because at first, she believed it was acne. Clinical examination identified a yellowish erythematous, with a brownish center, well circumscribed nodule, measuring 1.2 centimeters, presenting smooth surface, and telangiectasia in the periphery (Figure 1). On ultrasound examination of the cervical region, no lymphadenopathies or any other alterations were identified. Excision of the lesion for anatomopathological analysis was performed. The microscopic findings showed a proliferation of epithelioid cells in the dermis, with nodular architecture, and moderate inflammatory cell infiltration. No Touton giant cells were found (Figures 2A & 2B). The lateral and deep surgical margins were negative. Immunohistochemistry was carried out to define the histogenesis of the lesion. The epithelioid cells were positive for the CD68, in addition to a low proliferative index, assessed by ki67 (Figure 2C). Furthermore, the lesion was negative for CD1A, CD34, and S-100. The morphology and immunohistochemistry, as well as clinical data, were consistent with non-Langerhans cell histiocytosis, favoring reticulohistiocytoma.
Figure 1:Yellowish erythematous well circumscribed skin nodule in the left anterior cervical region.
Figure 2: a) Proliferation of epithelioid cells in the dermis, with nodular architecture (40x. H&E)
b) Detail showing epithelioid and admixed inflammatory cells (400x, H&E)
c) Strong and diffuse immunoreactivity for CD68 is observed in epithelioid cells (immunoperoxidase technique, 400x).
Discussion
Although it can be diagnosed in patients of any age, SRH affects mainly young adults, being more prevalent in males, making the case described above even more curious since the disease affected a female patient. [1,3,5,6,9,10]. SRH is a benign, localized disease induced by cytokines that cause a rare non-neoplastic proliferation of skin histiocytes, originated from the lineage of macrophages that react to yet unknown stimuli [4,5]. Clinically, the SRH presents itself as a single, firm, yellowish or reddish, asymptomatic skin nodule, measuring 0.5 to 2.0 centimeters, but usually smaller than one centimeter [1,10]. Its most common location is in the face, followed by neck and trunk, but can also be found in the mucosa. In our literature review, there are reports of trauma preceding these lesions, which could trigger the local inflammatory response. However, in most cases, a triggering factor for their development is not identified [1,4,5,10].
The diagnosis is based on the patient’s clinical history and the histopathological analysis. The microscopic findings show large histiocytes with eosinophilic cytoplasm in large quantities, with more purplish and amphophilic hues near the center of the histiocyte and lighter eosinophilic staining near the periphery [7]. Immunohistochemistry shows positivity for CD68 and CD163 and, in some cases, also for alpha-1-antitrypsin and lysozyme. The negativity of markers such as CD1a and S100 is essential for the differential diagnosis and exclusion of other histiocytosis [4,11]. Some studies concluded that SRH has clinical, histopathological, and immunohistochemical aspects similar to disseminated xanthogranulomas and multicentric reticulohistiocytosis [12,13]. Since these diseases present worse prognosis than SRH, and may require pharmacological therapy, including chemotherapy, it is essential to exclude these diagnoses. The definitive treatment for SRH consists of total resection of the lesion without the need for adjuvant therapies [1].
Conclusion
Despite the excellent prognosis of SRH, the early diagnosis of the disease is extremely important. Through morphology and immunohistochemistry, as well as clinical information, it is possible to rule out more aggressive histiocytosis which can negatively affect the patient’s quality of life, such as multicentric reticulohistiocytosis and Langerhans cell histiocytosis.
Author Contribution
IRPDP: contributed with study concept, supervised, analyses, research, wrote and reviewed the manuscript; PGLP; analyses, research, wrote and reviewed the manuscript; SSB; research, wrote and reviewed the manuscript; CP: supervised, analyses, reviewed the manuscript; JEJ: supervised, analyses, reviewed the manuscript; MRRCS: supervised, analyses, reviewed the manuscript; EMC: contributed to study concept, coordination, supervision, wrote and reviewed the manuscript.
References
- Classen CF, Minkov M, Lehrnbecher T (2016) The non-Langerhans cell histiocytoses (rare histiocytoses)–Clinical aspects and therapeutic approaches. Klinische Pädiatrie 228(6-7): 294-306.
- Silveira LNA, De Souza Queiroz L, Reis F (2016) Non-Langerhans cell histiocytosis. Acta Neurologica Belgica 116(4): 687-689.
- Nong L, Ren Y, Dong Y, Li D, Li X (2020) Uncommon cutaneous non-Langerhans cell histiocytosis arising from dermal dendritic cells in adults: a clinicopathological study of five cases. European Journal of Dermatology 30(1): 32-40.
- Weissman HM, Hayek BR, Grossniklaus HE (2015) Reticulohistiocytoma of the Orbit. Ophthalmic plastic and reconstructive surgery 31(1): e13.
- Otamendi AV, Ramos Garibay JA, Reyes AM (2012) Reticulohistiocitoma solitario. Revista del Centro Dermatológico Pascua 21(1): 24-26.
- Zak FG (1950) Reticulohistiocytoma ("ganglioneuroma") of the skin. Br J Dermatol 62(9): 351-354.
- Gardner JM (2019) Survival Guide to Dermatopathology. In: Gardner JM (Edt.)., Estados Unidos: Innovative Pathology Press.
- Bonometti A, Berti E, Associazione Italiana Ricerca Istiocitosi ONLUS (2020) Reticulohistiocytoses: a revision of the full spectrum. Journal of the European Academy of Dermatology and Venereology 34(8): 1684-1694.
- Emile JF, Abla O, Fraitag S, Horne A, Haroche J (2016) Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood, The Journal of the American Society of Hematology 127(22): 2672-2681.
- Behera B, Kumari R, Thappa DM, Gochhait D (2020) Dermoscopic features of a case of solitary reticulohistiocytoma. Indian Journal of Dermatology, Venereology and Leprology 86(4): 435-438.
- Miettinen M, Fetsch JF (2006) Reticulohistiocytoma (solitary epithelioid histiocytoma) a clinicopathologic and immunohistochemical study of 44 cases. The American journal of surgical pathology 30(4): 521-528.
- Zelger BWH, Sidoroff A, Orchard G, Cerio R (1996) Non-Langerhans Cell Histiocytoses. Am J Dermatopathol 18: 490-504.
- Snow JL, Muller AS (1995) Malignancy-associated multicentric reticulohistiocytosis: a clinical, histological and immunophenotypic study. Br J Dermatol 133(1): 71-76.

 Case Report
Case Report