Research Article
Prevalence and Associated Anomalies in Gastroschisis
and Omphalocele Cases in Villa Clara, Cuba: A 30-Year
Series from 1990 to 2019
Noel Taboada Lugo1*, Ana E Algora Hernández2, Manuela Herrera Martínez3, María E de la
Torre Santos4, Oriali Piedra Morales5 and Eliecer Anoceto Armiñana6
Author Affiliations
1Master of Sciences, Medical Doctor, Terminal Professional Degree in Clinical Genetics, Associated Professor and Researcher at
the Villa Clara Medical University, Cuba
2Master of Sciences, Medical Doctor, Terminal Professional Degree in Clinical Genetics, Associated Professor of Medical Genetics at the
Villa Clara Medical University, Cuba
3PhD. Master in Sciences. Terminal Professional Degree in Clinical Genetics. Full Professor and Researcher at the Villa Clara Medical
University, Cuba.
4Terminal Professional Degree in Clinical Genetics, Full Professor and Researcher at the Villa Clara Medical University, Cuba
5Medical doctor. Terminal Professional Degree in Radiology, Cuba
6Medical Doctor, Terminal Professional Degree in Pathological Anatomy, Associated Professor of Medical Genetics at the Villa Clara
Medical University, Cuba
Received: June 01, 2021 | Published: June 11, 2021
Corresponding author: Noel Taboada Lugo, Master of Sciences, Medical Doctor, Terminal Professional Degree in Clinical Genetics,
Associated Professor and Researcher at the Villa Clara Medical University, Cuba
DOI: 10.26717/BJSTR.2021.36.005854
Background: Gastroschisis and omphalocele are the most common anterior
abdominal wall defects. The aims of our study were to describe the prevalence trends
of these congenital anterior abdominal wall defects and to determine the frequency and
type of associated congenital anomalies.
Methods: A retrospective, observational study, with data obtained by the Cuban
Registries of Congenital Malformations; was conducted in the Cuban province of Villa
Clara from 1990 to 2019.
Results: A total of 158 cases were identified, 93 of them (59%) with gastroschisis
and 53 with omphalocele. An increasing trend in the prevalence rate per 10,000 births
of the studied abdominal wall defects over the thirty studied years, from 3.83 in 1990
to 7.47 in 2019, was observed. The prevalence rate of gastroschisis (per 10,000 births)
during the study timeframe was twofold those of omphalocele (4.8 and 2.7 respectively).
The majority of gastroschisis cases did not have additional anomalies (80/93 [86%]).
There was a statistically significant difference between the proportions of isolated and
associated cases. (p< 0.01). Omphalocele cases were more likely to be diagnosed with at
least one other congenital defect than those with gastroschisis (25/53 [47%] vs. 12/93
[13%].
Conclusions: Arise in anterior abdominal wall defects prevalence has been noted in
recent decades in Villa Clara province. The present study revealed that omphalocele cases
were more likely to have other congenital defects, predominantly in musculoskeletal and
cardiovascular systems, besides chromosomal aberrations. In our study a very high rate
of termination of pregnancy is observed among abdominal wall defects cases.
Keywords: Abdominal wall defects; Gastroschisis;
Omphalocele; Karyotyping;
Anomalies; Cuba
Anterior abdominal wall defects are a common cause of
morbidity and even mortality. These include the most common
congenital anterior abdominal wall defects (AWD): gastroschisis
(GS) and omphalocele (OM) or exomphalos. GS is a congenital
defect (CD) where the small intestine, part of the large intestine
and occasionally other abdominal organs protrude through a
lateral defect in the ventral abdomen without any protective
membrane, whereas OM is an amnion covered sac enclosing a
range of viscera from a few loops of midgut to the entire midgut,
liver and spleen [1-3]. Such defects were initially described in the
first century AD by the Roman physician Aulus Cornelius Celsus
but until the middle part of the 20th century, no real distinction was
made between the two [3]. The term gastroschisis was first used
by the Italian pathologist Cesare Taruffi in 1894 and translates
from Greek as ‘belly cleft’. The etiology of this CD is unclear, and its
actual pathogenesis is not known. Failure of migration and fusion of
embryonic ventral body folds (particularly from the right) has been
suggested together with disruption of either the umbilical vein or
the vitelline (omphalomesenteric) artery resulting in infarction at
the base of the umbilicus [3,4].
Recent theories challenge this last pathogenic mechanism
and propose that GS results from faulty embryogenesis with
failure of incorporation of the yolk sac and vitelline structures
into the umbilical stalk, resulting in an AWD, through which
the midgut egresses into the amniotic cavity. Thus, GS has no
covering membrane [4]. It is unclear why the failure of fusion of
embryonic folds occurs but is likely to be due to disruption of the
delicate balance of cellular apoptosis and proliferation during this
early stage of development. Although the specific insult is as yet
unknown, observational studies into genetic and environmental
factors supplemented by animal models have allowed developing a
basic framework of associated risk factors [3]. GS is one of the few
major CD with well documented increasing birth prevalence in both
resource-limited and resource-rich settings. The prevalence of GS in
recent decades shows a remarkable and worrying increasing trend
worldwide. Current estimates of the prevalence of GS demonstrate
an uptrend, from 3.6 per 10,000 births during 1995–2005 to 4.9
per 10,000 births during 2006–2012 [1,4-6].
Reasons for the increasing prevalence in GS are unknown;
however, several risk factors are associated with this CD, especially
young maternal age. An increasing prevalence of GS among younger
mothers, especially under 24 years of age, has consistently been
documented, and young maternal age has been recognized as one
of the strongest risk factors for GS [7]. The prevalence of GS also
differs by maternal race/ethnicity, with higher prevalence among
infants born to Caucasian or non-Hispanic white mothers [3,7].
There are less well-defined associations with maternal drug use
(illegal [e.g. cocaine, heroin] and legal [e.g. aspirin]), nutritional
factors, smoking and occupations involving cooking. There may
also be some association with environmental toxins like herbicides
and pesticides, and with the presence of maternal infections,
which include urinary tract infections and/or sexually transmitted
infections [1,3,8].
Evidence of regional or geospatial clustering of GS has also
been described. Among years 2013 and 2018 geospatial primary
and secondary clusters of CD were found by us in the Villa Clara
province. In that study, specifically a secondary spatial cluster of
GS was found in Manicaragua; located at the south-eastern of the
Villa Clara province. It’s a mountainous municipality where 59%
of its population lived in rural areas involved in agricultural land
activities, mainly coffee and tobacco plantations. We surmised that
this geographical cluster could be due to environmental exposures
and further evaluation is necessary to assess this possibility
[9]. Unlike OM, GS has little association with chromosomal
abnormalities. Large series of fetal GS have shown chromosomal
aneuploidy and additional unrelated fetal malformations in1.2%
and 12%, respectively [5]. Most experts agree that the physiological
midgut herniation is present between the 6th and 11th weeks of
gestation and at crown-rump length of less than 45mm. However,
there is 5% physiological midgut herniation could be observed at
12 weeks by three-dimension ultrasound (US) [3,5,10].
The term omphalocele quite literally means swelling (kele) of
the umbilicus (omphalos). The primary defect in OM is most likely
a reduced prominence of the lateral body wall that does not provide
sufficient space for the complete return of the intestines to the body
cavity. After birth, the intestinal loops can be easily seen within an
almost transparent sac consisting of amnion on the outside and
peritoneal membrane on the inside [3,10].
Spontaneous resolution of the first-trimester OM containing
only the bowel was reported. A spontaneous resolution has not
been observed in cases with the herniated liver [5]. The estimated
prevalence of OM ranges from 1.0 to 2.0 per 10,000 live births,
although the true incidence (1 in 3000 to 4000) and morbidity and
mortality may be higher when elective abortions or fetal demises
are taken into account [2,7,11]. In contrast to GS, prevalence studies
of OM have reported either stable rates or modest increases over
time [6,7,12].
In contrast to GS, maternal economic and behavioural
characteristics are not associated with OM. This CD is more
frequently associated with young or advanced maternal age
and with other associated anomalies including pulmonary
hypertension, congenital heart defects, neural tube defects, and
chromosomal abnormalities. When other anomalies are present,
studies have shown a strong association with poor prognosis such
as intrauterine fetal demise and preoperative neonatal death [1-3,13]. The presence or absence of the membranous sac aids in
differentiating GS and OM, however, the membrane can rupture in
the uterus. Ruptured OM has to be distinguished from a large GS.
There are also a few cases of large GS (containing liver) that may
be clinically difficult to differentiate from a ruptured OM [2]. In
these cases, the differential diagnosis is depending on the umbilical
cord insertion site: the umbilical cord insertion site is located in the
umbilical sac in OM and paraumbilical in GS [2,7].
Since 1980, with the continuous improvement of the US
equipment and technology, CD detected in the first and early second
trimesters continued to increase. Routine prenatal screening and
diagnosis of the AWD and any associated CD is paramount and
considered standard of care. Early detection allows for prenatal
genetic counselling and safe delivery at a tertiary care center with
a multidisciplinary team involving neonatologists, obstetricians
and pediatric surgeons [2,5]. Villa Clara province is in the central
region of the Cuban archipelago, with a superficial extension of 8
411, 81 km2, occupying the fourth place among the fifteen Cuban
provinces and representing 7.6% of the country´s total landmass
[14]. With this study we aimed to describe the prevalence trends of
AWD, associated anomalies and chromosomal abnormalities in GS
and OM cases, to provide an insight into the more affected system of
organs and to describe fetal outcomes in both conditions.
This retrospective, observational study was performed from
January 1990 to December 2019 with data obtained by the Cuban
Registry of Congenital Malformations and by the Cuban Prenatal
Congenital Malformations Registry (RECUMAC and RECUPREMAC
respectively, for their names in Spanish), a multicenter, hospital and
community-based registers, which recorded all pre- and postnatally
detected congenital defects.
The RECUMAC and RECUPREMAC are nationwide registries
which cover live births, fetal deaths from 20 weeks’ gestational age
and all terminations of pregnancy for any major CD. Their original
records in the Villa Clara province are stored at the Provincial
Medical Genetics Department (PMGD). We manually scrutinized all
of them for the study time period. Data of the provincial statistical
department, in the Villa Clara provincial health direction was
consulted for population statistics, as the live births number per
years.
We evaluated registered data from all diagnosed cases either
with OM or GS which were coded by trained PMGD staff according
to the 10th revision of the International Statistical Classification
of Diseases and Related Health Problems for Diagnoses (ICD-10),
codes for the aforementioned CD are Q79.2 and Q79.3 respectively,
[15] which are accompanied with a written description for each CD.
The full universe of AWD data was used; no cases were withdrawn
from the study. Due to the Cuban Registries include a textual
description of all the observed CD performed either by US or by
physical examination we avoid the bias of miscoding of the type of
AWD, because GS and OM shared the same code before the version
10 of the International Classification of Diseases -ICD).
Diagnostic Criteria
For GS we included those cases which intestinal extrusion
through a paraumbilical defects without a surrounding membrane
and a normal umbilical cord insertion site; whereas for OM, cases
with a median congenital herniation of viscera into the base of the
umbilical cord after 12 weeks of gestation usually covered by a
membrane, were included. For each case, the following numerical
and categorical variables were obtained and analyzed: year of
diagnosis, specific kind of AWD (GS, OM and others AWD) and the
number and type of associated majors’ CD. In the category “others
AWD” those cases with diagnosis of Pentalogy of Cantrell (defects
of the heart, pericardium, diaphragm, sternum, and AWD), ectopia
cordis thoracis and OEIS complex (Acronym by: OM-Exstrophy
of cloaca-Imperforate anus-Spinal defects), Body Stalk Anomaly
(AWD, severe kypho scoliosis and a short or absent umbilical cord)
or Limb-body wall Complex (AWD or thoraco-abdominoschisis,
limb defects and craniofacial defects) were included [16].
All cases were classified in two classes: “isolated” when no
other majors CD were observed neither by US nor by physical
examination or autopsies and “associated” when another CD was
pre or postnatally diagnosed. The associated majors CD were
counted in each affected system. Associated minors CD were not
included. The associated majors CD were classified in a regional
categorization by system of organs in the following six categories:
Cardiovascular, Respiratory, Central Nervous, Musculoskeletal,
Gastrointestinal and Genitourinary.
Data about associated CD were obtained besides the detailed
US and fetal echocardiogram from post-mortem reports of the
Pathology Department in the Provincial Maternity Hospital
“Mariana Grajales”, where all anatomo-pathological macroscopic
studies were performed.
A separate cytogenetics database confirmed the karyotypes,
and an abnormal karyotype was defined as one known to be
phenotypically significant. Chromosomal studies of the fetal or
neonatal karyotypes, resulting from amniocentesis, chorionic villus
sampling, or postnatal/postmortem studies, were performed in
the Cytogenetic Laboratory of the Medical Genetics provincial
department of the Villa Clara province, Cuba. Karyotyping with
G banding was performed in those cases of AWD with associated
findings on physical examination or diagnosed by prenatal US. The
prevalence rate at birth of AWD was calculated by dividing the
numerator (registered AWD cases of live birth, stillbirth or elective
pregnancy terminations) by the denominator (total number of live births in the studied period). The prevalence rate was expressed as
the number of cases per 10,000 live births.
Fetal outcome was stratified in three main categories:
intrauterine fetal death, elective termination of pregnancy (TOP)
and live births (LB). Data concerning long-term patient clinical
outcomes is not available in the revised CD registers. Categorical
variables were described by frequencies and percentages. We
conduct a statistical hypothesis test on the basis of the results of
the Z test to compare proportions. P value <0.05 was considered
statistically significant. Statistical analysis was done using SPSS
Version 22 software. This study is based on an analysis of existing
registered data, which were anonymously collected, according the
ethical issues on human investigations. Written informed consent
was obtained of all mothers previously at the sample´s obtaining for
chromosomal studies. It was approved by the Ethical Committee of
the Biomedical Research Unit of the Villa Clara Medical University,
following the World Medical Association Declaration of Helsinki
[17,18].
A total of 158 cases of AWD were recorded from 1990 to 2019
in Villa Clara, of these 93 (58.9%) were GS, 53 (33.5%) were OM,
whereas 12/158 (7.6%) were others AWD (which are excluded from
further analysis). The cases were ascertained from 193 916 LB. The
overall prevalence of AWD (per 10,000 LB) was 8.15, meanwhile
the prevalence of GS and OM was 4.80 and 2.73, respectively. That
is, one case of GS in 2085 LB, whereas OM was found in 1: 3658 LB.
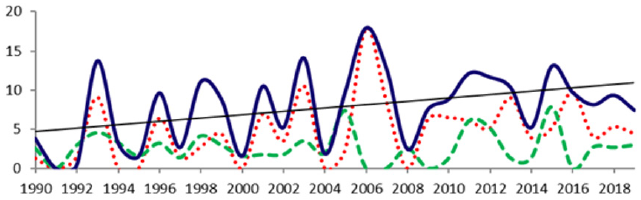
Figure 1 shows an increasing trend in the overall prevalence rate
per 10,000 LB of AWD over the thirty studied years in Villa Clara,
from 3.83 in 1990 to 7.47 in 2019. The GS prevalence was over the
OM prevalence most years during the study timeframe. The peak of
the prevalence of GS was 17.9 per 10,000 LB in 2006.
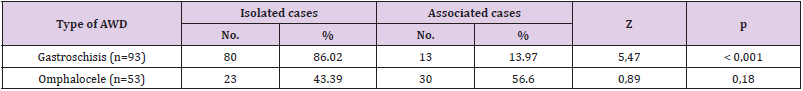
The majority of GS cases did not have additional anomalies
(80/93 [86,0%]). We observed a striking difference between the
proportions of isolated GS and associated cases. (Z= 5, 47; p<
0.001). Meanwhile, (30/53 [56,6%]) of OM cases had associated
CD, although, there were not statistically significant differences
between these proportions (p=0, 18). We identified 65 associated
CD in 43/146 [29,5%]) cases of GS and OM. In 13/93 [14%]) of GS
cases and in 30/53 [56,6%]) of OM cases at least one associated
CD was observed (Table 1). Of the 43 cases with associated CD,
13 (30,2%) had more than one CD. OM cases were more likely to
be diagnosed with at least one other CD than those with GS. This
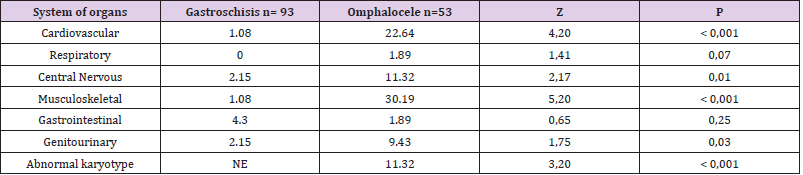
was true for most categories of involved system of organs, which
all shown statistically significant differences, but respiratory and
gastrointestinal. Gastrointestinal CD were the most frequent among
GS cases (4,30%), meanwhile among OM cases musculoskeletal
and cardiovascular CD were the most prevalent with frequencies of
30,19% and 22,64% respectively (Table 2).
One-half of cases with associated CD affecting Central Nervous
System had a Neural tube defects (4/8), where all cases were
identified among OM cases and all the chromosomal abnormalities
were observed among OM cases too (6/53 [11.3%], including three
cases with Trisomy 13, two cases with Trisomy 18 and a single case
with Triploidy as is shown in Table 3.
In Table 3 comparisons among the results from present study
and the literature of cases with GS and OM and the associated CD
was shown.
Regarding fetal outcome, elective TOP took place in 131/146
cases (89.7%), in 4/146 intrauterine fetal death was described
(2.7%), 16/146 were LB (11.0%). Six of these LB cases, (37.5%) had
prenatal diagnosis and parents decided to continue pregnancies.
The prevalence rate of GS (per 10,000 births) during the study
timeframe was twofold those of OM (4.8 and 2.7 respectively).
It is consistent with trends widely described in the literature,
where is stated that prevalence of GS in recent decades shows a
worldwide remarkable and worrying increasing trend, suggesting
a role of environmental factors [1,8,12,19]. From an incidence of
0.06–0.8 per 10,000 in the 1960s, GS has become more prevalent
over the last few decades to its current rates of 4.5–5.13 per 10,000
pregnancies [8]. The prevalence rates (per 10,000 LB) of GS and OM
in our series are consistent with Schemedding [11] who reported
4–5 for GS and 2 for OM, and almost the same as Stalling [7] found
for a larger series in the United States of America (USA) [4.3 for GS
and 2.1 for OM].
The ratio of GS to OM of 1.8:1 seen in our study can be
considered a reflection of the differences in incidence between the
two conditions, as reported in the published literature, which shows
that OM has an incidence rate approximately one-half that of GS and
has been stable over time [13]. Otherwise, the lowest prevalence
rates (per 10,000 LB) of GS worldwide had been described in Asian
countries. In the Liaoning province in China, the prevalence of GS
was 2.30 in a series of ten years of study and 0.50 in Taiwan and
Japan, respectively [20-22]. Authors surmised that to a large extent,
elective abortion may explain the lower incidence of the GS and
AWD in Taiwan [20].
A higher OM prevalence was found over 22 years of data
collection in the Wessex region of England and the Channel Isles,
where 335 cases of OM from 614 321 births were reported from
1994 to 2015, for a prevalence of 5.45 per 10,000 pregnancies [6].
In contrast to OM, GS was rarely associated with a complex pattern
of CD [4]. In the current study, 86% of GS were isolated and the
remaining 14% had associated CD; this is in agreement with other
authors who have reported an incidence of associated anomalies in
GS fluctuating from 5 to over 20% [23-25]. Reported associations
include cardiac abnormalities and increased prevalence of central
nervous system anomalies, and limb and kidney anomalies and may
influence the prognosis of the child with GS significantly [23]. In a
study conducted by Given et al. [26] using data from 18 European
congenital anomaly registries, they identified 1577 GS cases, 83.0%
of which were isolated. The higher frequency of isolated GS cases
than of those with associated CD has been shown in other series
as well [27]. However, in a study conducted in a Mexican hospital,
52/108 (48%) of infants with GS had one or more associated
anomalies, for 1.4 associated defects per case [28].
We found the most frequents associated anomalies in GS cases
affected the gastrointestinal system, mainly intestinal atresia and
necrosis. Intestinal atresia has been reported in up to 25% of GS
cases in some series, and especially when the bowel was thickened
and coated [25]. Likewise, in a study conducted by Lap and
colleagues in the Netherlands they found that the most common
additional gastrointestinal disorder was bowel atresia, accounting
for 94.7% (18/19) of cases with complex GS, whereas the remaining
case had perforation of the proximal jejunum without atresia [23].
Our finding of predominant associated major anomalies involved
the gastrointestinal tract in GS cases is also consistent with a
previously reported series [11] and it´s similar to those found by
researchers from Mexico, Nigeria and by far from USA (shown in
Table 3), nevertheless in France the most frequent associated CD
in GS cases were those affecting Central Nervous System, and in the
series of eleven GS cases from a single hospital in Japan none had
other associated gastrointestinal CD.
Similar to prior reports, we observed that OM cases were more
frequently diagnosed with associated CD compared with those
with GS [27] Musculoskeletal and cardiac anomalies were the most
prevalent associated CD found in OM cases in our study, which is
consistent with the literature, where its claimed that neonates
with OM have higher rates of death compared to neonates with
GS, this difference in mortality is thought to be related to the high
incidence of associated CD and specifically, cardiac abnormalities
among neonates with OM [29]. In our series, 57% of OM cases had
associated CD. These findings are consistent with other reports of
prenatal diagnosis and management of OM where is stated that
about 40–80% of all OM cases would have at least one concurrent
anomaly. Reported associated anomalies include cardiac (7–47%),
gastrointestinal (3–20%), genitourinary (6–20%), chromosomal
(3–20%), musculoskeletal (4–25%) and central nervous system
(4–30%). Authors stated that it is more common to find these
additional anomalies in cases of small defects rather than when a
giant OM [2].
In an study conducted by Corey, et al. [27] evaluating data from
all infants diagnosed with either GS or OM discharged from 348 neonatal intensive care units in North America, managed by the
Pediatrix Medical Group from 1997–2012, they found 162 cases
with an associated congenital heart defect from 507 OM cases, as
it´s shown in the comparison among dissimilar AWD researches
from six different countries. There is a known association between
genetic disease and OM [27]. We found 11% of chromosomal
aberrations among OM cases. This frequency is quite lower than
the reported in a single-center study of AWD prenatally diagnosed,
where chromosomal abnormalities were found by karyotype in 8/29
(28%) fetuses with OM [30]. In our study all cases with abnormal
Karyotypes had numerical chromosomal aberrations (five cases
with autosomal aneuploidy and a single case of polyploidy) and
interestingly we don’t find any case with structural chromosomal
aberrations. It could be caused by the fact that in our province
karyotyping is not performed to all OM cases, but those with pre
or postnatal diagnosis of multiple associated CD or those cases
diagnosed by US in mothers with advanced maternal age, whom
have highest risk for chromosomal aneuploidies. No chromosomal
study was performed to GS cases.
In contrast to our findings, in a study conducted by Zork and
other Americans researchers, of the OM cases with abnormal
karyotypes trisomy 18 (n=8) was the most common, followed
by single cases of trisomy 13, triploidy, trisomy 2 mosaic, and
a structural chromosomal aberration: 46,XX,del(5)(q13q22)
mosaic [31]. Chromosomal aberrations such as trisomy 13 and
18 frequently accompany OM. Certain prenatal US findings can
predict an associated chromosomal aberration, for example, an
intracorporeal liver has a higher association with an abnormal
karyotype than an extracorporeal liver. Furthermore, a small
defect is more likely to be associated with an abnormal karyotype,
by other hand; the presence of multiple CD increases the risk of
chromosomal abnormalities [31,32]. Children with OM have more
than 50% risk of having an associated anomaly, and about 50% of
these have a chromosomal aberration such as trisomy 13, 14, 15,
18 and 21 [33].
Among all abnormal karyotypes in our study we didn’t find any
Down syndrome (trisomy 21) or Turner syndrome (monosomy
X) among the OM cases. However, when twenty-six consecutive
fetuses with a sonographically detectable OM and known karyotype
were reviewed by Nyberg in the Swedish Medical Center, Seattle,
Washington, USA; chromosomal abnormalities were found in 10
cases (38%) from trisomy 18 (n = 4), trisomy 13 (n = 4), trisomy
21 (n = 1), or monosomy X (n = 1) [32]. It is important to note that
even in the setting of a normal karyotype, at least 50% of cases with
OM may have other CD (i.e. musculoskeletal and cardiovascular).
Most cases of GS and OM were prenatally diagnosed in Villa Clara
from 1990 to 2019, and around 90% of parents opted for the
elective TOP, whereas in this timeframe intrauterine fetal death
was described in around 3% of cases. The fetus with GS is at risk
for complications such as intrauterine growth restriction, preterm
delivery, and even intrauterine fetal demise [6]. Meanwhile in OM,
the main prognostic factor in the patient outcome is the presence
and severity of associated CD, although size of defect, prematurity
and sac rupture also have a role to play [3].
In many low and middle-income countries, the reported
mortality of these malformations is 30–100%, while in high-income
countries; mortality in infants with AWD reaches less than 5% [33].
A study conducted in Jamaica showed a frequency of death from GS
of 79%, meanwhile in Uganda, death frequency was 98% of cases
[12,34]. AWD are life-threatening malformations with significant
morbidity, mortality, and prolonged hospitalization, which require
multidisciplinary expertise for their repair and management.
Some parents may choose abortion because of their anxiety when
counseled about the possibility of gastrointestinal discomfort
or other associated CD. A high rate of TOP is associated with the
prenatal diagnosis of AWD, which in turn affects the prevalence at
birth of these CD [20]. Most cases of OM result in high rates of TOP
and/or fetal loss. Because of the OM association with chromosomal
aberrations and other severe CD potentially leading to TOP, over
85% of those with a chromosomal aberration were terminated
in a study of birth prevalence and survival in England and Wales
[33,35].
The surgical outcomes of the isolated AWD without associated
chromosomal or structural abnormalities appear to be good;
however, a very high rate of TOP is associated with AWD, which may
affect the parents’ evaluation of the prognosis of the AWD [20]. In
the Cuban population there is a marked tendency to choose TOP as a
reproductive preventive choice facing the unequivocal identification
of fetal life-threatening CD, conditioned by its reliance in the health
system because of abortions are performed of a secure, free and
institutional way. Likewise, in the Netherlands in up to 74% of
cases of OM, depending on the presence of associated anomalies
and gestational age at diagnosis, the pregnancy is terminated
[36]. Lakasing in a large study of 445 prenatally diagnosed OM
in a single unit over a 10-year period found that less than 10%
reached operative repair due to the recognized high TOP and fetal
death rate [37]. Although there is a high-TOP rate for fetuses with
AWD, the surgical outcome for isolated AWD without structural or
chromosomal abnormalities is good and overall survival rates is
greater than 80% [20,38].
To the best of our knowledge this is the first study conducted in
Cuba including a large series of years to determine the frequency
and type of associated congenital anomalies in GS and OM cases.
The major strength of the current study was the high quality of
Cuban´s hospital and community-based CD registries with reliable
prenatal and postnatal information and absence of unregistered
cases. Besides, Cuban Registries include a textual description of all the observed CD performed either by US or by physical examination
then, the bias of miscoding the type of AWD by using ICD-9 or
ICD-10 codes is inexistent. There are three limitations to our
study: The first is the lack of data regarding number of stillbirths
during the study timeframe, for that reason when prevalence rate
was estimated, in the denominator only LB were included; the
second limitation is that chromosomal studies was not performed
to the totality of the AWD cases, and the thirst limitation is the
non-availability of data concerning to long-term patient clinical
outcomes in the CD registers.
In conclusion, a rise in AWD prevalence has been noted in recent
decades in Villa Clara province. The present study revealed that
majority of GS cases did not have additional anomalies; meanwhile
OM cases were more likely to have other CD, predominantly in
musculoskeletal and cardiovascular systems, besides chromosomal
aberrations. In our study a very high rate of TOP is observed among
AWD cases.
The authors thank Gisela Noche González MD from the
Villa Clara PMGD for her assistant in obtaining RECUMAC and
RECUPREMAC data. We also thank the genetics counselors of Villa
Clara province´s 13 municipalities, who assess all newborns at one
month and three months of age in primary healthcare centers and
contribute to the countrywide congenital abnormality resgistry.
Authors are grateful too for the valuable comments and statistical
assistance provided by Roberto Lardoeyt Ferrer PhD from the
Havana Medical University, Cuba.
- Feldkamp ML, Arnold KE, Krikov S, Reefhuis J, Almli LM, et al. (2018) Risk of gastroschisis with maternal genitourinary infections: the US National birth defects prevention study 1997-2011. BMJ Open 9: e026297.
- Verla MA, Style CC, Olutoye OO (2019) Prenatal diagnosis and management of omphalocele. Sem Ped Surgery 28(2): 84-88.
- Kelay A, Durkin N, Davenport M (2016) Congenital anterior abdominal defects. Paediat Surgery 34 (12): 621-627.
- Stoll C, Alembik Y, Dott B, Roth MP (2008) Omphalocele and gastroschisis associated malformations. Am J Med Genet Part A 146A(10): 1280-1285.
- Ding WP, Li N, Chen M (2020) Ultrasound screening of fetal anomalies at 11–13+6weeks. Mat Fetal Med 3(1): 175-180.
- Safrida EN, Anggraini A, Wibowo T, Wandita S, Haksari EL (2020) Discharge outcomes of liveborn infants with omphalocele (Isolated Vs non-isolated). Mal J Med Health Sci 16(SUPP3): 37-42.
- Stalling EB, Isenburg JL, Short TD, Heinke D, Kirby RS, et al. (2019) Population-based birth defects data in the United States, 2012–2016: A focus on abdominal wall defects. Birth Defects Res 111(2): 1436-1447.
- Melov SJ, Tsang I, Cohen R, Badawi N, Walker K, et al. (2018) Complexity of gastroschisis predicts outcome: epidemiology and experience in an Australian tertiary centre. Pregnancy and Childbirth 18(1): 222.
- Taboada LN, Herrera MM, Hernández GG, Ledesma HH (2020) Geospatial and temporal clustering of folic acid- sensitive congenital defects in Villa Clara Province, Cuba. Biomed J Sci & Tech Res 29(5): 22818-22826.
- O’ Rahilly R (1978) The timing and sequence of events in the development of the human digestive system and associated structures during the embryonic period proper. Anat Embryol 153: 123-136.
- Schmedding A, Wittekind B, Salzmann-Manrique E, Schloesser R, Rolle U (2020) Decentralized surgery of abdominal wall defects in Germany. Pediat Surg Internat 36: 569-578.
- Marshall NSG, Fearon KM, Gill MI, DeSouza CJ, FearonIC, et al. (2017) Mortality-related factors in gastroschisis – a Jamaican perspective. J Ped Surgery 52(4): 530-533.
- Hibbs SD, Bennett A, Castro Y, Rankin KM, Collins JW (2016) Abdominal wall defects among Mexican American infants: The effect of maternal nativity. Ethn Dis 26(2): 165-170.
- (2020) Villa Clara Statistical Year Book. National Office of Statistic and Information. ONEI.
- (2018) Panamericam Health Organization International Statistical Classification of Diseases and Related Health Problems.10th revision. Washington, D.C: OPS.
- Lyons JK (2006) Chromosomal abnormality syndromes. En: Smith´s Recognizable patterns of human malformations. 6th (edn.). Philadelphia: Elsevier Saunders.
- Taboada Lugo N (2017) El consentimiento informado en la práctica asistencial e investigativa de la Genética Clí Acta Med Centro 11(3): 88-100.
- (2017) Helsinki´s Declaration. World Medical Association.
- Wissanji H, Puligandla PS (2018) Risk stratification and outcome determinants in gastroschisis. Sem Ped Surgery 27: 300-303.
- Chen MC, Chen JH, Chen Y, Tsai YH, Lee CH (2019) Low and decreased prevalence of congenital abdominal wall defect in Taiwan. J Pediat Surg 54(9): 1958-1964.
- Li N, Chen YL, Li J, Li LL, Jiang CZ, et al. (2016) Decreasing prevalence and time trend of gastroschisis in 14 cities of Liaoning Province: 2006–2015. Scient Reports 6(1): 33333.
- Suita S, Okamatsu T, Yamamoto T, N Handa, Yuji N, et al. (2000) Changing profile of abdominal wall defects in Japan: results of a national survey. J PediatrSurg 35(1): 66-71.
- Lap CC, Brizot ML, Pistorius LR, Kramer WL, Teeuwen IB, et al. (2016) Outcome of isolated gastroschisis; an international study, systematic review and meta-analysis. Early Human Develop 103: 209-218.
- Tadepally K, Gattu V, Vellanki S (2018) Gastroschisis and spine abnormality in fetus. Med J DY PatilVidyapeeth 11(1): 75-77.
- Beaudoin S (2018) Insights into the etiology and embryology of gastroschisis. Sem Ped Surgery 27: 283-288.
- Given JE, Loane M, Garne E, Nelen V, Barisic I, et al. (2017) Gastroschisis in Europe–A case-malformed-control study of medication and maternal illness during pregnancy as risk factors. Paed Perinatal Epidemiol 31(6): 549-559.
- Corey KM, Hornik CP, Laughon MM, McHutchison K, Clark RH, et al. (2014) Frequency of anomalies and hospital outcomes in infants with gastroschisis and omphalocele. Early Hum Dev 90(8): 421-424.
- Corona RJR, Nieto GR, López ME, Marure E, Cárdenas RJJ, et al. (2016) Associated congenital anomalies in infants with isolated gastroschisis: A single-institutional experience. Am J Med Genet Part 170(2): 316-321.
- Raymond SL, Downard CD, St Peter SD, Baerg J, Qureshi FG, et al. (2019) Outcomes in omphalocele correlate with size of defect. Sem Ped Surgery 54(8): 1546-1550.
- Hidaka N, Murata M, Yumoto Y, Hojo S, Fujita Y, et al. (2009) Characteristics and perinatal course of prenatally diagnosed fetal abdominal wall defects managed in a tertiary center in Japan. J Obstet Gynaecol Res 35(1): 40-47.
- Zork NM, Pierce S, Zollinger T, Kominiarek MA (2014) Predicting fetal karyotype in fetuses with omphalocele: the current role of ultrasound. J Neonatal Perinatal Med 7(1): 65-69.
- Nyberg D, Fitzsimmons J, Mack LA, Hughes M, Pretorius DH, et al. (1989) Chromosomal abnormalities in fetuses with omphalocele. Significance of omphalocele contents. J Ultrasound Med 8(6): 299-308.
- Chukwuemeka ALJ, Ajayi NA, Rolle U (2020) Major abdominal wall defects in the low‑and middle‑income setting: current status and priorities. Pediatr Surg Int 36(5): 579-590.
- Wesonga AS, Fitzgerald TN, Kabuye R, Kirunda S, Langer M, et al. (2016) Gastroschisisin Uganda: opportunities for improved survival. J Pediatr Surg 51(11): 1772-1777.
- Springett A, Draper ES, Rankin J, Catherine R, David T, et al. (2014) Birth prevalence and survival in England and Wales: 2005 to 2011. Birth Defects Res A Clin Mol Teratol 100(9): 721-725.
- Peters NCJ, Hijkoop A, Lechner RL, Eggink AJ, van Rosmalen J, et al. (2019) The validity of the viscera abdominal disproportion ratio for type of surgical closure in all fetuses with an omphalocele. Prenatal Diagnosis 39(10): 1070-1079.
- Lakasing L, Cicero S, Davenport M, S Patel, Kypros HN (2004) Current outcome of antenatally diagnosed exomphalos: an 11-year review. J Pediatr Surg 41(8): 1403-1406.
- Watanabe S, Suzuki T, Hara F, Yasui T, Uga N, et al. (2017) Omphalocele and gastroschisis in newborns: Over 16 years of experience from a single clinic. J Neonatal Surg 6(2): 27.

 Research Article
Research Article