Abstract
Keywords: T2DM; Clinical Inertia; Opened Medical Team; Patient-centered Care
Opinion
T2DM is a common disease progressed over the long duration of life. Because of lacking apparent symptoms and signs in many cases, interrelationship between patient and doctor becomes complicated.
Process for Adjusting Blood Glucose
Both a patient and his(her) doctor cannot know his(her) disease state before blood A1C level is shown. His(her) prescription is determined by the A1C level at visit and evaluated by the A1C level of next visit. If patient reaches target A1C level determined by clinical guideline and has no hypoglycemic symptoms and signs, his(her) prescription is proposed to continue, and if not, is proposed to adjust. This process is repeated continuously unless patient disrupts to visit for any reason.
Origin of Clinical Inertia
If patient disagrees proposal for his(her) lifestyle or adjustment of oral blood-glucose lowering drugs, GLP1 analogues, or insulin derivatives, his(her) doctor will try either to recommend it, or to propose other choice. Negotiation begins between patient and his(her) doctor, and then his(her) prescription is determined. If next visit A1C level is not reached to target level, present prescription should be adjusted. But many patients do not like the change of prescription, especially when they want it by themselves. And the same prescription will be continued. From this time, clinical inertia [1] arises.
What Should We Do?
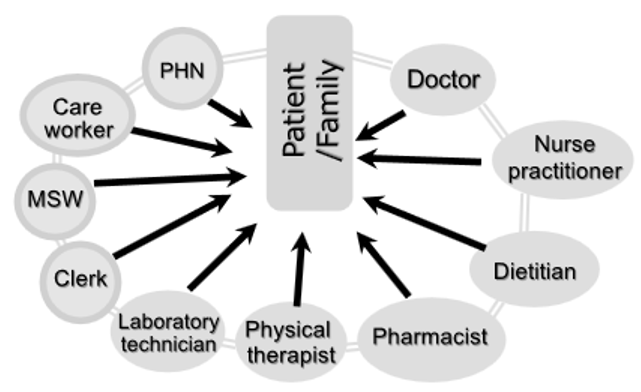
It is not impossible, but difficult, to break clinical inertia in the closed relationship between patient and his(her) doctor. Therefore, we should do organize medical team, which consists of patient him(her)self, his(her) doctor (general practitioner, diabetologist, if necessary, cardiologist, ophthalmologist, neurologist, nephrologist, dermatologist, orthopedic surgeon, etc.), diabetes educator (nurse practitioner, dietitian, pharmacist, physical therapist, and laboratory technician), other co-worker (clerk, medical social worker, care worker, public health nurse, etc.), and further his(her) family member(s). Opened relationship (Figure1) formed within this team would break clinical inertia.
Patient-Centered Care
If harmonized relationship, as had Steno-2 Study [2] shown, has developed, the medical team could provide patient-centered care [3] in T2DM.
Figure 1: Opened Medical Team: Nurse practitioner, dietitian, pharmacist, physical therapist, and laboratory technician belong to diabetes educator.
References
- Khunti K, Davies MJ (2017) Clinical inertia-Time to reappraise the terminology? Primary Care Diabetes 11(2): 105-106.
- Gæde P, Vedel P, Larsen N, Jensen GVH, Parving HH, et al. (2003) Multifactorial Intervention and Cardiovascular Disease in Patients with Type2 Diabetes. N Engl J Med 348(5): 383-393.
- (2017) NEJM Catalyst. What is Patient-Centered Care?

 Opinion
Opinion