ABSTRACT
We describe the first case of a 74 years old caucasic man with an etiological diagnosis of SARS-CoV-2 pneumonia treated with tocilizumab and who has been evaluated with lung ultrasound (LU) and Computed Tomography (CT) which is considered the gold standard before and after the treatment. We discuss the procedures adoperate in our ward in order to: minimize the biological risk due to human interactions; how lung ultrasound findings relate with the CT ones. In our experience LU, in the appropriate setting, reduce the spread of the disease and the clinician’s exposure to the infected patient, providing health care workers a cheap and widespread tool that allows a close monitoring of SARS-CoV-2 pneumonia.
Abbreviations: WHO: World Health Organization; ISS: Istituto Superiore di Sanità; HRCT: High Resolution Computed Tomography; LU: Lung Ultrasound; PPE: Protective Equipment; CT: Computed Tomography
Introduction
On 11/03/2020 the World Health Organization (WHO) declared SARS-CoV-2 a pandemic that began in December 2019 in the Hubei region naming it as Coronavirus Disease 2019 (COVID 19) [1]. The Istituto Superiore di Sanità (ISS) reports the first case of autochthonous infection in Italy on 21/02/2020. On 29 March 2020, 97689 total cases of SARS-CoV-2 infection are reported in Italy, and the diagnosis was provided by the regional reference laboratories using Real time PCR tecnique. We report, to our knowledge, the first case of an old man who began the therapy with tocilizumab and who has been evalueted with lung ultrasound.
Case Report
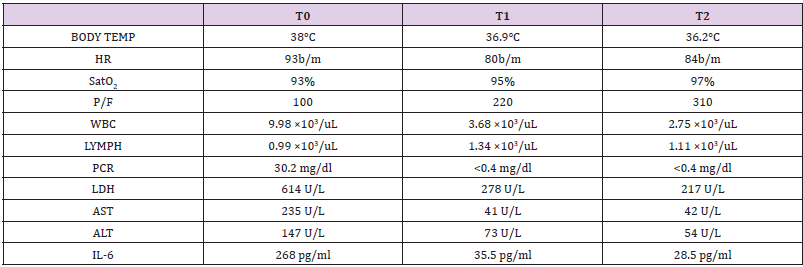
A 74-year-old man referred to the hospital because of fever, cough and dyspnea. He had an history of hypertension and smoking habit. A nasal-pharyngeal swab specimen was obtained to perform Real-time Polymerase Chain Reaction that was positive for the novel coronavirus (SARS-COV-2). He reported no travel towards Northern Italy or China. At admission he had an abnormal body temperature of 38°C, his heart rate was 93 b/m and his on air oxigen saturation was 93% [2] and a PaO2/FiO2 ratio of 100; other significant laboratory datas are reported in (Table 1). The patient began supportive care therapy, lopinavir/ritonavir 200/50mg/ td and idroxicloroquine 200mg/td after cardiological and clinical evaluation. In addition he has been the first patient of our ward treated with a one shot treatment with Tocilizumab 800mg ev (8mg/kg), a recombinant humanized monoclonal antibody directed against the soluble IL-6 receptor (sIL-6r) and the receptor bound to the membrane (mIL-6r) [3]. The patient was discharged after three weeks of hospitalization and with two negative swab specimens during the last 48 hours of his hospital stay.
Table 1: Main clinical and laboratoristic findings during Tocilizumab treatment, T0=admission, T1=10th day, T2 discharge.
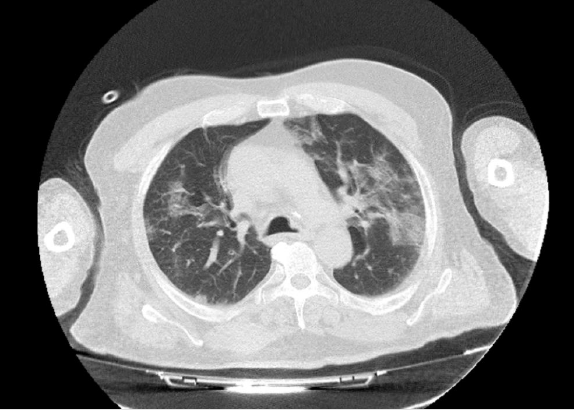
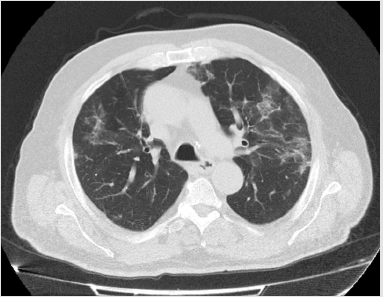
High Resolution Computed Tomography (HRCT) and bed-side lung ultrasound finding had been compared at the beginning and at the end of the therapy. The HRCT showed multiple areas of groundglass type parenchymal hyperattenuation, predominantly subpleural, with typical crazy-paving aspects especially in the posterior lower lobar basal site with associated confluent fibrotic streaks. Thin pleural effusion flap on the left. Moreover, there have been found some parenchimal consolidations especially in the posteriors lobes (Figure 1). Moreover, the CT scan performed immediately before the discharge (Figure 2) showed a reduction of the ground glass and an improvement of the previously detected consolidations [4-5]. In addition the patient performed bed-side Lung Ultrasound (LU).
Lung Ultrasound: How?
Lung ultrasound was performed with a convex probe (3.5 mHz), covered with a latex-free probe cover. The ultrasound machine had also been covered with an internal and external similar latex-free drape. In order to reduce the exposure of the health workers, only one operator, was allowed to enter the isolation room respecting all the preventive measures provided by the World Health Organization for the COVID-19 outbreak [6]. In particular we have been provided a guidance protocol on donning and removing Personal Protective Equipment (PPE) to manage COVID-19 patients and specific procedures for object surfaces’ disinfection. These protocols were shared and agreed by each member of the medical staff, in order to minimize the contamination risk. At the end of the procedure the covered ultrasound machine and probe are sterilized in a dedicated area. Secondly are removed the external drape and the probe-cover. The ultrasound machine remains covered by the internal drape and then is again sterilized. For each examination, we change the external drape and the probe cover. At the end of all scheduled examinations everything is again sterilized and removed [7-8]. The thorax was scanned bedside dividing the chest wall in: superior and inferior anterior wall, superior and inferior lateral wall, superior and inferior posterior wall, both sides [9]. One of the most important difficulty we encoutered was the sight’s reduction during LU due to the personal and machine protective equipment. For this reason LU in a COVID setting might be time consuming. Two experienced clinicians reviewed the images in post processing.
Lung Ultrasound: Findings
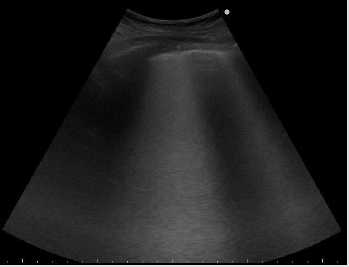
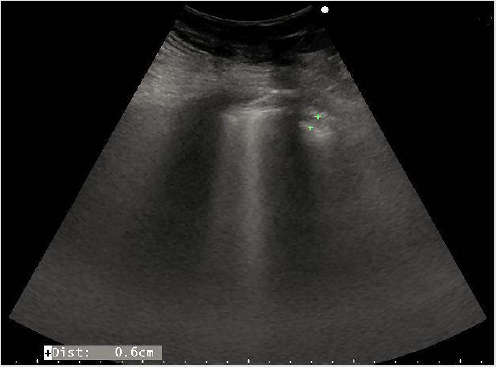
LU at admission assesed the presence of diffusively bilateral irregular and thickened pleural line with sliding reduction’s. Confluent B lines with white lung areas and some sub-pleural consolidations in the postero lateral areas (Figures 3 & 4), especially on the left side [10]. Pleural effusion on the left. The consolidations appeared as small ipo-iso echoic areas. We found a characteristic posterior distribution of the above features.
Figure 4: Shows a sub pleuric ipo-iso echoic consolidation, multiple B lines, pleural thickness and irregularities.
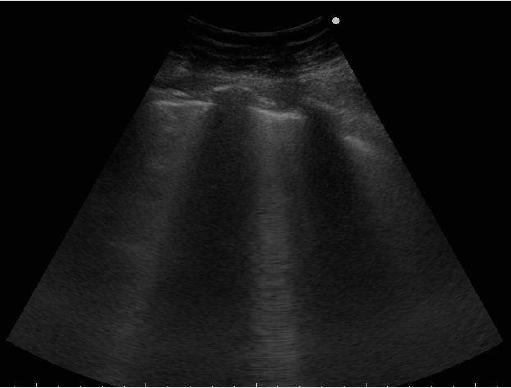
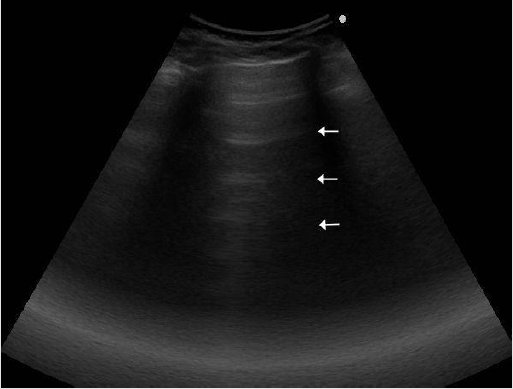
Finally we report the LU performed immediately before the discharge (Figures 5 & 6), showing more ventilated areas characterized by the presence of A lines and the reduction of B lines, that according to the literature, is an ultrasound finding of GGO improvement [11-12].
Discussion
To our knowledge, this is the first lung ultrasound description of COVID-19 pneumonia in an old man with respiratory distress and a confirmed diagnosis of SARS-COV2 infection treated with Tocilizumab. Although a low PaO2/FiO2 ratio, due to his relatively stable hemodynamic and clinical conditions we decided for a wait and see strategy and to begin the therapy with Tocilizumab. Lung ultrasound allowed us to recognize typical features of interstitialalveolar impairment showing bilateral, diffuse pleural line abnormalities, subpleural consolidations, white lung areas and B lines that in this setting with a characteristic posterior distribution, that we considered patognomonic for the disease. Nowadays lung ultrasound is a well estabilished tool able to help the clinician in the evaluation of several respiratory syndromes. However, the use of lung ultrasound in the evaluation of a suspected or confirmed COVID-19 patient implies, even in an infectious disease health care facility used to handle high risk outbreaks, several attentions. This is why we gave great importance to staff’s preparation and organization before the examination, not only with appropriate protocols for donning and removing PPE or drapes from the ultrasound machine, but also establishing “clean” and “dirty” pathways inside the ward and the right sanification procedures. LU can be safely performed bed-side by the same clinician, who is evaluating the patient reducing the number of health workers potentially exposed. This would really transform US in the new stethoscope which, on the other hand, cannot easily be used due to the high risk of self-contamination [13-14].
CT scan require the patient to be moved to the radiology unit and back to the ward and, altough there have been established several protocols to handle this setting in our facility providing different pathways, appropriate sanification and use of PPE, potentially several people can be exposed, from health care professional to the other patients requiring later a CT scan. Finally, as in our case, we found a relation between the clinical improvement (e.g. oxygen need) and the one seen at LU or CT, that were concordant. So, another advantage is that it’s a cheap, radiation-free tool that allows a close monitoring of the patient’s lung impairment during hospitalization or in the outpatient setting [15]. In our opinion LU can also be performed in an outpatient setting, even with portable devices, only if the above protocols, that require a learning curve to be properly applied, can be respected. For this reason, lung ultrasound can be a useful tool for patient management and stratification also able to decide which are the ones who may require, hospitalization, intensive care management or even a safer discharge supporting clinical and laboratoristic datas. In our experience LU is useful to assess the relation between clinical and ultrasound lung pattern evolution also in patients treated with Tocilizumab.
Conclusion
We encourage the use of lung ultrasound as a useful tool to evaluate COVID-19 pneumonia suggesting a safe procedure to perform it bed-side minimizing the risk of contamination. Moreover, due to its capability to show in real time lung involvement during the hospitalization it could be a valuable tool for monitoring this patients and to evaluate whether or not to begin an experimental therapy in complex settings. LU can be useful in an outpatient setting, even with portable devices, only respecting the right protocols in order to avoid the disease’s spread.
Conflict of Interest
The Authors declare that they have no conflict of interests. For case reports our ethic committee simply requires a communication but not an approval.
Acknowledgement
The Authors thank all the colleagues, nurses and workers who are facing the disease competently and ethically with the aim of serving others. A special thanks to our families for supporting us.
References
- Zhu N, Zhang D, Wang W, Li X, Yang B, et al. (2019) China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China. N Engl J Med 382: 727-733.
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, et al. (2019) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020 382(18): 1708-1720.
- (2010) Protocol Title: “Multi-center study on the efficacy and tolerability of tocilizumab in the treatment of patients with covid-19 pneumonia” EudraCT Number.
- Sana Salehi (2020) Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol 14: 1-7.
- Bern heim A, Mei X, Huang M, Yang Y, Fayad ZA, et al. (2010) Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of Infection. Radiology 20: 200463.
- (2020) WHO. Medical devices. Personal protective equipment.
- Procedure generali infection prevention and control in corso di epidemia da COVID-19-P.O. “D. Cotugno”
- Documento intersocietario SIUMB SIRM: Modalità di comportamento per l’effettuazione di un esame ecografico in questo momento pandemico.
- Luna Gargani, Giovanni Volpicelli (2014) How I do it: Lung ultrasound Gargani and Volpicelli Cardiovascular Ultrasound 12: 25
- Carla Maria Irene Quarato (2020) The artificial count of artifacts for thoracic ultrasound: what is the clinical usefulness? J Clin Monit Comput 34(6): 1379-1381.
- Lichtenstein D, Meziere G, Biderman P (1997) The comet-tail artifact. Am J Respir Crit Care Med 156(5): 1640-1646.
- Wang, Luna Gargani, Tatiana Barskova, Dan E (2017) Furst and Marco Matucci Cerinic Usefulness of lung ultrasound B-lines in connective tissue disease-associated interstitial lung disease: a literature review YuKai Arthritis Research & Therapy 19: 206
- Copetti R (2016) Is lung ultrasound the stethoscope of the new millennium? Definitely yes Acta Med Acad 45: 80-81.
- Danilo Buonsenso, Davide Pata, Antonio Chiaretti (2020) COVID-19 outbreak: less stethoscope, more ultrasound. Correspondence Lancet Respir Med 8(5): e27.
- Buonsenso D, Piano A, Raffaelli F, Bonadia N, De Gaetano Donati (2020) Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. European Review for Medical and Pharmacological Sciences 24(5): 2776-2780.

 Case Report
Case Report