Abstract
In 1993, Zukerberg et al. described an aggressive vascular neoplasm, named Kaposiform Hemangioendothelioma (KHE) [1]. It originates on the skin, and usually affects deeper tissues by infiltrative growth. However, KHE can present anywhere, including the retroperitoneum, the mediastinum, the pelvis, visceral organs, or the mesentery [2-5]. Frequently, KHE is associated with Kasabach–Merritt phenomenon (KMP), a condition hallmarked by platelet trapping leading to profound thrombocytopenia, hypofibrinogenemia, and elevated coagulation activation. It is distinguished from disseminated intravascular coagulation in pathophysiology noted for worsening coagulopathy triggered by platelet entrapment. About 50-60% of patients with KHE have KMP, with mortality rates up to 30% [2,6]. Schmid et al. confirmed that infants and toddlers have a higher risk of developing a KMP as compared to older children [7]. It typically presents as an induration, plaque-like cutaneous lesion, bulky (> 5 cm), solitary, painful, ill-defined margins, and pebbly texture with violaceous color and involves multiple planes of tissue [4,6,8,9]. According to the World Health Organization histopathological classification (2013), Angiosarcomas (AS) and Epithelioid Hemangioendotheliomas (EHE) are malignant vascular tumors, whereas Kaposiform Hemangioendothelioma (KHE) is classified as a rarely metastasizing vascular neoplasm of intermediate malignancy [10].
The disease is usually diagnosed by clinical exam and Magnetic Resonance Image (MRI). Confirmatory biopsy might be performed in selected cases [6]. The MRI findings in KHE are ill-defined margins, multiplanar involvement, diffuse enhancement, is intensity relative to muscle on T1-weighted imaging, hyperintensity on T2- weighted imaging and destruction/remodeling of adjacent bone [8]. Although Sauer et al. demonstrated that total resection was not a favorable prognostic factor [10], the surgical excision is the gold standard if it can be done in healthy margins and with no deterioration but is rarely possible due to the infiltrative feature of the tumor [9,11]. The treatment involves tailored therapy depending on the lesion and surgical resection when feasible. Oral steroids, weekly vincristine (VCR) and sirolimus for patients with unresectable lesions and KMP are the most common treatment options described in medical literature [6]. Wang et al. demonstrated that VCR was efficacious in almost 80% of steroid resistant KHE patients [12]. Here we report a successful case of an infant treated with vincristine and steroids.
Abbreviations: AS: Angiosarcomas; EHE: Epithelioid Hemangioendotheliomas; KHE: Kaposiform Hemangioendothelioma; MRI: Magnetic Resonance Image; mTOR: mammalian Target of Rapamycin
Introduction
Female, three months old, presented with a raised, hard, straight and reddish lesion of 3cm diameter, in upper region of right thigh, when she was 3 days old. The lesion was considered as a localized infection and the child received intravenous antibiotics for ten days. The skin lesion has increased, reaching the vulva, with purplish aspect and edges hyperemia. Laboratory examinations showed thrombocytopenia (6.000 platelets /mm3), hypofibrinogenemia and elevated D-dimer, which indicated thrombocytopenic coagulopathy. Doppler US of the right lower limb and Angio-MRI suggested vascular tumor. The combination of clinical findings, laboratory examinations and imaging findings led to the diagnosis of Kaposiform Hemangioendothelioma associated with the Kasabach Merritt Phenomenon. Biopsy was not attempted because of the potential risk for bleeding and death. Treatment with corticosteroids (prednisolone) was initiated. However, Vincristine (0.05 mg/ kg/week) was added at a weekly dose, due to persistent thrombocytopenia and increase of the lesion size. After two months, there has been complete regression of the lesion and progressive increase in the platelet count, until normalization. After three year follow up, no recurrence was detected (Figures 1 & 2).
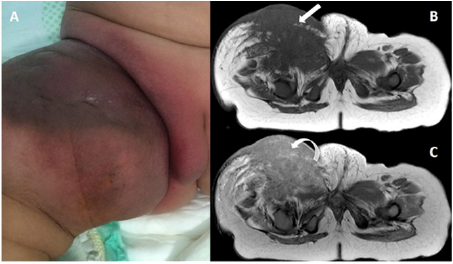
Figure 1:
a) Image of the expansive, purplish lesion, with imprecise limits, localization at the root of the right thigh.
b) Axial MRI images T1 show the extension to deep planes of the mass and its infiltrative aspect of imprecise limits (white arrow).
c) Diffuse and homogeneous enhancement (curved arrow) in T1 weighting after gadolinium.
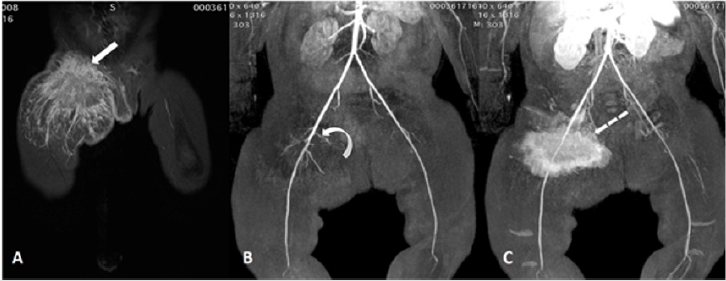
Figure 2: Magnetic Resonance Angiography.
a) Mass with hypersignal (white arrow) in STIR, with imprecise limits.
b) Tumor of vascular origin, concentration of small arterial branches (curved arrow) emerging from the right femoral artery, with enhancement in the late arterial phase by gadolinium (dotted arrow), with no larger venous drainage being observed.
Discussion
Current standard therapy for KHE includes several options such as surgery, chemotherapy, steroids, embolization, radiation therapy. There is no conclusive evidence of which is the best treatment strategy, and the decision should be made in a case-by-case basis [13]. Recent studies suggest that for cases where complete resection is not possible, the use of Vincristine or Sirolimus (rapamycin) would be the most suitable treatment alternatives [7]. Sirolimus, a mammalian Target of Rapamycin (mTOR) inhibitor, has been utilized to successfully treat vascular malformations. Schmid, et al. [7] has reported an efficacy on reduction of tumor size of 100% with Sirolimus in patients with KHE. Other authors have also described Sirolimus therapy as the best choice for these patients [5,6]. Nevertheless, the therapy with Sirolimus has been also associated with major side effects such as opportunistic agents pneumonia, not to mention other mild side effects [14,15]. On the other hand, Liu, et al. [16] published a meta-analysis which demonstrated a higher efficacy of VCR when compared to other treatment strategies [7,16]. These results have been supported by Wang et al., who reported a 70% rate of complete response in patients with KHE [2]. The side effects described with VCR were abdominal pain, loss of appetite, and elevations of ALT and AST, all classified grade [11,12,17]. Overall, it is noteworthy that both sirolimus and VCR have a high response rate in the treatment of KHE and KMP [11]. In this paper, we reported a clinical case of a patient who was treated with VCR in combination with prednisolone showing a complete response with no side effects. In our experience, and considering the current literature, this is an efficient and safe treatment strategy for KHE with KMP that should be considered as first line treatment, mainly in limited resources country, due to its low cost.
Conflict of Interest
We declare no conflict of interest.
References
- Zukerberg LR, Nickoloff BJ, Weiss SW (1993) Kaposiform hemangioendothelioma of infancy and childhood. An aggressive neoplasm associated with Kasabach-Merritt syndrome and lymphangiomatosis. Am J Surg Pathol 17(4): 321-328.
- Wang Z (2015) Steroid-resistant kaposiform hemangioendothelioma: a retrospective study of 37 patients treated with vincristine and long-term follow-up. Pediatr Blood Cancer 62(4): 577-580.
- Bsisu IK (2019) Bifocal Tibial Kaposiform Hemangioendothelioma Responsive to Vincristine Therapy: A Case Report. Am J Case Rep 20: 1923-1929.
- Ji Y (2018) Kaposiform haemangioendothelioma: clinical features, complications and risk factors for Kasabach-Merritt phenomenon. Br J Dermatol 179(2): 457-463.
- Jahnel J (2012) Kaposiform hemangioendothelioma with Kasabach-Merritt phenomenon: from vincristine to sirolimus. Klin Padiatr 224(6): 395-397.
- Cashell J (2018) Kaposiform hemangioendothelioma with Kasabach-Merritt phenomenon in an infant: Successful treatment with prednisolone, vincristine, and addition of sirolimus. Pediatr Blood Cancer 65(12): 27305.
- Schmid I (2018) Kaposiform hemangioendothelioma in children: a benign vascular tumor with multiple treatment options. World J Pediatr 14(4): 322-329.
- Gong X (2019) Ultrasonography and magnetic resonance imaging features of kaposiform hemangioendothelioma and tufted angioma. J Dermatol 46(10): 835-842.
- Tribolet S (2019) A not so harmless mass: Kaposiform hemangioendothelioma complicated by a Kasabach-Merritt phenomenon. Arch Pediatr 26(6): 365-369.
- Sparber Sauer M (2020) Endothelial cell malignancies in infants, children and adolescents: Treatment results of three Cooperative Weichteilsarkom Studiengruppe (CWS) trials and one registry. Pediatr Blood Cancer 67(3): e28095.
- Peng S (2019) Vincristine and sirolimus in the treatment of kaposiform haemangioendothelioma. J Paediatr Child Health 55(9): 1119-1124.
- Wang YJ (2012) Relationship between varicocele and sperm DNA damage and the effect of varicocele repair: a meta-analysis. Reprod Biomed Online 25(3): 307-314.
- Institute, N C Kaposiform Hemangioendothelioma.
- Ying H (2018) A Case Report of 2 Sirolimus-Related Deaths Among Infants with Kaposiform Hemangioendotheliomas. Pediatrics 141(5): S425-S429.
- Russell TB (2018) Pneumonia During Sirolimus Therapy for Kaposiform Hemangioendothelioma. Pediatrics 141(5): S421-S424.
- Liu X (2016) Clinical Outcomes for Systemic Corticosteroids Versus Vincristine in Treating Kaposiform Hemangioendothelioma and Tufted Angioma. Medicine (Baltimore) 95(20): e3431.
- Yao W (2019) Comparison of Corticosteroid and Vincristine in Treating Kaposiform Hemangioendothelioma and Tufted Angioma: A Systematic Review and Meta-Analysis. Eur J Pediatr Surg 29(5): 401-407.

 Case Report
Case Report