ABSTRACT
The study examines COVID-19 related strokes and the efficiency of endovascular stroke treatment for post COVID patients. The research was performed in the form of retrospective study at the Special Hospital for Cerebrovascular Diseases „St. Sava“ in the Republic of Serbia, from April 2020 to July 2020. The sample included 52 patients with stroke, where the post COVID-19 patients presented 42.3% of the research sample. The aim of the study was to analyse the influence of coronavirus pandemic on stroke cases as well as to indicate COVID-19 related strokes in young adult patients. NIH Stroke Scale/ Score (NIHSS) was used to evidence the efficiency of endovascular treatment.
Keywords: Endovascular treatment (EVT); Mechanical Thrombectomy (MT); Post COVID-19 Patients; Stroke
Introduction
The study examines COVID-19 related strokes and the efficiency of endovascular stroke treatment for post COVID-19 patients. The starting point in this study was the assumption that COVID-19 virus is related to stroke cases in the Republic of Serbia. The study conducted in Madrid has demonstrated that patients with COVID-19 have more severe strokes and poorer outcomes despite similar acute management Fuentes, et al. [1]. Fara, et al. [2] recognised macrothrombosis in the internal carotid artery in patients with mild respiratory symptoms of COVID-19 and stroke as a presenting symptom of the disease (2020). Another assumption in this study was that COVID-19 related strokes have affected young individuals. This assumption is based on literature review Fifi, et al. [3,4] and practical cases in Serbia. Effective reperfusion of the infarct area can be achieved by mechanical thrombectomy (MT), in patients with penumbra the procedure itself starts in a specific time window. That window could be maximum 6 hours for the carotid circulation and 9 hours for the vertebrobasilar circulation, from the onset of stroke. Mechanical thrombus extraction is an interventional procedure to remove a blood clot from a blood vessel. During this procedure, catheters and microcatheters are introduced through the groin - transfemoral approach, which leads to the carotid arteries or its branches across the abdominal aorta, and then to the thrombus that closed the blood vessel.
Recent concept involves the use of intracranial stents: Solitair Platinum, Solitair X, Embotrap and Catch. The stent is positioned above the thrombus in the M1, M2 segment of the ACM or A1 segment of the ACA, and recanalization is achieved by grafting the thrombus with a stent and removing the thrombus from the blood vessel, repeating the procedure until satisfactory Ćulafić, et al. [5]. During MT Heparin is used only for rinsing the guide catheter. Candidates for MT include patients on anticoagulant therapy, postoperative patients, patients with intrahospital infarction, thrombosis M1 and M2 segment ACM, large vessel occlusion (LVO), as well as patients who have not responded to intravenous thrombolytic therapy. Potential benefits of intravenous thrombolysis before MT are partial or complete lysis of the thrombus, which is target of MT, lysis of the embolus in the distal blood vessels to which MT cannot reach, as well as rapid resolution of cerebral ischemia. Potential disadvantages of MT are: starting later, risk of cerebral haemorrhage, as well as partial lysis of the thrombus in a larger blood vessel and the consequent movement of the thrombus more distally out of rich MT Saver, et al. [6].
Materials and Methods
The research was performed in the form of retrospective study at the Special Hospital for Cerebrovascular Diseases „St. Sava“ in the Republic of Serbia, from April 2020 to July 2020. The sample included 52 patients with stroke, where the post COVID-19 patients presented 42.3% of the research sample. The aim of the study was to analyse the influence of coronavirus pandemic on stroke cases as well as to indicate COVID-19 related strokes in young adult patients. During the statistical data processing, the following techniques and methods were implemented: the descriptive statistical measures (frequencies and percentage, arithmetical midranges), the measures of variability, the correlation method.
Results/Observations
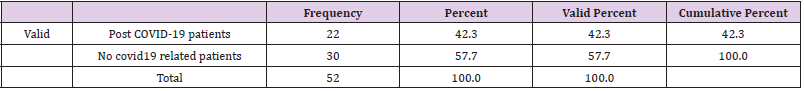
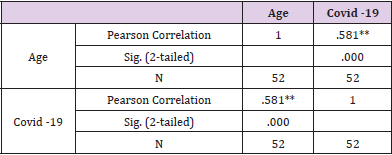
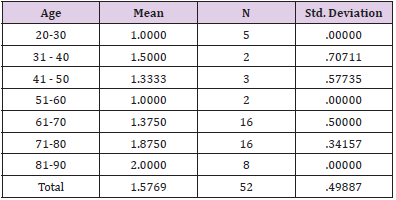
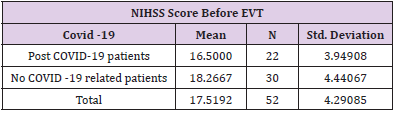
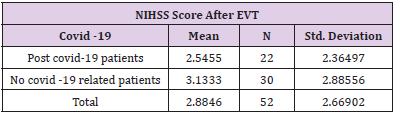
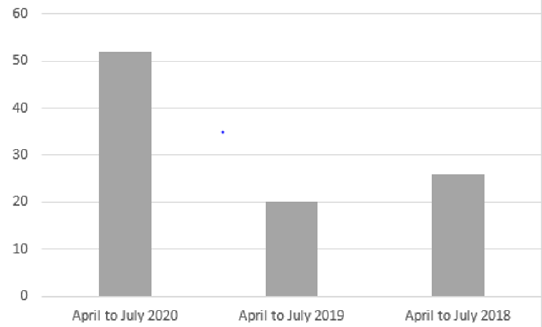
The sample included 52 patients with stroke, who participated in the retrospective study at the Special Hospital for Cerebrovascular Diseases, St. Sava “. To analyse the influence of COVID-19 pandemic on stroke cases, we have compared the number of stroke cases from 2018 to 2020. (Figure 1). presents an increase in the number of stroke patients during the COVID-19 pandemic and first lockdowns in the Republic of Serbia, in comparison to previous years (April to July 2018 and 2019) (Figure 1). Post COVID-19 patients presented 42.3 percent (22 patients) (Table 1), while other 30 patients amounted 57.7 percent in the research sample. If we compare this figure with the number of stroke cases in 2018 (26 patients) and 2019 (20 patients), it can be concluded that the emergence of coronavirus pandemic has affected the statistics of stroke cases (Table 1). Starting from the assumption that COVID -19 related strokes have affected young individuals, we have calculated the correlation between the variables “COVID -19 virus” and “patient’s age”. The results provided in (Table 2). present Pearson Correlation (r=0.58) demonstrating the existence of correlation between the tested variables. (Table 2) In addition, the function of compared Means (covid-19 and age) was calculated to analyse the relations between post COVID -19 patient’s age and stroke cases. Findings in (Table 3). show that all stroke cases in the youngest adult patients (age group: 20-30) are related to post covid-19 patients (N=5, M=1, SD = 0), while the majority of oldest patients (age groups: 71-80 and 81-90 years) is not related to post COVID-19 (N=16, M=1.87 and N=8, M=2). (Table 3) NIH Stroke Scale/Score (NIHSS) was used to evidence the efficiency of endovascular treatment. The average value of NIHSS before EVT (Table 4) in post COVID -19 patients was 16.5 (N=22, M=16.5), in comparison to no COVID related patients (N=30, M=18.3). After the procedure of EVT, the values of NIHSS decreased in all patient groups (Table 5). In post covid-19 patients the average NIHSS amounted 2.54 (M=2.54, N=22), showing the high efficiency of EVT in stroke cases from the sample.
Table 2: Correlation between the variables “COVID -19 virus” and “patient’s age”.
Note: *Correlation is significant at the 0.01 level (2-tailed).
Table 3: Compared Means for variables: age and COVID-19.
Note: Covid -19 (1= post COVID -19 patients, 2= no COVID -19 related patients)
Figure 1: The number of stroke cases at Special Hospital for Cerebrovascular Diseases, St. Sava from 2018 to 2020.
Discussion
The relative proportion of ischemic strokes in our study significantly increased in comparison to previous years, before the COVID -19 pandemic. If we compare the figure of 52 stroke cases in 2020 with 26 cases in 2018 and 20 cases in 2019, it can be concluded that the coronavirus pandemic has affected the statistics of stroke cases. Post COVID-19 patients presented 42.3 percent (22 patients), while no covid related patients amounted 57.7 percent in the research sample. The study conducted by Belani, et al. [7] identified 19 out of 41 patients (46.3%) with acute ischemic stroke who were confirmed to have COVID-19 infection. Mao, et al. [8] indicated that early reports from China described cerebrovascular disease in about 5% of patients with severe COVID-19 disease, with strokes occurring almost two weeks after initial diagnosis. Another important research question referred to the COVID-19 related strokes in young individuals. The calculated correlation between “COVID -19 virus” and “patient’s age” demonstrated the existence of correlation between the variables (r=0.58). According to Pisano, et al. [9] the most common causes in young patients are nonatherosclerotic, more often secondary to cardioembolism or arterial dissection, with risk factors including oral contraceptives, smoking, migraine, drug use, infections, vasculitis, connective tissue, disease congenital and acquired thrombophilia, malignancy, pregnancy, amongst others. Findings presented in this study showed that all stroke cases in the youngest adult patients (age group: 20-30) are related to post covid-19 patients (N=5, M=1, SD = 0), while the majority of oldest patients (age groups: 71-80 and 81-90 years) is not related to post COVID-19 (N=16, M=1.87 and N=8, M=2).
All patients in our study were undergone mechanical thrombectomy. The average value of NIHSS before EVT in post COVID -19 patients was 16.5 (N=22, M=16.5), demonstrating high level of neurological deficit. After the procedure of EVT, the values of NIHSS decreased in post covid-19 patients on the average level of 2.54 (M=2.54, N=22), showing the highly efficient. The combination of MT and thrombolytic therapy, compared with thrombolytic alone, increased the success rate of reperfusion to 70-80%, as well as the positive outcome in general to 40-50% in studies involving all ischemic stroke. When interpreting the findings of this research, certain limitations should be taken into consideration. First limitation is related to the fact that only 52 patients were studied. Further research should include more patients, from different cities in Serbia, or even other countries. Another limitation is the time frame of the research, bearing in mind that the study was carried out from April to July in 2020, during the strictest anti COVID measures and lockdowns in the Republic of Serbia and at the very beginning of coronavirus pandemic.
Conclusion
The study indicated that the cases of ischemic cerebral infarction from the sample were related to post COVID-19 infection. The research also demonstrated an increase in the number of stroke cases during the pandemic in comparison to previous years (April to July 2018 and 2019). Furthermore, the findings provided insight into the variables age and COVID-19 infection, showing that all stroke cases in the youngest adult patients are related to post covid-19 patients. In post covid-19 patients the average NIHSS amounted 2.54 (M=2.54, N=22), showing the high efficiency of EVT in stroke cases from the sample.
References
- Fuentes B, Alonso de Leciñana M, García Madrona S, Fernando Díaz-Otero, Clara Aguirre, et al. (2021) Stroke Acute Management and Outcomes During the COVID-19 Outbreak-A Cohort Study from the Madrid Stroke Network. Stroke 52(2): 552-562.
- Fara M G, Stein LK, Skliut M, Morgello S, Fifi JT, et al. (2020) Macrothrombosis and stroke in patients with mild COVID-19 infection. J Thromb Haemost 18(8).
- Fifi JT, Mocco J (2020) COVID-19 related stroke in young individuals. The Lancet 19(9): 713-715.
- Sweid A, Hammoud B, Bekelis K, Missios S, Tjoumakaris S I, et al. (2020) Cerebral ischemic and hemorrhagic complications of coronavirus disease 2019. International Journal of Stroke 15(7): 733-742.
- Ćulafić S (2019) Protokol za interventne neuroradiološke procedure-The protocol for interventional neuroradiological procedures. Belgrade: Aja grafika.
- Saver J L, Adeoye O (2021) Intravenous Thrombolysis Before Endovascular Thrombectomy for Acute Ischemic Stroke. JAMA 325(3): 229-231.
- Belani P, Schefflein J, Kihira S, Rigney B, Delman B N, et al. (2020) COVID-19 Is an Independent Risk Factor for Acute Ischemic Stroke. American Journal of Neuroradiology 41(8): 1361-1364.
- Mao L, Jin H, Wang M, Hu Y, Chen S, et al. (2020) Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol 77(6): 683-690.
- Pisano TJ, Hakkinen I, Rybinnik I (2020) Large Vessel Occlusion Secondary to COVID-19 Hypercoagulability in a Young Patient: A Case Report and Literature Review. J Stroke Cerebrovasc Dis 29(12): 105307.

 Research Article
Research Article