ABSTRACT
Introduction: Pubovaginal sling is an efficient and safe procedure for stress urinary incontinence without the complications of synthetic sling. Urine retention and de novo urgency are bothersome aftermath of this procedure. We aim to identify potential risk factor for de novo urgency after autologous pubovaginal sling.
Methods: From 2013 to 2016, 347 patients underwent autologous pubovaginal sling. Age, BMI, pelvic irradiation, use of anticholinergic medication, previous vaginal related surgical histories, “over-tight” technique, concomitant surgeries were examined for potential risk factors. De novo urgency/urge incontinence was defined as treatment (medication, botulinum toxin/botox injection, sacral neuromodulation) for urge postoperatively and was not noted before surgery. Chi-square and fisher’s exact testes were used as statistical analysis.
Results: 109 patients underwent autologous rectus fascia pubovaginal sling, after excluding status post urethral diverticulectomy, concomitant diverticulectomy, and concomitant abdominal surgery. 23(21.1%) patients were treated for de novo urge/ urge incontinence, 18 (78.2%) with anticholinergic, 4 (17.3%) with botox injection and 2 (8.69%) with sacral neuromodulation. None but prior pelvic organ prolapse surgery was associated with developing de novo urge/urge incontinence (p=0.026).
Conclusion: Patients with prior pelvic organ prolapse surgery were more likely to be at risk of de novo urgency after autologous pubovaginal sling. This study provided more information for preoperative consultation for patients undergoing incontinence surgery.
Keywords: Stress Urinary Incontinence; De Novo Urge Urinary Incontinence; De Novo Urgency; Autologous Pubovaginal Sling
Abbreviations: ASC: Abdominal Sacrocolopopexy; AF: PVS Autologous Rectus Fascia Pubovaginal Sling; DO: Detrusor Overactivity; LSC: Laparoscopic Sacrocolpopexy; MUS: Mid-Urethral Sling; POP: Pelvic Organ Prolapse; PSC: Pubovaginal Cystocele Sling; SUI: Stress Urinary Incontinence
Introduction
Stress urinary incontinence (SUI) is reported in 10-40% of women and has a bothersome impact on the quality of life [1]. The surgical treatments consisted of mid-urethral slings (MUS), pubovaginal slings, retropubic slings, transvaginal urethral suspensions and urethral bulking agents. Autologous rectus fascia pubovaginal sling was first introduced in the early 20th century, but for the last two decades, synthetic mid-urethral slings have been the main stay of treating SUI. MUS gained its popularity due to shorter operative time, absence of harvest site complications (pain and infection) [2], faster recovery [3], however urologists and gynecologists have growing concerns for synthetic MUS after several statements made by the Food and Drug Administration since 2008 [4]. Autologous pubovaginal sling has been regaining popularity in the recent years, with reported excellent success rates [5]. This procedure is suitable for patients with concomitant urethral diverticulectomy, concomitant urethrovaginal fistula, and post complications failed previous synthetic sling [6].
Although autologous pubovaginal slings have no concern for mesh-related adverse events, inevitably certain complications have been reported, such as urinary retention, voiding difficulty and de novo urgency incontinence [7,8]. De novo urgency has been reported to be 2-20% [9]. Urgency is a bothersome symptom, especially for patients who are already suffering from stress urinary incontinence. Unanticipated de novo urgency/ urge incontinence after continent surgery may be discouraging on patients’ satisfaction. Much effort was exerted in finding the risk factors of postoperative urgency/ urge incontinence after synthetic mid urethral sling, such as age, preoperative urodynamic finding of detrusor overactivity (DO), and presence of pelvic organ prolapse [10,11]. However limited literature to date investigates of the potential risk factors contributing to de novo urgency/ urge incontinence after autologous pubovaginal sling. In this study, we reviewed patients’ baseline characteristics, related-history and surgical technique who had underwent rectus fascia pubovaginal sling and analyzed in those who received secondary treatments for de novo urgency/ urge incontinence. The aim is to identify the potential risk factors attributed to postoperative de novo urgency/ urge incontinence.
Material and Methods
Between 2011 and 2016, a total of 347 women with SUI underwent pubovaginal sling in a single medical center, this study included only patients using rectus fascia and who followed up postoperative for over a year. The patients with concomitant abdominal surgery, concomitant urethral diverticulectomy and previous diverticulectomy were excluded to eliminate confounding factors in the study population. De novo urgency is defined in patients who did not report urge or urge incontinence, but were treated with anticholinergics or beta3 agonist, intravesical botox injection and sacral neuromodulation. We understand urgency/ urge incontinent treated in a tiered manner; therefore, we recorded the treatment modality seen at the last follow up date. Data were extracted from electronic medical records and charts. Baseline data including age, BMI, prior irradiation, prior hysterectomy, prior surgeries for SUI were recorded. Perioperative details such as “overtight” method, concomitant pelvic organ prolapse (POP) surgery and concomitant urethral surgery were collected. Patients who follow up less than a year, previous or concomitant diverticulectomy, concomitant abdominal surgery were excluded. Descriptive data were presented as mean. The Chi-square and fisher’s exact testes were used to compare categorical variable. The chi-square analysis was done to find a relationship between urgency/urge incontinence and those parameters. A p- value for <0.05 was considered to be statically significant. All analyses were conducted suing the statistical Package for Social Sciences (SPSS) version 24.0.
Result
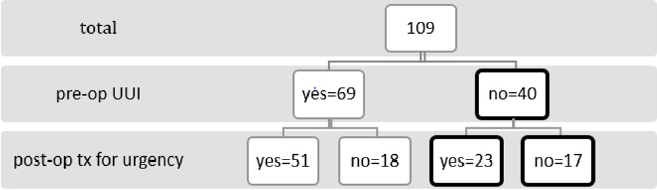
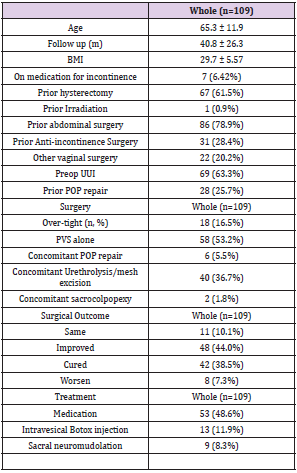
Total of 109 patients were included in this study after the exclusion of patients following up less than a year, prior and concomitant urethral diverticulectomy as shown on Figure 1. The median age was 65.3 ± 11.9 years at the time of surgery, they were followed up for 40.8 ± 26.3 months after surgery. Among these patients, 67 (61.5%) had prior hysterectomy, only 1 (0.9%) had prior irradiation, 86 (78.9%) had prior abdominal surgery, 31 (28.4%) had prior anti-incontinence surgery. The cohort demographic data is as described in (Table 1). In the surgical aspect, 18 (16.5%) patients utilized the “over-tight” technique. 58 (53.2%) patients had underwent pubovaginal sling alone, while 6(5.5%) had concomitant POP repair, 40 (36.7%) had urethralysis or mesh excision, only 2 (1.8%) had concomitant sacrocolpopexy. In the overall population, 11 (10.1%) patients reported similar bothersome SUI postoperatively, 48 (44.0%) patients stated improved symptoms, 42 (38.5%) patients were cured, but 8 (7.3%) patients reported worsen symptoms.
Figure 1: Patient Distribution.
Note: 109 patients were included in our study, 40 patients did not present with urge urinary incontinence preoperatively. Among these 40 patients, 23 patients received treatment or postoperatively urge urinary incontinence and 17 patients were not treated
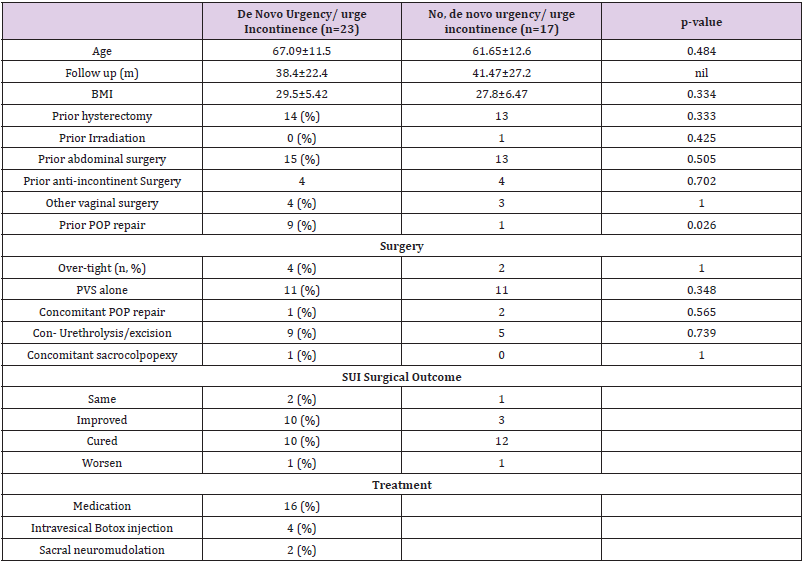
We focus on our analysis on the 40 patients who did not mention nor treat for urge/ urge incontinence preoperatively but developed de novo urge/urge incontinence (n=23), as shown as the highlighted box in Figure 1. Among the 23 patients with de novo urgency/urge incontinence, most of the patients (n=20) reported improved or cured symptoms, while 2 patients stated similar bothersome and 1 patient stated worsen symptoms. In patients with de novo urge/ urge incontinence, 16 patients were treated with anti-cholinergic medication, 4 patients were treated with Botox injection and 2 were treated with sacral neuromodulation. One patient with de novo urgency incontinence were treated with both medication and botox injection. Chi-square analysis was done in attempt to identify the potential risk factor of de novo urgency/urge incontinence after autologous pubovaginal sling as shown in (Table 2). Patients with previous POP repair were more likely to receive secondary treatment for de novo urgency/urge incontinence (p=0.026). Age, BMI, previous abdominal surgery, previous hysterectomy, previous mid urethral sling, previous bulking agent injection, previous other vaginal surgery, concomitant surgeries were not found to have statistical significance in relations to de novo urgency/ urge incontinence.
Table 2: Comparison between patients with de novo urgency/urge incontinence and those did not by Chi-square.
Discussion
Though synthetic mid-urethral sling has been proven to achieve high success rates, the concern for adverse events has made autologous pubovaginal sling regain popularity for the treatment of stress urinary incontinence. The downfalls of pubovaginal slings reported were wound infections, obstructive symptoms and de novo urgency incontinence [12]. This study had identified previous POP repair and over-tight technique to be related to patients seeking for treatment for de novo urgency incontinence after surgery. The etiology of de novo urgency after incontinence surgery has not been validated but causes of de novo urgency after synthetic sling were proposed by Abraham et al, including urinary tract infection, bladder outlet obstruction, perforation of the urinary tract and idiopathic urgency [13]. Similar hypothesis can be implemented in autologous pubovaginal sling, except perforation by foreign body. Other hypotheses included irritation of the vesical neck [14], it is suggested bladder contraction is triggered by urine entering proximal urethra [15], and urethral afferent activity can evoke involuntary detrusor activity [16].
Autologous pubovaginal sling is a bladder neck sling, with increasing pressure on the bladder neck, may result in involuntary detrusor activity and subsequently urgency/urge incontinence as a subjective symptom. This hypothesis makes the finding that pubovaginal sling had more de novo urgency reported than midurethral sling [17]. We defined de novo urgency as subjects seeking medical treatments such as anticholinergic medication, intravesical botox injections and sacral neuromodulation, without urgency symptoms in preoperative charting. Previous studies had used a more objective questionnaire and/or included patients on anticholinergic medication [18,19]. We included patients who were much affected in order to identify possible risk factors attributed to de novo urgency incontinence. Age, BMI, previous SUI surgeries were not related to de novo urgency incontinence. “Over-tight” technique and concomitant surgeries were also not attributed to de novo urgency incontinence.
Previous POP repair surgery dissections are speculated to be more extensive therefore resulting in de novo urgency incontinence. Since extensive dissections may be disrupting the autonomic innervation of the bladder, which is also another possible pathogenesis of de novo urgency [20]. Despite much input in attempt to investigating potential risk factors for de novo urgency, there is limited evidence to support a convincing risk factor. A similar study was done, also trying to look for prognostic factors of autologous fascia rectus sling, and none of the preoperative parameters proved to be associated with the final outcome [21]. Kenton et al was also unable to find an association between any other preoperative symptoms, urodynamic parameters or patient characteristics and postoperative treatment or bother form UUI [18], after they looked into patient’s status post Burch colposuspension and pubovaginal sling. The urodynamic parameters related urgency post-sling procedure have been studied. Alperin et al noticed an elevation of detrusor pressure >15cm H2O during the filling phase of cystometry put patients at risk of developing de novo urgency incontinence [19].
However, urge/ urge incontinence was self-reported, unlike in this study, the patients were included only if they were treated. Mitsui et al. investigated the clinical and urodynamic outcome of autologous pubovaginal, found out patients who had PVR more than 100mL or Qmax 20mL/s or less were more likely to have voiding problems. No urodynamic parameters were reported to associate with urgency/urge incontinence but noted postoperative urgency and de novo urgency rate as 38% and 8% respectively [20]. Heterogeneous findings in identifying risk factors for de novo urge/ urge incontinence were present in our literature review. Not all literatures found urodynamic parameters to be risk factors [18,21]. The presence of detrusor overactivity, history of prior anti-incontinence surgery was reported to be risk factors of de novo urgency/ urge incontinence, while poorer anterior and apical vaginal support were “protective” factors after mid urethral sling [10].
Another study found preoperative urge, detrusor overactivity and prior use of anticholinergic mediation were more likely to develop de novo urgency/urge incontinence after autologous sling and/or Burch procedure [18]. However prior medication did not show significance in our result. The limitations of this study were a retrospective and single center study. Our study number would have more statistical power if we have a larger cohort, however de novo urgency is not a common sequela but a very bothersome symptom after pubovaginal surgery. This study was a snapshot in time, treatment modality was recorded as their last clinic visit. There was no follow up on the change of treatment over the course of time, given that urge/urge incontinence treatment is tiered. Therefore, a follow up outcome of those treated is a future aspect of research. There was no literature available on studying the possible risk factors to de novo urgency/ urge incontinence after autologous pubovaginal sling. We a relatively long follow-up period of time.
Conclusion
De novo urgency/ urge incontinence may be troublesome and affects the daily life of patients, therefore it is important in informing and discussing with the patients of such condition. Our study found prior pelvic organ prolapse surgeries as possible risk factors related to postoperative de novo urgency, hoping to give more information in consultation for autologous pubovaginal sling.
Acknowledgement
Not applicable.
Conflicting Interests
The authors declare that they have no conflicting interests.
References
- Hunskaar S, Burgio K, Diokno A, Herzog AR, Marie Carmela Lapitan, et al. (2003) Epidemiology and natural history of urinary incontinence in women. Urology 62(4 Suppl 1): 16-23.
- Cox A, Herschorn S, Lee L (2013) Surgical management of female SUI: is there a gold standard? Nat Rev Urol 10(2): 78-89.
- Kaplan SA, Santarosa RP, Te AE (1996) Comparison of fascial and vaginal wall slings in the management of intrinsic sphincter deficiency. Urology 47(6): 885-889.
- Bailly GG, Carlson KV (2017) The pubovaginal sling: Reintroducing an old friend. Cuaj-Canadian Urological Association Journal 11(6): S147-S51.
- Milose JC, Sharp KM, He C, Stoffel J, Clemens JQ, et al. (2015) Success of autologous pubovaginal sling after failed synthetic mid urethral sling. J Urol 193(3): 916-920.
- Ghoniem G, Hammett J (2015) Female pelvic medicine and reconstructive surgery practice patterns: IUGA member survey. Int Urogynecol J 26(10): 1489-1494.
- Chaikin DC, Rosenthal J, Blaivas JG (1998) Pubovaginal fascial sling for all types of stress urinary incontinence: long-term analysis. J Urol 160(4): 1312-1316.
- Cross CA, Cespedes RD, McGuire EJ (1998) Our experience with pubovaginal slings in patients with stress urinary incontinence. The Journal of urology 159(4): 1195-1198.
- Niknejad K, Plzak LS, Staskin DR, Loughlin KR (2002) Autologous and synthetic urethral slings for female incontinence. Urol Clin North Am 29(3): 597-611.
- Lee JK, Dwyer PL, Rosamilia A, Lim YN, Polyakov A, et al. (2013) Which women develop urgency or urgency urinary incontinence following midurethral slings? Int Urogynecol J 24(1): 47-54.
- Lee JK, Dwyer PL, Rosamilia A, Lim YN, Polyakov A, et al. (2011) Persistence of urgency and urge urinary incontinence in women with mixed urinary symptoms after midurethral slings: a multivariate analysis. BJOG 118(7): 798-805.
- Sharifiaghdas F, Nasiri M, Mirzaei M, Narouie B (2015) Mini Sling (Ophira) versus Pubovaginal Sling for Treatment of Stress Urinary Incontinence: A Medium-term Follow-up. Prague Med Rep 116(3): 210-218.
- Abraham N, Vasavada S (2014) Urgency after a sling: review of the management. Curr Urol Rep 15(4): 400.
- Summitt RL, Bent AE, Ostergard DR, Harris TA (1990) Stress incontinence and low urethral closure pressure. Correlation of preoperative urethral hypermobility with successful suburethral sling procedures. J Reprod Med 35(9): 877-880.
- Fulford SC, Flynn R, Barrington J, Appanna T (1999) An assessment of the surgical outcome and urodynamic effects of the pubovaginal sling for stress incontinence and the associated urge syndrome. J Urol 162(1):135-137.
- Jung SY, Fraser MO, Ozawa H, Yokoyama O, Yoshiyama M, et al. (1999) Urethral afferent nerve activity affects the micturition reflex; implication for the relationship between stress incontinence and detrusor instability. J Urol 162(1): 204-212.
- Ogah J, Cody JD, Rogerson L (2009) Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 7(4): CD006375.
- Kenton K, Richter H, Litman H, Lukacz E, Leng W, et al. (2009) Risk factors associated with urge incontinence after continence surgery. J Urol 182(6): 2805-2809.
- Alperin M, Abrahams Gessel S, Wakamatsu MM (2008) Development of de novo urge incontinence in women post sling: the role of preoperative urodynamics in assessing the risk. Neurourol Urodyn 27(5): 407-411.
- Mitsui T, Tanaka H, Moriya K, Kakizaki H, Nonomura K (2007) Clinical and urodynamic outcomes of pubovaginal sling procedure with autologous rectus fascia for stress urinary incontinence. Int J Urol 14(12): 1076-1079.
- Athanasopoulos A, Gyftopoulos K, McGuire EJ (2011) Efficacy and preoperative prognostic factors of autologous fascia rectus sling for treatment of female stress urinary incontinence. Urology 78(5): 1034-1038.

 Research Article
Research Article